Abstract
Purpose
To assess the relationship between eye position and anesthesia depth using the bispectral index (BIS) value, a parameter derived from electroencephalography data.
Methods
We investigated the relationship between BIS value and eye position in 32 children who underwent surgery for epiblepharon under general anesthesia. BIS values were recorded continuously throughout the procedure (from induction to awakening). Eye positions were video-recorded and analyzed after surgery. The vertical position of each eye was scored according to its height in relation to the medial canthus. An eye position in which the upper eyelid covered one-third of the cornea was defined as a significant ocular elevation.
Results
The BIS value correlated inversely with the end-tidal concentration of each anesthetic agent, whereas it correlated positively with the eye elevation score (eye position = 0.014 × BIS + 0.699, p = 0.011). The mean eye position score was significantly greater in patients whose BIS values were over 65. Eleven patients (34.4%) had significant ocular elevation; their mean concurrent BIS value was 61.6. Two of these patients had elevation during surgery and 9 had elevation during emergence from anesthesia.
Conclusions
We found that high BIS values were correlated with low levels of anesthetic concentration and high eye position, suggesting that BIS monitoring may be useful for predicting eye position during anesthesia. Particular attention must be given to eye position during ophthalmic surgery. Anesthesia depth can be maintained by assuring that the BIS value remains below 65.
The eyes generally have slightly divergent and elevated positions during general anesthesia [1]. However, eccentric eye positions that develop unexpectedly during anesthesia, such as an extreme upward gaze, can be problematic for all ocular procedures, especially surgery for pediatric strabismus or ptosis [2]. For example, the occurrence of eccentric eye positions during anesthesia can lead to an unsatisfactory surgical field and increase the risk of ophthalmological complications [2]. However, these eye movements can be helpful to anesthesiologists, who can use them to help evaluate the depth of anesthesia [34]. Despite its potential utility, the absence of a validated system for monitoring the depth of anesthesia has prevented quantitative examination of the relationship between eye elevation and anesthesia depth [2].
The bispectral index (BIS) monitoring system gathers processed electroencephalography (EEG) parameters and provides a simple pharmacodynamic measure of the hypnotic effect of anesthetic or sedative drugs on the central nervous system [56789]. The BIS value ranges from 0 to 100; a value of 65 to 85 is recommended for sedation and a value of 40 to 65 for general anesthesia [5]. Recent pediatric studies have indicated that the BIS value is a good general measure of the depth of anesthesia and have validated its utility for this purpose [6789]. Thus, BIS monitoring may help ensure that children remain unconscious during anesthesia and are in a suitable condition for surgery [679]. In the present study, we aimed to quantitatively characterize the relationship of eye position with anesthesia depth using BIS monitoring in children undergoing eyelid surgery.
This prospective observational study followed the tenets of the Declaration of Helsinki and was approved by the institutional review board of Ajou University School of Medicine, Korea (AJIRB-MED-OBS-12-162). A parent or legal guardian provided written informed consent for the participation of each child. Unpremedicated healthy children (American Society of Anesthesiologists physical status classification 1) who were scheduled for elective surgery to correct epiblepharon in the lower eyelids were enrolled. Children younger than 3 years were excluded because BIS monitoring of anesthesia depth has not been validated for this population [89]. Likewise, children with ocular comorbidities (including eye movement disorders), children with neurologic disorders, children with developmental delays, and children who used anti-epileptic or anti-psychotic drugs were excluded.
Anesthesia was induced and maintained by inhalational sevoflurane (21 patients) or desflurane (11 patients). Neuromuscular blockade was achieved for intubation with a single dose of rocuronium (0.5 mg/kg) in all cases. A BIS monitor (Aspect-2000; Aspect Medical Systems, Newton, MA, USA) and a BIS pediatric sensor (Aspect Medical Systems) were used to monitor anesthesia depth. The skin was first cleansed with 70% ethanol, after which a BIS electrode was placed fronto-laterally on the patient's forehead following the manufacturer's recommendations. BIS values and hemodynamic parameters, including electrocardiography, pulse oximetry, and non-invasive blood pressure, were recorded automatically and continuously from induction until 3 to 5 minutes after extubation. A BIS signal quality index greater than 95% was accepted as reliable.
