Abstract
Purpose
We aimed to compare skin closure techniques, standard (intermittent mattress) and continuous subcuticular sutures, following Limberg flap procedure.
Methods
From July 2013 to July 2015, 92 patients with sacrococcygeal pilonidal disease were prospectively randomized into 2 groups consisting of 46 patients for both. Patients underwent sinus excision and closure with Limberg flap; continuous subcuticular suture was used in subcuticular group (SG) and intermittent mattress sutures were used in mattress group (MG) for skin closure. Characteristics of patients, features of pilonidal disease, macerations, infections, wound dehiscence, flap necrosis, operation time, time of drain removal, wound complications, early recurrences, and time till return to work were compared between the 2 groups.
Results
There was no statistical difference between groups per sex, age, body mass index, smoking, number of sinuses, depth of intergluteal sulcus, distance of incision to anus, volume of extracted tissue, number of hair follicles per cm2, recurrence, operation, and mean follow-up time. Two patients showed signs of wound complications (4.4%) in SG, whereas 8 cases (17.4%) showed signs in MG (P < 0.05). One patient in SG had surgical site infection and required antibiotics (2.2%), where as there were 6 cases treated in MG (13.0%) (P < 0.05). Removal of drain tube, and time till return to work rates are lower for SG than MG (P < 0.05).
A pilonidal cyst, pilonidal sinus or sacrococcygeal pilonidal disease (SPD), occurs mostly at the intergluteal sulcus characterized by inflammation, abscess, or sinus formation. SPD commonly affects young adults with high incidence (26–700/100,000), and causes time and work loss [1].
Excision of the sinus and closure with flaps are considered popular treatment modalities. Long learning curves and operation times are commonly encountered. Postoperative macerations, infections and high rates of wound dehiscence may be seen. Even flap necrosis, which can be difficult to treat, may occur [2]. Therefore, the search for the ideal surgical treatment modality remains.
Removal of the sinus and closure with flaps are commonly applied in our country and clinic. Frequently seen complications are: skin macerations and local wound dehiscence (Fig. 1). Macerations almost always occurred over the suture line, between the needle entry points, in our daily practice. Intermittent mattress sutures might be a possible cause for maceration. Micro organisms may intrude easily through openings and, along with hairs, can cause early recurrences. Reducing the number of entry points with continuous subcuticular closure may be the solution to this condition.
In this present study, we aimed to compare skin closure techniques; standard (intermittent mattress) and continuous sub cuticular, following Limberg flap procedure, according to macerations, infections, wound dehiscence, and flap necrosis. Early discharge is one of our major concerns.
This prospective study was conducted in Dr. Lutfi Kirdar Kartal Research and Education Hospital bet ween July 2013 and July 2015. All patients were informed in detail preoperatively and informed consents were taken. Patients were computer-based randomized by an independent officer using patient admission numbers. Our study was approved by Dr. Lutfi Kirdar Kartal Research and Education Hospital ethics committee (approval number: 8951337/1009/152).
All patients complaining of SPD, which requires a surgical approach, were prospectively included in our study. Recurrences, continued infections, American Society of Anesthesiologists physical status classification III–IV cases, and involuntary patients were excluded.
All cases received epidural anesthesia. Prophylactic antibiotics were applied (Cefazoline 1 g/IV). After administration of anesthesia, prone Jackknife position was our preferred method. Hair removal was performed with clippers. A 1-cm2 area at the sacral site was marked and the number of hair follicles and depth of natal cleft was recorded. With the help of surgical bands gluteus was retracted and easy access to intergluteal sulcus was achieved. The surgical site was cleaned with polyvinyl iodine, at least three times. Additional sponge with iodine was applied to the anal opening to prevent contamination.
