Abstract
Since multiport laparoscopic cholecystectomy has become a standard treatment for gallbladder (GB) disease, a single incision laparoscopic surgical technique has been tried to decrease the surgical site pain and achieve a better cosmetic out come in selected patients. The development of devices dedicated for single incision laparoscopic cholecystectomy (SILC) is expanding the indication of this single incision laparoscopic technique to more complicated GB diseases. Mirizzi syndrome (MS) is one of the complex uncommon gallstone diseases in patients undergoing cholecystectomy. Because the laparoscopic procedure has become a routine treatment for cholecystectomy, several studies have reported their experience with the laparoscopic technique for the treatment of MS with a comparable outcome in Csendes type I or II. Because the indication for SILC cholecystectomy is expanded to more complicated GB conditions, and the desire of patients for a less painful, better cosmetic surgical outcome has increased, our medical center used this single incision laparoscopic surgical technique for MS Csendes types I and II patients. Here, we report 2 successful cases of SILC for patients with MS types I and II without significant morbidity.
Since laparoscopic cholecystectomy was performed in 1985, this procedure has become a standard treatment for gallbladder (GB) disease over the last three decades. Laparoscopic cholecystectomy has traditionally been performed with multiple small port sites. The efforts to decrease the complication of multiple incisions and improve cosmesis have led to the development of a less invasive surgical technique, and single incision laparoscopic surgery has emerged as an alternative method to minimize complications associated with multiple incisions and to increase the satisfaction of the patients. Ever since Navarra et al. [1] published a report on a single skin incision laparoscopic cholecystectomy in 1997, this technique has been regarded as a safe and beneficial surgical methods to replace multiport laparoscopic cholecystectomy (MLC) in selected patients [2].
Initially, single incision laparoscopic cholecystectomy (SILC) was not indicated for patients with inflammatory GB dis ease such as acute cholecystitis, and GB empyema due to its limited range of maneuverability and possible safety concerns. However, the indication is now expanding after multiple centers have reported that single incision methods have shown comparable results in terms of safety and the complication rate with the conventional multiport laparoscopic procedure in more com plex GB diseases [3].
Mirizzi syndrome (MS) is one of the complicated uncommon gallstone diseases with a reported incidence between 0.06 and 5.7% in patients undergoing a cholecystectomy. It is defined as a benign common hepatic duct (CHD) obstruction due to gallstone impaction in the GB neck resulting in local inflammation and bile duct spasm. Bile duct wall necrosis and subsequent cholecystobiliary fistula caused by chronic inflammation are the sequence of the disease. MS was classified by McSherry et al. [4] in 1982 who described 2 types; type I includes partial or complete obstruction of the CHD due to external compression; type II refers to the formation of a communication between the GB neck or the cystic duct and the CHD. Csendes et al. [5] further distinguished the MS type II into 3 subtypes. In this classification, type II is a cholecystocholedochal fistula involving less than one-third of the diameter of the bile duct; type III, with the fistula involves two-thirds of the diameter; and type IV, with the fistula involves the complete bile duct. The treatment of MS is mainly surgical and consists of a partial or complete cholecystectomy with or without a common bile duct exploration. Shortly after the advent of laparoscopy in the treatment of GB disease, Rust et al. [6] suggested that MS may be a contraindication for laparoscopic cholecystectomy. In contrast, Paul et al. [7] reported the first successful laparoscopic treatment of type I MS in 1992 and several studies have reported the feasibility of the laparoscopic procedure for MS in Csendes types I and II [89].
Because the indication for a SILC cholecystectomy has expanded to include more complicated GB conditions, and the desire of patients for a less painful, better cosmetic surgical outcome has increased, our medical center used this single incision laparoscopic surgical technique in MS Csendes types I and II patients and we report here 2 successful cases of SILC for patients with MS Csendes types I and II without significant morbidity or mortality.
A 43-year-old male without any underlying disease visited a regional secondary hospital with back pain for 2–3 days. The initial laboratory results showed elevated liver enzymes and an increased total and direct bilirubin level. A CT scan was done and it was noticed that there was intra and extrahepatic duct dilatation. Under the diagnosis of a bile duct obstruction, an endoscopic retrograde cholangiopancreatography (ERCP) was performed. It showed that a GB stone 1.5 cm in size was impacted at the distal cystic duct compressing the CHD (Fig. 1A). Two endoscopic retrograde biliary drainage (ERBD) stents, a cholecystoduodenal and a hepatoduodenal, were placed to decompress the biliary tract before surgical treatment.