Eye position was video-recorded during anesthesia and analyzed after surgery at 1-minute intervals by an examiner who was blinded to the BIS results. The positions of both eyes were assessed by gentle exposure using a speculum during the induction and emergence from anesthesia; the fellow eye was assessed during surgery. To prevent unnecessary stimulation, the cornea was protected by a covering of hyaluronic acid in the form of an ophthalmic viscosurgical device. The vertical position of each eye was scored on an ordinal scale from −2 to +6, according to its height in relation to the medial canthus (Fig. 1A, 1B). For this analysis, a circular tape with a diameter of 15 mm was placed in the middle of the glabella and used as a reference for eye position scoring. The eye position was calculated as the ratio of the height to the circular tape size and was scored at 1 mm intervals. Thus, higher eye positions in relation to the medial canthus resulted in higher scores. Positive values reflect superior positions and negative values reflect inferior positions. An eye position with a score of +4 or more, where the upper eyelid covered one-third of the cornea, was defined as significant ocular elevation. For cases in which both eyes were assessed, the position of the eye with the greater change (higher score) was selected for analysis.
After determining the relationship between BIS value and anesthesia depth (end-tidal volume of inhalation agents), the relationship between all BIS values and eye position scores was first evaluated using linear regression analysis. Then, to determine the BIS cut-off value for stable eye position, the eyes were binned into 5 different groups according to their BIS value (<36, 36–45, 46–55, 56–65, and >65). The maximum recommended BIS value for general anesthesia compatible with surgery is 65. We compared the eye position scores among the BIS groups using one-way analysis of variance. The incidence of significant ocular elevation was also assessed at every moment, correlated with the concurrent BIS values, and analyzed in the different BIS groups using a chi-square test. The Bonferroni method was used for post-hoc analysis. All statistical analyses were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL., USA) and a p-value less than 0.05 was considered significant.
We initially enrolled 34 children, but excluded 2 of these children from the analysis due to their poor BIS signal quality indexes (<95%). Thus, we studied 64 eyes from 32 children (13 males; mean age, 5.4 years; age range, 3 to 10 years). None of the patients moved intraoperatively or had any intraoperative clinical signs of awareness. The mean duration of surgery was 19.09 ± 4.83 minutes and that of anesthesia was 32.16 ± 5.41 minutes. We ultimately analyzed 1,055 observations of eye positions, of which 198 represented the highest eye position scores in each 5-minute interval with the concurrent BIS values. The BIS values ranged from 24 to 77 (mean, 49.36) and the mean eye position score was 1.38 ± 1.07.
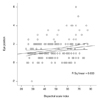
Linear regression analysis indicated that the BIS value correlated inversely with end-tidal sevoflurane (r = −0.486, p < 0.001) and desflurane (r = −0.405, p < 0.001) concentrations. However, the BIS value was correlated positively with eye position score (eye position = 0.014 × BIS + 0.699, r = 0.181, p = 0.011) (Fig. 2).
The mean eye position score was significantly greater in the group with BIS values over 65 than in the groups with BIS values <36, 36 to 45, and 56 to 65 (one-way analysis of variance, p = 0.005) (Table 1 and Fig. 3). Eye position scores of +2 or more (25 of 34 time-points, 73.5%) mainly occurred when the BIS values were over 65; all of the downward eye drift with negative eye position scores (3 of 3 time points, 100%) occurred when the BIS values were below 35 (chi-square test, p < 0.001).
Significant ocular elevation occurred in 11 patients (34.4%). For 2 of these patients, the elevation occurred during surgery; for 9 of these patients, the elevation occurred during emergence from general anesthesia. The mean BIS value of the 17 time-points when patients had significant ocular elevation was 61.59 (range, 40 to 77). Eleven of these 17 time-points (64.7%) occurred when the BIS value was above 65. Pearson's correlation analysis indicated that the magnitude of change in eye position score during anesthesia was not significantly related to the magnitude of changes in the BIS value, patient age, or surgery duration. In addition, comparisons of the right versus left eyes, males versus females, and sevoflurane versus desflurane anesthesia indicated no significant differences in eye position scores (Student's t-test, p > 0.05 for all comparisons).
