Abstract
Purpose
Although few hepatectomy patients develop unexpected early diffuse and multinodular recurrence in the remnant liver, the prognosis in such cases is often dismal. The aim of this study was to evaluate the risk factors of early disseminated multinodular hepatocellular carcinoma (HCC) recurrence within 3 months after liver resection for solitary HCC.
Methods
Eighty-four patients who were diagnosed with recurrent HCC within 3 months after hepatectomy for solitary HCC were retrospectively reviewed. Disseminated HCC recurrence was defined as more than 10 tumors in both lobes and total tumor size >10 cm.
Results
Preoperative α-FP level, incidence of poor tumor grade, and presence of portal vein tumor thrombosis were higher in the patients with disseminated HCC recurrence than in those without disseminated HCC recurrence (P < 0.05). Multivariate analysis showed that α-FP >1,000 ng/dL was a predisposing factor of disseminated HCC recurrence within 3 months after liver resection. The overall survival rate for patients without disseminated HCC recurrence was higher than that for patients with disseminated HCC recurrence (P < 0.001).
Liver resection is a curative treatment method for solitary liver cancer [1]. However, only 9%–27% of patients with hepatocellular carcinoma (HCC) are eligible for surgical resection [2]. Although overall survival after resection of HCC has improved in recent years because improved surgical skills and postoperative management have led to a marked reduction in postoperative mortality rates. However, the recurrence of HCC after liver resection is a major surgical limitation because the recurrence rate remains high.
The pattern of recurrence after curative surgery for HCC is variable. Many hepatectomy patients developed intrahepatic recurrence [34]. Intrahepatic recurrence of HCC can be divided into cases with solitary or a few nodules and those with multinodular recurrence.
Early recurrence, defined as recurrence within 1 year of liver resection, is one of the most important factors affecting the prognosis and survival of patients with HCC [567]. Tumor size, intrahepatic metastasis, microvascular invasion, serum α-FP, serum proteins induced by vitamin K antagonist-II, C-reactive protein, and serum alkaline phosphatase have been reported as risk factors associated with early recurrence [48910]. Early recurrence of HCC in patients who undergo resection is still a controversial issue [11].
Few patients who undergo liver resection develop unexpected early diffuse and multinodular recurrence in the remnant liver at first visit within 3 months after hepatic resection. The prognosis is often dismal if it occurs. There might be no benefit of hepatic resection if the patient dies due to early disseminated multinodular HCC recurrence shortly after the surgery. Therefore, the risk factors of early disseminated multinodular HCC recurrence should be evaluated.
In this retrospective study, we evaluated and identified risk factors of early disseminated multinodular HCC recurrence within 3 months after liver resection in patients with recurrent HCC by analysis of preoperative and pathological factors.
This study included patients who underwent surgical resection of solitary HCC in Samsung Medical Center or Seoul National University Hospital based on preoperative radiological images between January 2005 and December 2011. HCC was confirmed from pathologic results after hepatectomy. We included patients with recurrent HCC patients after liver resection in 2 centers (n = 661). This study was approved by the Samsung Medical Center Institutional Review Board (IRB) (approval number: SMC 2013-05-013) and Seoul National University Hospital IRB (approval number: H-1303-061-474). Informed consent was exempted from the each IRB.
Inclusion criteria included primary curative resection, Child-Pugh class A, and HCC recurrence within 3 months after surgery. Exclusion criteria were as follows: mixed HCC and cholangiocarcinoma on pathology; age <18 years; non-Korean ethnicity; hepatic resection in recurrent HCC patients; Child-Pugh class B or C; multiple preoperative tumors based on preoperative radiologic images; ruptured HCC; R1 resection; extrahepatic metastasis or invasion; concurrent malignancy in other organs; history of malignancy other than HCC; previous locoregional therapies such as hepatectomy, radiation, transarterial chemoembolization (TACE), radiofrequency ablation (RFA), or percutaneous ethanol injection (PEI); intraoperative RFA; fibrolamellar HCC; or loss to follow-up after hepatectomy. Demographic, preoperative laboratory findings, and pathologic data collected from electronic medical records were retrospectively reviewed. None of the patients in either group received postoperative adjuvant therapy before recurrence.
Surgical and pathological procedures performed after liver resection have been described previously [34]. Liver function was evaluated using the Child-Pugh classification system. Adequate mobilization was achieved according to the part of the liver to be resected. Selective clamping of the portal vein and hepatic artery was performed when feasible. One center routinely used Pringle maneuver during liver resection, but the other center used Pringle maneuver whenever necessary. If operators thought much bleeding during hepatectomy, they used Pringle maneuver in those cases. Parenchymal transection was performed using a Cavitron Ultrasonic Surgical Aspirator or Kelly-clysis under low central venous pressure. Major hepatectomy was defined as the resection of ≥3 segments and minor hepatectomy was defined as the resection of <3 segments. Postoperative histological assessment and reporting included maximal tumor size, tumor grade, hemorrhage, necrosis, portal vein tumor thrombosis (PVTT), microvascular invasion, and intrahepatic metastasis. The histologic grade of HCC was assigned according to the Edmonson-Steiner system as well as differentiated (grade I), moderately differentiated (grade II), or poorly differentiated (grades III, IV) [12].