Preoperatively, 2-mL methylene blue was administered into the sinus opening. The diameter of pseudocysts and subcutaneous tracts were evaluated. The rhomboid incision was marked and applied keeping the sinus opening at the center. All tissues were removed and the sacrococcygeal fascia was prepared. Absence of diseased area plays major role in successful surgery. Meticulous control of hemostasis was done with the help of cautery. The horizontal angle of the ABCD parallel site was elongated with the help of a surgical incision on the gluteus, as far as BC site and, consequently, E point was reached (Fig. 2). Starting from this point with the help of another incision parallel to AD site, F point was reached. Incisions were deep enough to reach gluteal muscle fascia, and this fascia was released. The rhomboid flap was thus prepared. Surgical bands were removed. Transposition of the flap was achieved through approximation of FD points. A 12F suction drain was applied. Separate 2/0 polyglactin sutures were used for approximation of the fascia and subcutaneous tissue. Sacrococcygeal fascia was also included in these suture lines to prevent dead space.
3/0 polypropylene sutures were applied as mattress stitches in mattress group (MG), whereas 3/0 polyglactin sutures were used as continuous subcuticular sutures in subcuticular group (SG) for skin closure. Distance to anal area was recorded. Following irrigation with saline solution, wounds were cleaned with iodine and dressings were applied.
In the absence of any kind of complication all patients were discharged on the first day after surgery with drains. Ten days of leave of absence was applied to all cases. Drains were removed when the total amount was below 30 mL/day. Mattress sutures were removed on postoperative day 10. Wound cultures were obtained and a 5-day antibiotic regimen (ampicillin sulbactam) was applied in the presence of infection, without waiting for results, to prevent further wound complications (dehiscence, etc.). All cases were controlled on 3rd, 5th, 10th day, then 1st and 6th month. Follow-up controls were conducted over the phone. The visual analogue scale (VAS) scores (between 0 and 10) were recorded at days 1, 3, 5, 10, and 30. All cases were seen in outpatient clinics in the presence of discharge, bleeding, and itching.
In our present study maceration, discharge, dehiscence, and flap necrosis were considered wound complications within a 1-month period. Only final signs were recorded, even when multiple symptoms were seen. Maceration was recorded as softening and breaking down of the suture line. Surgical site infections were described as local redness, swelling, and purulent discharge, all in combination with suture lines.
Demographic data, body mass index (BMI), number of sinuses, distance of incision to anus, volume of extracted tissue, number of hair follicles per cm2, operation time, time of drain removal, wound complications, early recurrences, and finally time till return to work.
Statistical analysis was carried out using the IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). All statistical analyses were calculated with the help of chi-square for nonparametric values, whereas Student t-test was applied for evaluation of parametric values. Based on the results of the analyses, a P-value < 0.05 was considered as statistically significant.
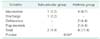
One hundred thirty-five patients received surgery for SPD. Forty-three cases were excluded for various reasons. Forty-six cases in MG and 46 cases in SG were included in our study. Seventy-five percent of patients were male with a mean age of 25.1 ± 8.8. There was no statistical difference between groups as per sex, age, BMI, smoking, number of sinuses, depth of intergluteal sulcus, distance of incision to anus, volume of extracted tissue, number of hair follicles per cm2, recurrence, operation, and mean follow-up time (Table 1). Drain tube removal day, wound complication, infection, antibiotic requirement, and time till return to work rates are lower for SG than MG (P < 0.05).
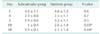
All patients were discharged on the first day after surgery. The shorter time to drain removal was statistically significant in SG (3.6 ± 1.3 days vs. 4.4 ± 1.5 days, P < 0.05). Two patients showed signs of wound complications (4.4%) in SG whereas there were 8 cases (17.4%) in MG (P < 0.05). One patient in SG had surgical site infection (2.2%), whereas 6 cases were treated therefor in MG (13.0%) (P < 0.05). No flap necrosis or complete wound dehiscence was detected in SG. Two cases in MG were admitted due to flap necrosis, and vacuum assisted closure therapy was applied. Distribution of wound complications per group are depicted in Table 2.
Requirement of antibiotics was evaluated. Only 1 patient was treated in SG (2.2%), whereas 6 cases needed antibiotics (13.0%) in MG (P < 0.05). Discontinuation of leave of absence was 10.8 ± 2.6 days in SG compared to 15.3 ± 6.2 days in MG (P < 0.001). After 6 months, only 1 patient showed signs of recurrence (2.2%) in SG. Two cases had recurrence in MG (4.4%) (P = 0.6).
