Abstract
Small bowel lymphangioma is a rare benign tumor of the lymphatic system, characterized by the presence of dilated lymphatic spaces and significant gastrointestinal bleeding. Small bowel lymphangiomas are rare in adults and case reports are few. Lymphangiomas in the jejunum or ileum are extremely rare and account for less than 1% of all lymphangiomas. The case reported herein is of an older patient (70-year-old male) with melena and chronic anemia (hemoglobin count < 5 g/dL) who had small-sized multiple lymphangiomas in his small bowel (jejunum). Surgical resection was performed after failure of treatment by gastroenteroscopy. Final pathological analysis revealed lymphangioma with thrombus and hemorrhage. After surgery, he no longer had decreased hemoglobin count, nor symptoms of anemia and melena. Also, at the last follow-up visit, the patient's hemoglobin count patient was normal and he returned to normal daily functions.
Small bowel lymphangioma is a rare benign tumor of the lymphatic system, characterized by the presence of dilated lymphatic spaces and significant gastrointestinal bleeding [1]. Lymphangioma lesions are generally located in the head and neck region and the axilla, rarely developing intra-abdominally. The most common locations for lymphangiomas of the intra-abdominal cavity are the mesentery, omentum, mesocolon, and retroperitoneum [2]. The diagnosis of a lymphangioma in the small bowel is very difficult preoperatively, even if biopsy is performed by gastroenteroscopy. Small bowel lymphangiomas are rare in adults and published case reports are few in number. The patient reported here had an unusual case of multiple lymphangiomas in the small bowel, presenting as chronic anemic symptoms in an adult.
A 70-year-old South Korean man was admitted presenting with anemia, dizziness, and intermittent melena. He had a history of iron deficiency anemia beginning 3 years prior. He had been admitted to hospital 4 times over the past 3 years because of anemia (hemoglobin count < 5 g/dL) and melena, and he had undergone transfusion with packed RBCs. He had undergone a clipping of a hemangioma on the duodenum by gastroenteroscopy 1 year previously. Laboratory testing revealed a white blood cell count of 5,500 cells/mm3 and a hemoglobin count of 5.2 g/dL. Other routine lab tests revealed no specific findings. His clinical symptoms were dizziness, general weakness, and melena. A video capsule endoscopy was performed and revealed mucosal erosion with a blood clot at the jejunum (at about 60–70 cm distal to the ligament of Treitz) (Fig. 1). Gastroenteroscopy revealed multiple polypoid masses, with bleeding, in the long segment of the jejunum. Histology from endoscopic biopsies did not provide a conclusive diagnosis but revealed a chronic inflammation pattern with lymphangiectasia.
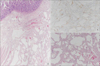
The patient underwent repeated gastroendoscopy (4 times) for bleeding control by clipping due to low his hemoglobin count and chronic bleeding (Fig. 2). However, his symptoms did not improve. He continued to show chronic anemia and melena even after bleeding control by gastroendoscopy. He underwent segmental resection of the long segment of the jejunum (about 70 cm) that had been marked (tattooing) previously during gastroendoscopy. The intraoperative finding was not remarkable except for the tattoo and no palpable masses. Macroscopically, the mucosal surface showed multifocal erosions, and multiple bright yellow-white submucosal lesions were observed in the resected jejunum (Fig. 3). Histologically, numerous dilated lymphatics were identified in the submucosa by hematoxylin and eosin (H&E) staining. The lymphatics were positive for D2-40, based on immunohistochemical staining (Fig. 4). The final pathological analysis was consistent with lymphangioma with thrombus and hemorrhage. After surgery, the patient no longer experienced drops in hemoglobin count or symptoms of anemia and melena. At the last follow-up visit (after 3 months), his hemoglobin count was normal (10.4 g/dL) and he was living a normal life. He then visited the outpatient clinic for hypertension on February, 2017 (6 months after surgery). His hemoglobin count was 12.9 g/dL and he had no symptoms.
Ethical approval was not necessary as this case report was based on retrospective review.
Lymphangiomas are rare lymphatic system tumors and represent 6% of small bowel tumors found in children and 1.4%–2.4% of those tumors in adults [3]. Approximately 60% of patients with lymphangiomas are younger than 5 years; however, a significant number of abdominal lymphangiomas do not manifest until adulthood [3]. The common sites of lymphangiomas are the head, neck, and axillary regions. Tumors at other locations, such as the abdominal or mediastinal cavity, are rare and account for approximately 5% of all lymphangiomas [24]. Among these, lymphangiomas of the small bowel are very rare, and lymphangiomas in the jejunum or ileum are extremely rare, accounting for less than 1% of all lymphangiomas [3]. A literature review of studies on lymphangiomas revealed that only 19 cases of small bowel lymphangioma were reported from 1960 to 2009 [5]. Similarly, small bowl lymphangiomas with gastrointestinal bleeding were reported in only 15 cases from 1967 to 2012 [6]. Two recent case reports of small bowel lymphangioma were published: one, reported in 2014, was a 24-year-old woman with clinical presentation of iron deficiency anemia who had a lymphangioma in the second portion of the duodenum [7]; the other case report, published in 2015, was a 28-year-old man with melena and anemia who had a lymphangioma in the third duodenal segment [8]. The present case is an elderly patient with melena and clinical presentation of iron deficiency anemia who had a lymphangioma in the long segment of the jejunum.
The clinical presentation of lymphangioma is unspecific and often presents with nausea, vomiting, and abdominal discomfort or pain. Other symptoms of lymphangioma are acute or chronic hemorrhage, infection, perforation, intussusceptions, torsion, rupture, and protein-losing gastroenteropathy [8]. The most common complications of lymphangioma are spontaneous or traumatic bleeding, hemorrhage, rupture and infection [9]. Histologically, lymphangioma consist of blood vessels and lymphatic channels of various sizes. The pathogenesis of spontaneous hemorrhage of lymphangioma is unknown. The present case had symptoms of chronic hemorrhage, dizziness, and melena. Diagnosis of small bowel lymphangioma is difficult and requires pathological confirmation of the lesion. Histopathological examination of lymphangioma demonstrates dilated lymphatic vessels and space by H&E staining and positive D2-40 immunohistochemical staining [789]. The size and number of lymphangiomas varies. One case report published in 2012 described a single lesion 5.0 cm × 4.0 cm in size in the duodenum [10]. The present case involved multiple small-sized lesions (<10 mm) in the long segment of the jejunum.
The first-line treatment of small bowel lymphangiomas is bleeding control by gastroenteroscopy or double-balloon enteroscopy [6]. Surgery is necessary when bleeding control by gastroenteroscopy fails. Surgical segmental resection of the bowel, including the lesion, is the optimal treatment for avoiding recurrence (Table 1). Our patient underwent surgical resection of a small bowel segment including the lesion.
Figures and Tables
Fig. 1
Video capsule endoscopy revealed mucosal erosion (A) with blood clot at jejunum (B) (at about 60 cm distal to the ligament of Treitz).

