Abstract
Background and Objectives
Although many studies have assessed factors related to adherence of PAP therapy, there were no studies about factors related to doctors or device managers. The purpose of this study was to investigate the relationship between PAP therapy adherence and doctor or device manager.
Subjects and Methods
Between February 2013 and June 2015, 163 patients newly diagnosed with moderate to severe OSA in one of five hospitals were enrolled in this study. All patients received 4 weeks of PAP treatment with intervention consisting of mechanical support and motivation by doctor and device manager. Data from the PAP device were obtained following a minimum of an initial 30 days, with adherence defined as >4 h/night on 70% of nights.
Results
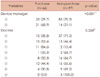
After 30 days, total adherence rate to PAP therapy was 35.6% (n=58). The adherence rate of device manager ① was 26.3% (31/118), and that of device manager ② was 60% (27/45), and there was statistically significant difference between the two device managers. Furthermore, there were statistically significant differences in the adherence to PAP therapy ranging from 85.6% to 0.0% according to doctor.
Figures and Tables
Acknowledgments
This work was supported by the year 2018 clinical research grant from Pusan National University Hospital.
References
1. Lee SM, Lee YJ, Kim HJ. Common side effects and compliance with nasal continuous positive airway pressure in Korean OSA patients: short-term follow up. J Korean Sleep Res Soc. 2010; 7:1–7.

2. Kim HY, Jang MS. Improving compliance for continuous positive airway pressure compliance and possible influencing factors. Korean J Otorhinolaryngol-Head Neck Surg. 2014; 57:7–14.

3. Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009; 5:263–276.
4. Hoffstein V. Review of oral appliances for treatment of sleep-disordered breathing. Sleep Breath. 2007; 11:1–22.

5. Ballester E, Badia JR, Hernández L, Carrasco E, de Pablo J, Fornas C, et al. Evidence of the effectiveness of continuous positive airway pressure in the treatment of sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1999; 159:495–501.

6. Loube DI, Gay PC, Strohl KP, Pack AI, White DP, Collop NA. Indications for positive airway pressure treatment of adult obstructive sleep apnea patients: a consensus statement. Chest. 1999; 115:863–866.

7. Marshall NS, Barnes M, Travier N, Campbell AJ, Pierce RJ, McEvoy RD, et al. Continuous positive airway pressure reduces daytime sleepiness in mild to moderate obstructive sleep apnoea: a meta-analysis. Thorax. 2006; 61:430–434.

8. Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath. 2010; 14:323–335.

9. Dhillon S, Chung SA, Fargher T, Huterer N, Shapiro CM. Sleep apnea, hypertension, and the effects of continuous positive airway pressure. Am J Hypertens. 2005; 18:594–600.

10. Smith SS, Lang CP, Sullivan KA, Warren J. A preliminary investigation of the effectiveness of a sleep apnea education program. J Psychosom Res. 2004; 56:245–249.

11. Han EK, Yoon IY, Chung S. The compliance and effect of CPAP in obstructive sleep apnea syndrome. Sleep Med Psychophysiol. 2006; 13:52–58.
12. Choi JB, Lee SH, Jeong DU. Compliance of nasal continuous positive airway pressure in patients with obstructive sleep apnea syndrome. Sleep Med Psychophysiol. 2006; 13:27–32.
13. Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993; 147:887–895.

14. Lutfey KE, Wishner WJ. Beyond “compliance” is “adherence”. Improving the prospect of diabetes care. Diabetes Care. 1999; 22:635–639.

15. Choi J, Cho SH. Treatment of obstructive sleep apnea with positive pressure ventilation. Hanyang Med Rev. 2013; 33:239–245.

16. Kim MJ, Kim MJ, Bae SH, Park CH, Kim DK. Predictors of adherence with positive airway pressure treatment in patients with obstructive sleep apnea in Korean. J Rhinol. 2015; 22:89–95.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download