Abstract
Purpose
This study is performed to evaluate the usefulness of arthroscopic surgery prior to open reduction and fixation surgery to treat acetabular fractures and hip fractures-dislocation.
Materials and Methods
From January 2010 to March 2014, a total of 54 patients with acetabular fractures or hip fractures with dislocation were treated arthroscopically via fracture surface before open reduction and fixation (group 1, n=11), and without hip arthroscopy prior to open reduction and fixation (group 2; n=43). Clinical results were evaluated using Harris hip score (HHS) and visual analogue scale (VAS) pain scores.
Results
The mean age of patients is 43.2 years and there are 10 males and 1 females in group 1. The mean follow-up period is 15 months. The acetabular status of each case was assessed arthroscopically. Bone fragment was performed in 6 cases, and ligamentum teres shrinkage in 1 case. At the final follow up, the mean HHS and VAS pain scores were 78.6 and 2.18, respectively. During follow up, one case of osteoarthritis and one case of heterotopic ossification were identified. At the final follow up, the mean HHS and VAS pain scores were 77.5 and 2.23, respectively. In group 2, oteoarthritis and ectopic ossification were observed in 4 and 1 cases, respectively.
Conclusion
No differences were observed in the clinical outcomes of patients with acetabular fracture or hip fracture-dislocation when treated with or without arthroscopic surgery before open reduction and fixation. However, arthroscopy is thought to be useful for evaluating the joint cartilage surface and fracture fragments more accurately.
Acetabular fractures and hip fractures-dislocation are common and inherently affected the stability of hip joint bones. These events can be caused by high-energy traumas (e.g., traffic accidents) and often accompany other injuries. Early orthopedic intervention is essential for improved prognosis of hip fracture-dislocation. Precisely quantifying the level of injury is critical, and although physical and radiographic examinations are extremely useful, assessments using these approaches may vary from surgical findings because they are limited by the anatomical nature (i.e., depth) of the hip joint.
Hip arthroscopy has been used to diagnose and treat intraarticular lesions (e.g., acetabular labral tears, femoroacetabular impingement), and the indications for the procedure have broadened based on its ability to provide a clear view of the ligamentum teres, synovium, acetabular labrum, femoral head and acetabular cartilage1). However, hip arthroscopy indications after a hip fracture have not yet been clearly defined2).
Since intra-articular loose bodies (e.g., bone fragments) may cause degenerative changes, arthroscopic loose body removal and other procedures are required3). Conventionally, loose bodies can be removed with arthroscopy after internal fixation of a fractured hip, but patients may experience discomfort undergoing at least two surgical procedures. This study aims to characterize the effectiveness of hip arthroscopy prior to open reduction and internal fixation.
Here, we report on a retrospective analysis of 54 patients with acetabular fracture or hip fracture-dislocation treated between January 2010 and March 2014 with a minimum of 1 year follow up. Of these, 11 (group 1) were treated with hip arthroscopy via fracture surface before open reduction (Fig. 1, 2). Their mean age was 43.2 years (range, 23–68 years), and there were 10 males and 1 female. The mean follow-up duration was 15 months (range, 12–25 months). There were 1 case with acetabular fracture and 10 cases with fracture-dislocation. According to the Thomson-Epstein classification system, patients were type I (n=0), type II (n=4), type III (n=2), 3 type VI (n=3), and type V (n=1). Meanwhile, 43 patients (group 2) did not undergo hip arthroscopy. Their mean age was 50.1 years (range, 26–68 years), and there were 39 males and 4 females. The mean follow-up duration was 18.4 months (range, 12–39 months). Preoperative computed tomography (CT) scan was done in all patients. The presence of intra-articular fragments and the shape of the intra-articular fracture line were examined.
All operations were performed in the lateral position and the supine position. Patients in group 1 were treated with open reduction and internal fixation through the Kocher- Langenbeck approach (n=9), the ilioinguinal approach combined with Kocher-Langenbeck approach (n=1), and osteotomy of the greater trochanter (n=1). Patients in group 2 were treated with open reduction and internal fixation through the Kocher-Langenbeck approach (n=38) and the ilioinguinal approach combined with Kocher-Langenbeck approach (n=5). Arthroscopy was performed through an incision made for internal fixation of the fracture without making an additional endoscopic portal. In each approach, the joint space was secured through manual traction after exposure of the joint capsule and then 30° and 70° arthroscopes were inserted to evaluate intra-articular lesions. Arthroscopy was performed before internal fixation via fracture surface and space formed after dislocation, and reduction and internal fixation were carried out after removal of loose bodies such as fracture fragments, debridement of the labral tissue and soft tissue, removal and irrigation of hematoma (Fig. 3, 4). To obtain a surgical view of arthroscopy, consistent fluid supply using the arthroscopic pump and suction use were maintained. Subsequently, open reduction and internal fixation were performed (Fig. 5, 6). The arthroscopic pump pressure was maintained at 50 mmHg. To prevent extra-articular extravasation of fluid during arthroscopy, suction was consistently used.