The procedures used for surveillance after liver resection have been described previously [8]. All patients were followed postoperatively one month. After then, all patients were followed every 2 or 3 months. Follow-up parameters were physical examination, serum α-FP, liver function tests, and chest x-rays. Abdominal CT was performed every 3 months or when recurrence was suspected. MRI and/or PET scans were performed if CT did not show definitive evidence of recurrence and tumor markers elevated. Disseminated HCC recurrence was defined as tumor number > 10 in both lobes and total tumor size >10 cm. Patients with intrahepatic recurrences were treated with RFA, TACE, liver resection, liver transplantation, or radiation according to functional liver reserve and the pattern of recurrence. Follow-up time was the length of time from surgery to the final follow-up or death.
All statistical analyses were performed using SPSS ver. 21.0 (SPSS, Inc., Chicago, IL, USA). Continuous variables are described as median with range. Categorical variables are expressed as number and percentage of subjects. Fisher exact test was conducted to evaluate differences in the frequencies of categorical variables between the groups. Mann-Whitney U analysis was conducted to evaluate the differences in continuous variables between the 2 groups. Binary logistic regression analysis was used to predict multinodular disseminated HCC recurrence within the first 3 months after liver resection. All tests were 2-sided, and statistical significance was defined as P <0.05.
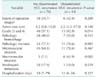
Eighty-four patients developed HCC recurrence within 3 months after liver resection. The baseline characteristics are summarized in Table 1. Disseminated HCC recurrence occurred in 14 patients (16.7%). There were no statistically significant differences in the sex, age, etiology for HCC, hemoglobin, platelet count, liver function tests, internal normalized ratio, indocyanine green value, or preoperative tumor size between the 2 groups. The preoperative median α-FP level was 6,295 ng/dL (range, 6.9–356,800 ng/dL) in the patients with disseminated HCC recurrence and 164 ng/dL (range, 1.9–157,310 ng/dL) in the patients without disseminated HCC recurrence (P = 0.013).
All patients had solitary nodule of HCC. The median tumor size was 5.5 cm (range, 2.2–17.0 cm) in the patients with disseminated HCC recurrence and 4.2 cm (range, 0.8–15.0 cm) in the patients without disseminated HCC recurrence (P = 0.140). The proportion of tumor grades 3 and 4 in the patients with disseminated HCC recurrence was 92.9% (n = 13), compared with 57.1% (n = 40) in the patients without disseminated HCC recurrence (P = 0.014). The incidence of PVTT was higher in the patients with disseminated HCC recurrence than in those without disseminated HCC recurrence (42.9% vs. 7.1%, P = 0.002). There were no statistically significant differences in extent of operation, tumor size, hemorrhage, necrosis, microvascular invasion, intrahepatic metastasis, or hospitalization between the 2 groups (Table 2).
The median follow-up duration was 9 months (range, 4–24 months) in the patients with disseminated HCC recurrence and 26 months (range, 4–101 months) in the patients without disseminated HCC recurrence (P < 0.001). At time of diagnosis of recurrent HCC, the median α-FP level was 9.385 ng/dL (range, 5.8–427,000 ng/dL) in the patients with disseminated HCC recurrence and 171 ng/dL (range, 1.7–200,000 ng/dL) in the patients without disseminated HCC recurrence (P = 0.002). Multivariate analysis showed that α-FP >1,000 ng/dL (odds ratio, 5.333; 95% confidence interval, 1.095–25.985; P = 0.038) was a predisposing factor of disseminated HCC recurrence within 3 months after liver resection. Treatments for recurrent HCC patients are summarized in Table 3.
The overall survival rate at 1-year was 38.9% in the patients with disseminated HCC recurrence and 84.8% in the patients without disseminated HCC recurrence. The overall survival for patients without disseminated HCC recurrence was higher than that for patients with disseminated HCC recurrence (P < 0.001) (Fig. 1).
The present study showed that the incidence of rapid and diffuse recurrent tumors after hepatectomy is associated with poor prognosis. Within the observation period, the mortality rates of patients with disseminated HCC recurrences (within 3 months of liver resection) were higher than those of patients without disseminated HCC recurrences. Among the 70 patients with early nondisseminated intrahepatic recurrences within 3 months after hepatectomy, 47 died within the observation period. In contrast, 11 patients of the 14 patients with early disseminated intrahepatic recurrence were dead within 2 years after hepatic resection as a result of advanced HCC.