He was transferred to Seoul National Universitiy Bundang Hospital for further surgical management. MRCP was done one day after admission, and it showed that the impacted stone was compressing the CHD at the confluence of the CHD and the cystic duct (Fig. 1B). MS Csendes type II was diagnosed, and an operation was performed on the third day after the transfer.
A 3-cm transumbilical single incision was done. A single transparent Glove port (Nelis, Bucheoni, Korea) with 4 trocar sites and a scope holder, called the Laparostat (CIVCO, Coralville, IA, USA) was placed. To achieve a better surgical view, the fundus of the GB was lifted and fixed to the anterior peritoneum by temporarily sewing it. Due to severe adhesion around the GB, and the cystic and common bile duct, the antegrade technique of dissection from the fundus to the infundibulum was used. After meticulous dissection of the cystic and common bile duct, the cystic duct was incised at the proximal site of the stone impaction (Fig. 2A). The cholecystoduodenal stent and impacted stone were extracted, and the incision site was closed with an in situ suture using a V-Loc absorbable wound closure device (Covidien, New Haven, CT, USA) (Fig. 2B). The operating time was 142 minutes.
He developed fever up to 39.5℃ on postoperative day 4. The laboratory test showed leukocytosis (WBC, 14.0×103/µL). The patient underwent a CT scan, and it showed fluid collection at the cholecystectomy bed site. An image guided percutaneous drainage catheter was placed. Fever and leukocytosis were resolved by 2 days after the catheter placement. He was discharged on postoperative day 9 with a drainage catheter. The drainage catheter was removed during his second visit at the outpatient clinic after it was confirmed there was no residual fluid collection from the drainage tube. A hepatoduodenal stent was removed 1 month after his discharge.
A 66-year-old male who had a history of common bile duct stones, with post ERCP and CBD stone removal visited the Emergency Department with right upper quadrant pain for 5 days. The initial laboratory results included mild leukocytosis (WBC, 14.0×103/µL) and an elevated CRP level (10.6 mg/dL). ACT scan was performed, which showed acute cholecystitis and a cystic ductal stone compressing the CHD externally (Fig. 3). Under the diagnosis of acute cholecystitis with MS Csendes type I, he was admitted, and a percutaneous cholecystostomy was performed. After starting the decompression of the GB and antibiotics, the abdominal pain was resolved, and the laboratory results improved. He was discharged 7 days after his admission with a cholecystostomy drain and readmitted 2 weeks later followed by the operation on the next day.
A transumbilical single incision was done. A single port and scope holder were placed (Fig. 4). An antegrade dissection of the GB from the fundus to the infundibulum was performed. The cystic duct was dilated and adhered to the CHD. After careful dissection of the cystic duct from the CHD, the infundibulum was incised, and 8-mm stone was extracted (Fig. 5A). The cystic duct was ligated and resected with a 10-mm Hem-O-Lok clip (Teleflex Medical, Research Triangle Park, NC, USA) (Fig. 5B) and the specimen was extracted along with the cholecystostomy catheter together. The operating time was 84 minutes.
The patient was discharged on postoperative day 2 without any complications, and the follow-up laboratory results in the outpatient clinic showed all liver enzymes and the total bilirubin level within the normal range.
The informed consent was received by all patients for this manuscript.
Although Navarra et al. [1] first reported on SILC in 1997, it did not initially receive much attention. However, SILC has been rapidly adopted since 2009 with improvements to the platforms and devices specifically for SILC [10]. The excellent aesthetic outcome of SILC has been the driving force to not only use it in cholecystectomy procedures but also in other surgical procedures [11]. Especially, cholecystectomy is relatively easy to perform by the single incision laparoscopic technique because the surgical field is limited to the liver bed and the direction of the scopes and devices remains constant. The development of a scope holder could provide a more stable surgical view. By manipulating the scope in the direction an operator needs without having to struggle with instruments having a camera, this solo technique is starting to be regarded as the best combination with the single incision laparoscopic procedure [12].
One of the major concerns about SILC is a potential increase in the incidence of trocar site hernia postoperatively compared to the conventional multiport laparoscopic procedure. However, a recent study by Krajinovic et al. [13] showed there was no significant difference between SILC and conventional MLC in the incidence of trocar site hernia.
This anatomical benefit of applying a single incision laparoscopic technique to cholecystectomy and the development of devices specifically for SILC are contributing to its popularity by achieving comparable safety with that of conventional MLC [14]. The safety of SILC in more complicated GB disease such as acute cholecystitis has been reported by several studies [3].