Patients were put on bed rest during the first postoperative week. According to the status of fracture healing, partial weight bearing was progressively allowed using a wheelchair, crutches or other ambulation aids depending on the results of radiographic follow-up examination after non-weight bearing at least for 4 weeks. Age, sex, body mass index (BMI), intraoperative bleeding, operating time, and preoperative VAS scores were compared between the two groups. Clinical assessments were made using the Harris hip score (HHS) and VAS pain score. Radiological assessments included anterior, oblique, inlet and outlet views of the pelvis on simple radiographs, joint congruency of the acetabulum on CT scans, and evaluation of fracture-reduction statuses. Radiological evaluations performed 12 months after surgery confirmed bone union and the presence or absence of traumatic arthritis and heterotopic ossification. All statistical analyses were performed using the SPSS software package (IBM SPSS ver. 22.0; IBM Co. Armonk, NY, USA). The Mann-Whitney U-test was used to test differences. P-values of less than 0.05 were considered statistically significant.
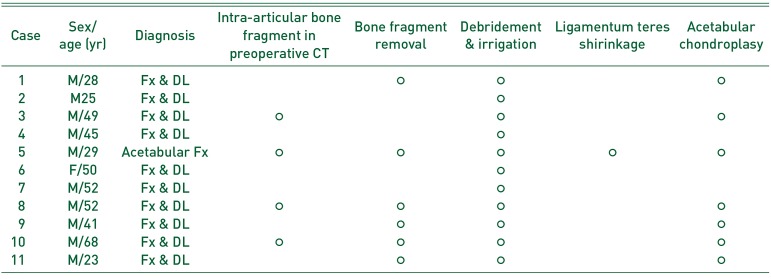
As shown in Table 1, no statistically significant differences were observed between the baseline demographics of groups 1 and 2 (i.e., age, sex, BMI intraoperative bleeding, operating time and preoperative VAS scores). The mean duration of hip arthroscopy was 40.8 minutes (range, 28–51 minutes). At the final follow-up, HHS and VAS pain scores of group 1 were 78.6 and 2.18, respectively, compared with 77.5 and 2.23 in group 2. In group 1, the overall acetabular status was shown by hip arthroscopy in all cases and debridement was conducted due to cartilage lesions and partial tears of the labrum in all patients. Preoperative CT findings revealed intra-articular fragments in 4 cases, but removal of the bone fragment was performed in 6 cases (Table 2). The fragments were thought to be caused by injury to the acetabular cartilage, but there were more cases not identified with the origin of fragments. Injury was greater than International Cartilage Repair Society grade 3. Thermal shrinkage was performed in 1 case with partial tear of the ligamentum teres. Complete tears were observed in most cases, excluding 2 cases with unknown state. Unlike conventional hip arthroscopy techniques, this is thought to be because we had the risk of iatrogenic injury at the fracture site due to excessive manipulation of arthroscopy via fracture surface to improve the operative view.
Complete bone union was observed within 16 weeks after surgery in all group 1 patients. Postoperative complications included osteoarthritis (n=1) and heterotopic ossification (n=1). There were no specific complications associated with arthroscopy (e.g., iatrogenic articular cartilage injury, extra-articular extravasation). No patients underwent a second arthroscopy during follow-up. Chondroplasty was performed in 7 cases with injuries to the acetabular cartilage accessible for the arthroscopic procedure. Total hip arthroplasty was conducted in one patient with osteoarthritis as secondary surgery (Fig. 7); this patient was also monitored with magnetic resonance imaging during the first postoperative year after fracture.
The average time to fracture union was 15.4 months (range, 12–20 months) at the follow-up after surgery in group 2. Postoperative complications included osteoarthritis (n=4) and heterotopic ossification (n=1). Of the 4 cases with osteoarthritis, 3 patients underwent total hip arthroplasty and 1 patient is currently under follow-up.
Hip arthroscopy was first introduced in 1931 by Burman; however, its clinical application and usefulness went unmentioned until the 1970s. This procedure has been used for the diagnosis and treatment of hip disease intermittently since the 1980s. Hip arthroscopy is limited by: i) difficulty with gaining arthroscopic access due to the deep location and thick bands of tissue of the hip joint, ii) required traction devices, and iii) other technical challenges. However, with recent advances in surgical methods and instruments, hip arthroscopy is being used more readily than ever before. Indications for hip arthroscopy vary slightly depending on authors, but commonly include, but are not limited to: i) diagnosis of patients complaining of hip pain, ii) diagnosis and treatment of labral tears, iii) removal of loose bodies, iv) diagnosis and treatment of cartilage injuries, pyogenic arthritis, extra-articular injuries, and femoroacetabular impingements. In recent years, there has been a gradual trend toward the increased use of second-look arthroscopic surgeries4567). Hwang et al.8) reported chronic impingement, insufficient repair of labral tear and postoperative labral adhesion as the leading causes for hip pain persisting despite arthroscopic surgical repair of labral tears. Lim et al.9) achieved favorable surgical outcomes without any arthritis or avascular necrosis in arthroscopic hip surgery with a follow-up of 9 months after open surgical intervention of the femoral head severely injured after hip