In the remnant liver after hepatectomy, tumor recurrence is recognized as intrahepatic metastasis caused by dissemination of cells in the portal vein or metachronous multicentric hepatocarcinogenesis [345]. Patients with solitary or a few recurring nodules can be treated using several different modalities, including repeat liver resection, RFA, or liver transplantation, and have relatively high survival rates [1314]. However, among these diverse patterns of recurrence, disseminated multinodular intrahepatic recurrence is thought to be fatal not only because there is not amenable to effective treatment strategy, but also because their recurrent tumors are usually aggressive [215]. These recurrence patterns inevitably mean a short remaining survival time [2615].
If surgeons experience early disseminated multinodular HCC recurrence after liver resection in patients with solitary HCC, they can be disappointed and even embarrassed. However, the risk factors for early diffuse and multinodular recurrence within 3 months after liver resection are currently unclear. Risk factors for early disseminated multinodular intrahepatic recurrence after surgical resection may be reliable prognostic factors of long-term survival. Therefore, understanding the patterns and risk factors of early disseminated multinodular intrahepatic recurrence of HCC after hepatectomy will help clinicians to identify high-risk patients during the preoperative evaluation. The present study showed that α-FP >1,000 ng/dL was a predisposing factor of disseminated multinodular HCC recurrence within 3 months after hepatic resection in patients with recurrent HCC.
When recurrent HCC appears immediately after liver resection for HCC, it is generally thought that metastases of occult cancer cells that were not detected either grossly or by imaging techniques were already presented at the time of surgery. If these occult micrometastases could be detected in the preoperative evaluation stage, surgical resection of the main tumor may be contraindicated. However, current clinical technology does not allow preoperative determination of micrometastatic lesions; therefore, the best available approach at the present time is the determination of risk factors of immediate postoperative fatal recurrence.
Previous data have shown that high preoperative α-FP level is a significant risk factor of early postoperative recurrence [5,6]. The present study also revealed similar result that serum α-FP level > 1,000 ng/dL is significant a risk factor of early disseminated multinodular HCC recurrence after hepatic resection in patients with solitary HCC. Tumor cells may be probably already present in the remnant liver, together with microscopic portal invasion, before liver resection in patients with high α-FP level [7]. Another study has reported that the liver regeneration process after liver resection can enhance the growth of occult metastases, which rapidly develop into overt metastasis [16]. Therefore, efforts to predict these micrometastases and systemic dissemination of cancer cells should not be overlooked. Present study revealed that poor differentiated grade and microvascular invasion were closely associated with early multinodular disseminated recurrence by univariate analysis. Another study reported that those factors were considered as predictive factors for recurrence beyond Milan criteria after hepatic resection [17]. However, the present study did not demonstrate that vascular invasion was an independent risk factor related to early disseminated multinodular HCC recurrence by multivariate analysis.
Hepatectomy patients with risk factors such as increased preoperative α-FP levels, microvascular invasion, and poor differentiated grade had a dismal prognosis when early multinodular disseminated recurrence was developed after liver resection. Therefore, a possible strategy for improving patient survival may be early radiological evaluations within 2 weeks after surgery and early intervention.
This study has several limitations. First, the study is retrospective. Second, selection bias can occur due to inclusion of hepatectomy patients with preoperative radiologically solitary tumor and well-preserved liver function. Third, present study included only recurrent HCC patients after liver resection and excluded patients without HCC recurrence. Therefore, reports from other centers are also necessary to allow generalization of our findings.
In conclusion, early disseminated multinodular HCC recurrence was associated with poor survival after liver resection. Patients with α-FP >1,000 ng/dL in the preoperative period should be frequently evaluated for the early detection of recurrent HCC after hepatic resection. These findings indicate that the surgeon should explain the possibility of early disseminated multinodular HCC recurrence after surgery in patients with solitary HCC who have high serum α-FP level. If there is a possibility of disseminated HCC recurrence after surgery, sequential locoregional therapies first and surgery may be helpful.
Figures and Tables
References
1. Cherqui D, Laurent A, Mocellin N, Tayar C, Luciani A, Van Nhieu JT, et al. Liver resection for transplantable hepatocellular carcinoma: long-term survival and role of secondary liver transplantation. Ann Surg. 2009; 250:738–746.
2. Lee HY, Rhim H, Lee MW, Kim YS, Choi D, Park MJ, et al. Early diffuse recurrence of hepatocellular carcinoma after percutaneous radiofrequency ablation: analysis of risk factors. Eur Radiol. 2013; 23:190–197.