Fig. 2
Gastroendoscopy revealed mucosal erosions (A) on jejunum and performed bleeding control (C) by clipping due to chronic bleeding (B–D).

Fig. 3
Macroscopically, (A) the mucosal surface was showed multifocal erosion (A) and some bright yellow-white multiple submucosal lesions are observed in specimen (resected jejunum) (B).

References
1. Gerosa Y, Bernard B, Lagneau M, You K, Hoang C, Brasseur JL, et al. Cystic lymphangioma of the duodenum revealed by digestive hemorrhage and associated with exudative enteropathy. Gastroenterol Clin Biol. 1993; 17:591–593.
2. Enzinger FM, Weiss SW. Tumors of lymph vessels. In : Enzinger FM, Weiss SW, editors. Soft tissue tumors. 3rd ed. St. Louis(MO): Mosby;1995. p. 679–99.
3. Suthiwartnarueput W, Kiatipunsodsai S, Kwankua A, Chaumrattanakul U. Lymphangioma of the small bowel mesentery: a case report and review of the literature. World J Gastroenterol. 2012; 18:6328–6332.

4. Jang JH, Lee SL, Ku YM, An CH, Chang ED. Small bowel volvulus induced by mesenteric lymphangioma in an adult: a case report. Korean J Radiol. 2009; 10:319–322.

5. Morris-Stiff G, Falk GA, El-Hayek K, Vargo J, Bronner M, Vogt DP. Jejunal cavernous lymphangioma. BMJ Case Rep. 2011; 05. 12. pii: bcr0320114022. DOI: 10.1136/bcr.03.2011.4022.

6. Kida A, Matsuda K, Hirai S, Shimatani A, Horita Y, Hiramatsu K, et al. A pedunculated polyp-shaped small-bowel lymphangioma causing gastrointestinal bleeding and treated by double-balloon enteroscopy. World J Gastroenterol. 2012; 18:4798–4800.

7. Antonino A, Gragnano E, Sangiuliano N, Rosato A, Maglio M, De Palma M. A very rare case of duodenal hemolymphangioma presenting with iron deficiency anemia. Int J Surg Case Rep. 2014; 5:118–121.

8. Bucciero F, Marsico M, Galli A, Tarocchi M. Small bowel lymphangioma: a rare case of intestinal bleeding. Dig Liver Dis. 2015; 47:815.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download