There was no statistical significance between groups as per VAS scores on the 1st, 3rd, and 5th days. In contrast, VAS scores were lower in SG on the 10th day and first month (Table 3).
SPD is commonly encountered in specific countries. Initially, it was described by Herbert Mayo in 1883 as sinus containing hair. In 1880 Hodge proposed a new nomenclature and since then this clinical entity is addressed as pilonidal disease [3]. There is ongoing debate about the etiology. Formerly, the disease was considered as congenitally developed, while current studies are in favor of acquired [4]. Some risk factors were defined as puberty, hirsutism, obesity, deep intergluteal sulcus, and presence of hair follicles in natal cleft [56]. Contradictions in treatment modalities remain a major obstacle for successful treatment. Various methods of therapy can be found in the literature. A gold standard method of treatment is still missing. The ideal therapy should include a high success rate in healing, low risk of postoperative complications, low recurrence rates, decreased hospitalization time, absence of general anesthesia and shorter intervals till return to work [7]. None of the current treatment modalities covers these conditions. Time till return to work is longer due to delayed wound healing. Alternatively, wounds can be closed in the midline portion or beside it. Methods of primary closure shortens the healing process and time till return to work, whereas it is related with high risk of infection and recurrence [89]. Flaps are also commonly applied for closure in our current practice. Commonly used flaps are Karydakis and Limberg. Some authors compared various surgical flap techniques, though there was no statistical difference [1011]. In our study, we mainly focused on skin closure and suture techniques.
Limberg flap should close the defect and get rid of natal cleft depth. We attempted to achieve this goal in our current study. Removal of hair follicles from the midline and absence of pressure due to sitting remain major goal. Although it has only been applied for complex and recurrent cases, it is applied for all kinds of SPD in current practice [1213141516]. According to Horwood et al. [17], prospective randomized studies showed rates of surgical site infection between 2%–8%, whereas rates of wound dehiscence were between 0%–2% in comparison of primary closure with Limberg flap procedure. The same study showed low recurrence rates of between 0%–5.2%. Macerations following Limberg flap procedures may increase infection rates and delay healing. Kaya et al. [18] reported wound macerations at 8.5% in a study consisting of 94 patients. In our study, 2 macerations were seen on postoperative day 5 in SG group, whereas 8 cases were found in MG group. Initially, macerations lead to surgical site infections, flap necrosis and wound dehiscence at the final step. Our main goal was to prevent occurrence of macerations which lead to further complications. We believe that subcutaneous closure can reduce complications by reducing macerations. Our study findings were supportive of this idea.
We believe our current study is the first one where the application of intradermal subcuticular closure technique following Limberg flap procedure was utilized. Milone et al. [7] report that closure with intradermal suture encounters increased the rate of patient satisfaction and better cosmesis compared with transdermal sutures. In contrast, they used the primary midline closure technique. In this study, there was no statistical significance between groups as per surgical site infection, pain, daily activities, and time till return to work.
In our study, surgical site infection, requirement of antibiotic, maceration, and wound complications were detected in decreased numbers in SG. More so, drains were removed earlier and daily activities were achieved in shorter times. Also, time till return to work was short compared to MG. There was no statistical difference as per pain on days 1, 3, and 5, and recurrence.
There are certain limitations in our study. Since our study is the first one in the literature there is no other paper to attain power analysis to evaluate and describe patient numbers. Through evaluation of other pilonidal sinus studies, we believe that our number of cases is sufficient.
Additionally, we believe the absence of patient satisfaction and cosmesis evaluations remain major limitations. Future studies are needed to address this problem.
In conclusion, surgical procedures encountering Limberg flap method and subcuticular closure may reduce infection and maceration rates. Future studies are needed to provide detailed evaluation. Especially in our country, SPD is commonly seen.
Figures and Tables
Fig. 2
(A) Landmarks for Limberg flap. (B) Excision of sinus. (C) Approximation of fascia and subcutaneous tissue. (D) Closed wound with Limberg flap.