fracture-dislocation. Post-reduction arthroscopic hip surgery was shown to be most useful in the treatment of hip fracture-dislocations. However, this intervention is limited as it is a sequential surgery performed under general anesthesia. Additionally, removal of fracture fragments is reliant on the ability to achieve proper acetabular visualization during open reduction. On the other hand, hip arthroscopy can reveal lesions that are not detected in a surgical view. In this study, several limitations in our evaluation of the hip joint were unavoidable since we performed hip arthroscopy through the fracture site before open reduction instead of the common approach to the hip joint via anterior and anterolateral portals. Excessive arthroscopic manipulation to obtain a better surgical view may cause injury to the fractured area. Since our procedure provides a different arthroscopic view compared with conventional hip arthroscopy techniques, accurate understanding of the surgical anatomy is difficult and anatomical deformities caused by the fracture makes it even more challenging. Nevertheless, we were able to detect and remove fracture fragments unseen in the surgical view and access to acetabular cartilage lesions to some extent.
Hwang et al.10) suggested arthroscopic hip surgery to remove loose bodies and incarcerated acetabular laburm following reduction in patients with traumatic hip dislocation. Kim et al.11) documented the entrapment of the labrum into the articular surface after reduction of hip dislocation. We detected labral tears in all cases and performed debridement and thermal shrinkage. According to Hwang et al.12), patient symptoms improved after second-look hip arthroscopy and clinical outcomes were good, with osteoarthritis observed during follow-ups. However, in this study, we observed no differences in clinical results between the two groups (i.e., those treated with or without hip arthroscopy). Progressive osteoarthritis was observed in one patient in group 1 treated with hip arthroscopy, and appeared to be the result of severe damage on the femoral head and acetabular cartilage at the time of injury on arthroscopic view. Santori and Villar13) reported that arthroscopy revealed early-stage osteoarthritis in a considerable number of patients with normal findings on plain radiographs. Since plain radiography does not provide an accurate view of internal conditions of the joint, if necessary, hip arthroscopy should be used to further confirm intra-articular lesions. Plain radiography and CT provide insight into the degree of articular injury in cases with a severe fracture or lesion, but not in cases with a mild injury of the articular surface. For this reason, a diagnosis should be made after a comprehensive assessment of clinical examination and additional evaluation.
The Kocher-Langenbeck approach is commonly considered for patients with a posterior wall fracture of the acetabulum and posterior column fracture14). Baumgaertner15) obtained unsatisfactory clinical outcomes in 32% of cases with posterior wall fractures. Several factors affect clinical results, including: i) the degree of fracture reduction, ii) fracture pattern, iii) the presence of intra-articular fragments, iv) femoral head injury associated with the fracture, v) extension of the fracture line into the acetabular dome, and vi) the use of intra-articular fixation devices15161718). The major limitation of the Kocher-Langenbeck approach is incomplete visualization of the entire acetabulum and femoral head. To overcome this shortcoming, Tannast et al.19) reported the outcome of surgical dislocation that chondral lesions were mainly detected in the anterior medial aspect of the femoral head and the posterior superior portion of the acetabulum, and labral lesions were mostly found in the posterior wall of the acetabulum. Maini et al.20) reported the usefulness of surgical dislocation in the treatment of acetabular fractures and chondral lesions were mostly in the anterosuperior zone in 9 cases with chondral lesion in the femoral head. A surgical approach to the acetabulum through surgical dislocation has an advantage of providing a better operative view, but this invasive procedure may disrupt femoral head blood supply, delay recovery, and increase the risk of nonunion when performing trochanteric osteotomy. Arthroscopy in hip fracture surgery can be considered as a complementary treatment option by allowing an improved surgical view in cases without surgical dislocation, and is can be expected to lower the risk of complications associated with surgical dislocation. However, since hip arthroscopy requires multiple surgical instruments, lengthens operating time and increases the risk of fluid extravasation through the fracture site, thorough intraoperative monitoring is warranted.
This retrospective study was limited by the relatively small sample size, the relatively short follow-up period and technical challenges in arthroscopic surgery for the treatment of fractures.
No clinical differences were seen in patients with acetabular fractures or hip fracture-dislocation when treated with and without arthroscopic surgery before open reduction and internal fixation. However, arthroscopy is thought to be useful for evaluating the joint cartilage surface and fracture fragments more accurately.
References
1. Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013; 29:661–665. PMID: 23375668.