3. Kim JM, Kwon CH, Joh JW, Park JB, Lee JH, Kim SJ, et al. Outcomes after curative hepatectomy in patients with non-B non-C hepatocellular carcinoma and hepatitis B virus hepatocellular carcinoma from non-cirrhotic liver. J Surg Oncol. 2014; 110:976–981.

4. Kim JM, Kwon CH, Joh JW, Park JB, Lee JH, Kim SJ, et al. Differences between hepatocellular carcinoma and hepatitis B virus infection in patients with and without cirrhosis. Ann Surg Oncol. 2014; 21:458–465.

5. Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003; 38:200–207.

6. Kim BW, Kim YB, Wang HJ, Kim MW. Risk factors for immediate post-operative fatal recurrence after curative resection of hepatocellular carcinoma. World J Gastroenterol. 2006; 12:99–104.

7. Kamiyama T, Nakanishi K, Yokoo H, Kamachi H, Tahara M, Kakisaka T, et al. Analysis of the risk factors for early death due to disease recurrence or progression within 1 year after hepatectomy in patients with hepatocellular carcinoma. World J Surg Oncol. 2012; 10:107.

8. Kim JM, Kwon CH, Joh JW, Park JB, Ko JS, Lee JH, et al. The effect of alkaline phosphatase and intrahepatic metastases in large hepatocellular carcinoma. World J Surg Oncol. 2013; 11:40.

9. Kim JM, Kwon CH, Joh JW, Ko JS, Park JB, Lee JH, et al. C-reactive protein may be a prognostic factor in hepatocellular carcinoma with malignant portal vein invasion. World J Surg Oncol. 2013; 11:92.

10. Kim JM, Hyuck C, Kwon D, Joh JW, Lee JH, Paik SW, et al. Protein induced by vitamin K antagonist-II (PIVKA-II) is a reliable prognostic factor in small hepatocellular carcinoma. World J Surg. 2013; 37:1371–1378.

11. Yu SJ. A concise review of updated guidelines regarding the management of hepatocellular carcinoma around the world: 2010–2016. Clin Mol Hepatol. 2016; 22:7–17.

12. Edmondson HA, Steiner PE. Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer. 1954; 7:462–503.
13. Song KD, Lim HK, Rhim H, Lee MW, Kim YS, Lee WJ, et al. Repeated hepatic resection versus radiofrequency ablation for recurrent hepatocellular carcinoma after hepatic resection: a propensity score matching study. Radiology. 2015; 275:599–608.

14. Lee S, Hyuck David Kwon C, Man Kim J, Joh JW, Woon Paik S, Kim BW, et al. Time of hepatocellular carcinoma recurrence after liver resection and alpha-fetoprotein are important prognostic factors for salvage liver transplantation. Liver Transpl. 2014; 20:1057–1063.

15. Park JH, Koh KC, Choi MS, Lee JH, Yoo BC, Paik SW, et al. Analysis of risk factors associated with early multinodular recurrences after hepatic resection for hepatocellular carcinoma. Am J Surg. 2006; 192:29–33.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download