Since SILC was introduced in our hospital in 2012, it has been performed only in selected patients during the initial period. From March 2014, we have used this technique for all available patients except for those with gall bladder cancer as we accumulated knowledge and standardized the technique. Currently, we are performing about 300 cases of SILC annually with a camera holder to achieve a stable surgical view and to overcome the insufficient single incised operating space under the lithotomy position of patients as our standardized protocol.
Our interim data of SILC for patients with acute cholecystitis showed no mortality and a postoperative complication rate of 5.2% which is comparable with the result of Ikumoto et al. (4.0%) [3]. The reason for the slightly higher rate of complication is probably because our institution is a specialized center for laparoscopic treatment. Many patients with complicated GB problems are referred to our hospital. According to our data on the characteristics of our patients using the updated Tokyo guidelines 2013 severity grading system for acute cholecystitis [15], the ratio of grade I/II was 0.64/0.36 and this high proportion of patients with grade II may explain this result. All of the complications were Clavien-Dindo classification IIIa or less, and all patients completely recovered from those complications.
MS is a rare disease that begins with a history of gallstones impacted in the neck of the GB or in the cystic duct. Due to the presence of a dense fibrotic process and/or communication bet ween the GB and the CHD, surgical management is not easy [16]. The surgical treatment of MS avoids a truly standardized approach and must be individualized depending on the stage of the disease and the expertise of the surgical team. However, some guidelines could be drawn and have been used during the last few years [17].
In MS classified as Csendes types I and II, a total or subtotal chole cystectomy is regarded as a standard treatment. Most cases of Csendes type III can be treated by a subtotal cholecystectomy leaving a flap of the GB wall to repair the bile duct. However, some cases with severe inflammation of the GB wall will need another procedure such as a hepaticojejunostomy. The treatment of MS type IV with extensive destruction of the bile duct wall consists of bilioenteric anastomosis. A hepaticojejunostomy Roux-en-Y is preferred. In contrast, in MS classified as Csendes types I and II, a total or subtotal chole cystectomy is regarded as a standard treatment.
Since the laparoscopic procedure has become a routine treatment of cholecystectomy, there have been several studies that described their experiences with the laparoscopic technique for the treatment of lesser severe types of MS. According to a systematic review by Antoniou et al. [16], the overall complication rate after a laparoscopic procedure for MS types I and II was 16% with residual stone and bile duct injury as the most common complications. Csendes et al. [5] who reported the second-largest available case series for the open treatment of MS in the literature, reported a procedural morbidity of 13.2%, excluding the rate of residual bile duct lithiasis. After excluding this complication from the rate of the recent analysis, the rate of complication after laparoscopic treatment of MS was 12%. Overall, the mortality rate was 0.8% after the laparoscopic procedure [18], and an in-hospital mortality of 1.8% was reported after the open procedure [5]. Lledó et al. [9] also have reported their experience over 7 years for treating MS during the laparoscopic era. They reported no postoperative mortality and a morbidity of 14.5%, which is comparable with open surgical management. Antoniou et al. [16] also emphasized that the most important predicting factor for the technical success of laparoscopic surgery for MS is the preoperative diagnosis. He reported a significantly decreased open conversion and complication rate in MS patients who were diagnosed preoperatively. Preoperative ERCP was recommended for patients with clinical suspicion of MS and intraoperative cholangiography is suggested if the diagnosis of MS is not made intraoperatively. In our cases, intraoperative cholangiography was not performed because MS was diagnosed preoperatively by ERCP or CT. Additionally, the cystic duct could be identified clearly during the surgical procedure without an intraoperative cholangiography.
Based on this comparable result of the laparoscopic approach for the treatment of MS type I or II, we used the single incision laparoscopic technique in these selected 2 patients. The SILC had acceptable results with no mortality and one case of morbidity which was resolved without sequelae.
In conclusion, it is still a challenge to use the single incision laparoscopic procedure in patients with complicated GB diseases. With antegrade dissection of the GB, a low threshold to open conversion, and careful patient selection, we were able to perform SILC in patients with MS Csendes types I and II.
Figures and Tables
Fig. 1
Preoperative image of patient. Endoscopic retrograde cholangiopancreatography (A) and magnetic resonance cholangiopancreatography (B) show a large stone which is impacted in the distal cystic duct at the confluence of common hepatic duct.
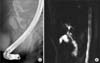
Fig. 2
Intraoperative view. Opening at the proximal site of impacted stone (A), closure of opened cystic duct after stone removal and cholecystectomy (B).