2. Khanna V, Harris A, Farrokhyar F, Choudur HN, Wong IH. Hip arthroscopy: prevalence of intra-articular pathologic findings after traumatic injury of the hip. Arthroscopy. 2014; 30:299–304. PMID: 24581254.

3. Yamamoto Y, Ide T, Ono T, Hamada Y. Usefulness of arthroscopic surgery in hip trauma cases. Arthroscopy. 2003; 19:269–273. PMID: 12627151.

4. McCarthy JC, Lee JA. Hip arthroscopy: indications, outcomes, and complications. Instr Course Lect. 2006; 55:301–308. PMID: 16958465.
5. Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005; 21:1496–1504. PMID: 16376242.

6. McCarthy JC. Hip arthroscopy: when it is and when it is not indicated. Instr Course Lect. 2004; 53:615–621. PMID: 15116651.
8. Hwang DS, Kang C, Cha SM, Kim JH. Second-look arthroscopy after arthroscopic labrectomy of the hip-preliminary report. J Korean Orthop Assoc. 2009; 44:480–485.
9. Lim BH, Jang SW, Park YS, Lim SJ. Open repair and arthroscopic follow-up of severely delaminated femoral head cartilage associated with traumatic obturator fracture-dislocation of the hip. Orthopedics. 2011; 34:199. PMID: 21667908.

10. Hwang JM, Hwang DS, Lee WY, Noh CK, Zheng L. Hip arthroscopy for incarcerated acetabular labrum following reduction of traumatic hip dislocation: three case reports. Hip Pelvis. 2016; 28:164–168. PMID: 27777919.

11. Kim YT, Ninomiya S, Tachibana Y, Tanabe T, Yano Y. Acetabular labrum entrapment following traumatic posterior dislocation of the hip. J Orthop Sci. 2003; 8:232–235. PMID: 12665963.

12. Hwang JT, Lee WY, Kang C, Hwang DS, Kim DY, Zheng L. Usefulness of arthroscopic treatment of painful hip after acetabular fracture or hip dislocation. Clin Orthop Surg. 2015; 7:443–448. PMID: 26640626.

13. Santori N, Villar RN. Acetabular labral tears: result of arthroscopic partial limbectomy. Arthroscopy. 2000; 16:11–15.

14. Rommens PM. The Kocher-Langenbeck approach for the treatment of acetabular fratures. Eur J Trauma. 2004; 30:265–273.

15. Baumgaertner MR. Fractures of the posterior wall of the acetabulum. J Am Acad Orthop Surg. 1999; 7:54–65. PMID: 9916185.

16. Bosse MJ. Posterior acetabular wall fractures: a technique for screw placement. J Orthop Trauma. 1991; 5:167–172. PMID: 1861192.
17. Kreder HJ, Rozen N, Borkhoff CM, et al. Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. J Bone Joint Surg Br. 2006; 88:776–782. PMID: 16720773.

18. Saterbak AM, Marsh JL, Brandser E, Nepola JV, Turbett T. Outcome of surgically treated posterior wall aceatabular fractures. Orthop Trans. 1997; 21:627.
19. Tannast M, Krüger A, Mack PW, Powell JN, Hosalkar HS, Siebenrock KA. Surgical dislocation of the hip for the fixation of acetabular fractures. J Bone Joint Surg Br. 2010; 92:842–852. PMID: 20513883.