References
1. Can MF, Sevinc MM, Yilmaz M. Comparison of Karydakis flap reconstruction versus primary midline closure in sacroco ccygeal pilonidal disease: results of 200 military service members. Surg Today. 2009; 39:580–586.
2. Kaser SA, Zengaffinen R, Uhlmann M, Glaser C, Maurer CA. Primary wound closure with a Limberg flap vs. secondary wound healing after excision of a pilo nidal sinus: a multicentre randomised controlled study. Int J Colorectal Dis. 2015; 30:97–103.
3. Chintapatla S, Safarani N, Kumar S, Haboubi N. Sacrococcygeal pilonidal sinus: historical review, pathological insight and surgical options. Tech Coloproctol. 2003; 7:3–8.
4. Fazeli MS, Adel MG, Lebaschi AH. Com parison of outcomes in Z-plasty and delayed healing by secondary intention of the wound after excision of the sacral pilo nidal sinus: results of a randomized, clinical trial. Dis Colon Rectum. 2006; 49:1831–1836.
5. Cihan A, Ucan BH, Comert M, Cesur A, Cakmak GK, Tascilar O. Superiority of asym metric modified Limberg flap for sur gical treatment of pilonidal disease. Dis Colon Rectum. 2006; 49:244–249.
6. Akinci OF, Bozer M, Uzunkoy A, Duzgun SA, Coskun A. Incidence and aetiological fac tors in pilonidal sinus among Turkish soldiers. Eur J Surg. 1999; 165:339–342.
7. Milone M, Musella M, Maietta P, Bianco P, Taffuri C, Salvatore G, et al. Intradermal ab sor bable sutures to close pilonidal sinus wounds: a safe closure method? Surg Today. 2014; 44:1638–1642.
8. Khan PS, Hayat H, Hayat G. Limberg flap versus primary closure in the treatment of primary sacrococcygeal pilonidal disease; a randomized clinical trial. Indian J Surg. 2013; 75:192–194.

9. Dass TA, Zaz M, Rather A, Bari S. Elliptical exci sion with midline primary closure ver sus rhomboid excision with limberg flap reconstruction in sacrococcygeal piloni dal disease: a prospective, randomized study. Indian J Surg. 2012; 74:305–308.
10. Zorlu M, Sahiner IT, Zobacı E, Kocak C, Yastı AC, Dolapcı M. Early results with the Mutaf technique: a novel off-midline approach in pilonidal sinus surgery. Ann Surg Treat Res. 2016; 90:265–271.

11. Altintoprak F, Dikicier E, Arslan Y, Ozkececi T, Akbulut G, Dilek ON. Compa ri sion of the Limberg flap with the V-Y flap technique in the treatment of pilo nidal disease. J Korean Surg Soc. 2013; 85:63–67.
12. Tokac M, Dumlu EG, Aydin MS, Yalcın A, Kilic M. Comparison of modified Limberg flap and Karydakis flap operations in pilonidal sinus surgery: prospective randomized study. Int Surg. 2015; 100:870–877.

13. Altintoprak F, Gundogdu K, Ergonenc T, Dikicier E, Cakmak G, Celebi F. Retrospective review of pilonidal sinus patients with early discharge after Limberg flap procedure. Int Surg. 2014; 99:28–34.

14. Topgul K, Ozdemir E, Kilic K, Gokbayir H, Ferahkose Z. Long-term results of limberg flap procedure for treatment of pilonidal sinus: a report of 200 cases. Dis Colon Rectum. 2003; 46:1545–1548.
15. Cihan A, Mentes BB, Tatlicioglu E, Ozmen S, Leventoglu S, Ucan BH. Modified Limberg flap reconstruction compares favourably with primary repair for pilonidal sinus surgery. ANZ J Surg. 2004; 74:238–242.

16. Jamal A, Shamim M, Hashmi F, Qureshi MI. Open excision with secondary healing versus rhomboid excision with Limberg transposition flap in the management of sacrococcygeal pilonidal disease. J Pak Med Assoc. 2009; 59:157–160.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download