Fig. 3
Preoperative image of patient. CT scan shows a stone in the cystic duct which is compressing common hepatic duct externally.

References
1. Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997; 84:695.

2. Philipp SR, Miedema BW, Thaler K. Single-incision laparoscopic cholecystectomy using conventional instruments: early experience in comparison with the gold standard. J Am Coll Surg. 2009; 209:632–637.

3. Ikumoto T, Yamagishi H, Iwatate M, Sano Y, Kotaka M, Imai Y. Feasibility of single-incision laparoscopic cholecystectomy for acute cholecystitis. World J Gastrointest Endosc. 2015; 7:1327–1333.

4. McSherry CK, Ferstenberg H, Virshup M. The Mirizzi syndrome: surggested classification and surgical therapy. Surg Gastroentrol. 1982; 1:219–225.
5. Csendes A, Diaz JC, Burdiles P, Maluenda F, Nava O. Mirizzi syndrome and cholecystobiliary fistula: a unifying classification. Br J Surg. 1989; 76:1139–1143.

6. Rust KR, Clancy TV, Warren G, Mertesdorf J, Maxwell JG. Mirizzi's syndrome: a contraindication to coelioscopic cholecystectomy. J Laparoendosc Surg. 1991; 1:133–137.

7. Paul MG, Burris DG, McGuire AM, Thorfinnson HD, Schonekas H. Laparoscopic surgery in the treatment of Mirizzi's syndrome. J Laparoendosc Surg. 1992; 2:157–163.

8. Piccinni G, Sciusco A, De Luca GM, Gurrado A, Pasculli A, Testini M. Minimally invasive treatment of Mirizzi's syndrome: is there a safe way? Report of a case series. Ann Hepatol. 2014; 13:558–564.

9. Lledo JB, Barber SM, Ibanez JC, Torregrosa AG, Lopez-Andujar R. Update on the diagnosis and treatment of mirizzi syndrome in laparoscopic era: our experience in 7 years. Surg Laparosc Endosc Percutan Tech. 2014; 24:495–501.
10. Ito M, Asano Y, Horiguchi A, Shimizu T, Yamamoto T, Uyama I, et al. Cholecystectomy using single-incision laparoscopic surgery with a new SILS port. J Hepatobiliary Pancreat Sci. 2010; 17:688–691.

11. Tam YH, Pang KK, Tsui SY, Wong YS, Wong HY, Mou JW, et al. Laparoendoscopic single-site nephrectomy and heminephroureterectomy in children using standard laparoscopic setup versus conventional laparoscopy. Urology. 2013; 82:430–435.

12. Kalteis M, Pistrich R, Schimetta W, Polz W. Laparoscopic cholecystectomy as solo surgery with the aid of a robotic camera holder: a case-control study. Surg Laparosc Endosc Percutan Tech. 2007; 17:277–282.
13. Krajinovic K, Koeberlein C, Germer CT, Reibetanz J. The incidence of trocar site hernia after single-port laparoscopic chole cystectomy-a single center analysis and literature review. J Laparoendosc Adv Surg Tech A. 2016; 26:536–539.
14. Arezzo A, Scozzari G, Famiglietti F, Passera R, Morino M. Is single-incision laparoscopic cholecystectomy safe? Results of a systematic review and meta-analysis. Surg Endosc. 2013; 27:2293–2304.

15. Yamashita Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, et al. TG13 surgical management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2013; 20:89–96.
16. Antoniou SA, Antoniou GA, Makridis C. Laparoscopic treatment of Mirizzi syndrome: a systematic review. Surg Endosc. 2010; 24:33–39.

17. Beltran MA. Mirizzi syndrome: history, current knowledge and proposal of a simplified classification. World J Gastroenterol. 2012; 18:4639–4650.
18. Sare M, Gurer S, Taskin V, Aladag M, Hilmioglu F, Gurel M. Mirizzi syndrome: choice of surgical procedure in the laparoscopic era. Surg Laparosc Endosc. 1998; 8:63–67.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download