20. Maini L, Batra S, Arora S, Singh S, Kumar S, Gautam VK. Surgical dislocation of the hip for reduction of acetabular fracture and evaluation of chondral damage. J Orthop Surg (Hong Kong). 2014; 22:18–23. PMID: 24781607.

Fig. 1
(A) Posterior wall fracture and bone fragment in right hip joint was seen at preoperative X-ray, (B) computed tomography (CT), and (C) three-dimentional CT.
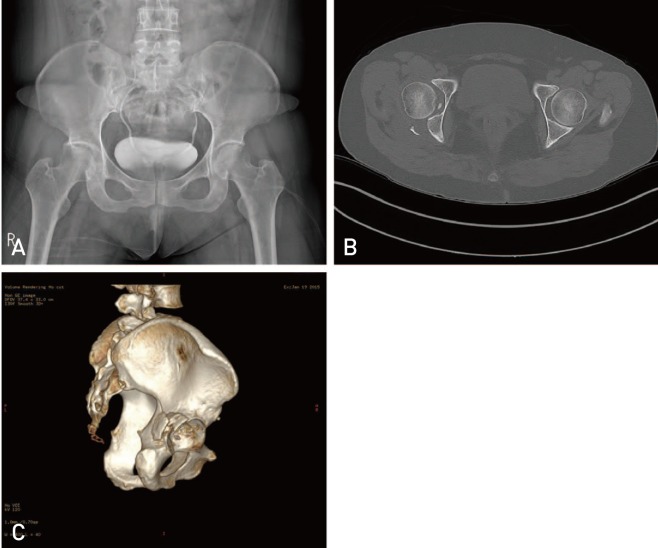
Fig. 2
(A) Femoral head was posterior dislocated. (B) Reduction was done. (C) Posterior wall fracture and bone fragment was seen in preoperative computed tomography (CT) and (D) three-dimensional CT.
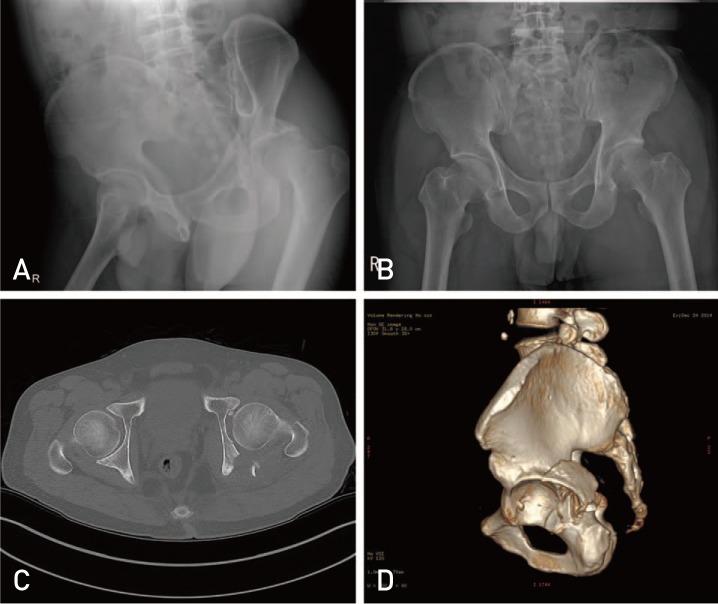
Fig. 3
Intraoperative arthroscopic finding, injured acetabular cartilage, labrum and bone fragment was seen.
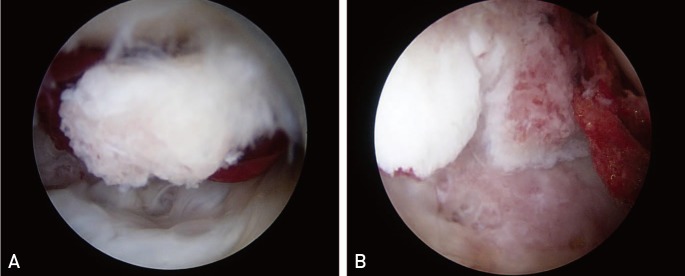
Fig. 4
Intraoperative arthroscopic finding, (A) Acetabular fracture gap was seen. (B) Injured acetabular cartilage was seen.
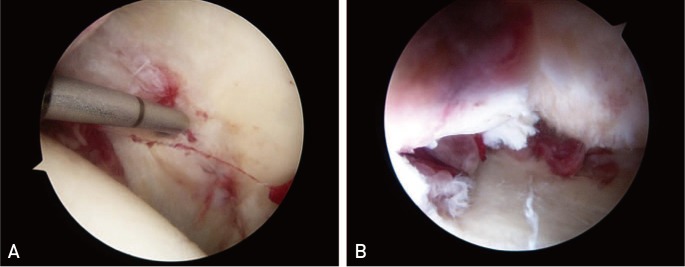
Fig. 5
(A) Plate fixation was seen in postoperative radiography. (B) Specific abnormal change was not seen in follow up radiography.
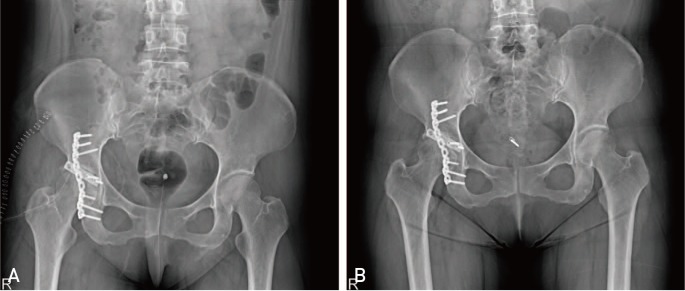
Fig. 6
(A) Plate fixation was seen in postoperative radiography. (B) Specific abnormal change was not seen in follow up radiography.
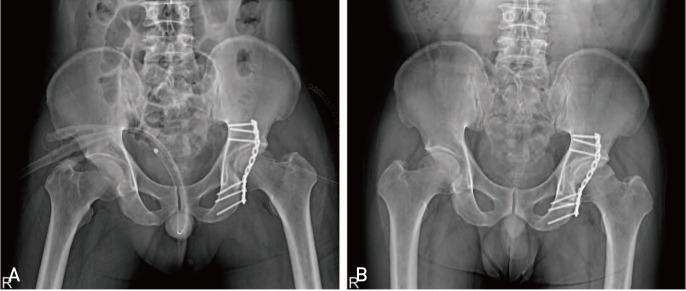
Fig. 7
(A) Left hip fracture and dislocation was seen in preoperative radiography. (B) Open reduction and internal fixation was done. (C) After 2 years, osteoarthric change was checked. (D) Total hip arthroplasty was done.
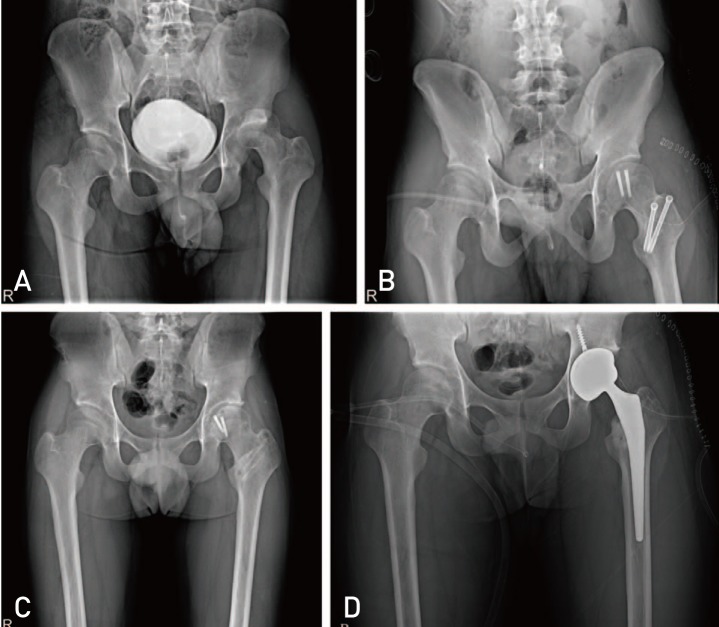
Table 1
Preoperative and Postoperative Results
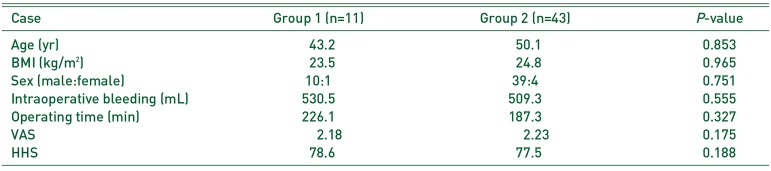
Table 2
Artrhoscopic Findings in Group 1




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download