This study demonstrated a significantly positive relationship between BIS value and eye elevation score in healthy children given anesthesia for epiblepharon surgery. As the pediatric BIS value has also been shown to have a significant negative correlation with anesthesia depth [67], our results suggest that a shallower level of anesthesia is related to a higher eye position.
Eye movements occur during induction of anesthesia and the eye position under anesthesia may differ somewhat from that in the conscious state [1234]. However, few published studies have provided data for comparison of our results. A few studies have evaluated eye position under general anesthesia in patients with strabismus for adjustment of surgical results [101112]. However, most reports on eye position during anesthesia have examined controversial issues related to horizontal deviation and focused on the correlation between clinical preoperative deviation with ocular alignment under anesthesia [91011]. Only one study evaluated the incidence of eccentric ocular position in patients under anesthesia [2]. This study reported an incidence of eccentric ocular position of 8%, which increased to 18% without the use of muscle relaxants. The authors reported that an eccentric ocular position was more likely during the light planes of general anesthesia, as first described by Snow in 1847 [3]. Guedel [4] refined the concept of anesthetic depth and reported that the extraocular muscles became flaccid during the deeper planes of anesthesia. This finding led to the use of balanced general anesthesia with non-depolarizing muscle relaxants [2]. In our study, we found that 34.4% of the patients had significant ocular elevation. One possible reason for this discrepancy could be the extended duration of our measurement period, which included the time of emergence from anesthesia. During surgery, only 2 patients (6.3%) showed eye elevation, similar to previously published results [2]. In addition, eccentric elevation during surgery of these 2 patients occurred at 26 and 29 minutes after induction; there was little effect of muscle relaxants considering the action period of rocuronium (non-polarizing neuromuscular blocking agent with an intermediate duration of 20 to 30 minutes) [13]. However, this previous study was an observational survey that used a questionnaire completed by the anesthetist, did not specifically define significant ocular deviation, and included some patients undergoing cataract surgery in whom surgical instruments may have been used to hold the eyes [2]. Therefore, this previous study did not objectively assess the relationship of eye elevation with depth of anesthesia.
Some previous anesthesiology studies have attempted to characterize the relationship of eye movement with anesthetic depth using closed-eye movement tracking [141516]. For example, Kevin et al. [14] compared ocular microtremors with BIS values to predict responses to verbal commands. Deletis et al. [15] aimed to record the blink reflex during anesthesia. Power et al. [16] examined the relationship of non-rapid eye movement (REM) stage sleep induced by anesthesia with eye movements using electrooculography in closed eyes. Other research examined REM during sleep in the form of tandem movements [17]. However, the focus of these previous studies differed from the focus of the present study, which was fixed eccentric eye elevation during surgery.
Although the relationship between eccentric ocular elevation during anesthesia and a shallow level of anesthesia seems intuitive, it is unclear why an eccentric eye position usually manifests as a fixed ocular elevation. Rossiter et al. [2] posited that this eccentric eye position may develop because of an intense and sustained contraction of the superior rectus muscle over its opposing muscle. However, we found no evidence in the literature to support this assertion. Although the tension and active force of the medial rectus muscle is higher than that of the lateral rectus muscle [18], the eyes usually diverge under anesthesia [1]. In addition, complete lack of electrical discharge in the extraocular muscles only occurs during deep sleep or deep anesthesia [1]. In a light plane of anesthesia, electrical activity is present in the extraocular muscles. Further physiologic studies using electromyography to assess the superior rectus and inferior rectus muscles during anesthesia may help resolve this issue. Harrad and Stoddart [19] suggested that Bell's phenomenon may explain this eccentric eye position. However, the protection afforded by Bell's phenomenon is significantly decreased during general anesthesia [20]. The eccentric ocular elevation during the light plane of anesthesia would also differ from REM sleep. In REM sleep, brain activity becomes quite intense, similar to that during wakefulness; moreover, REM occurs just before awakening [17]. In our study, eccentric eye elevation with concurrent elevation of BIS values also occurred more frequently during the emergence from anesthesia than during surgery. Although the similar timing of these phenomena is consistent with a causal relationship, general anesthesia aims to induce non-REM sleep and eyes usually move in tandem but unfixed patterns in REM sleep.
We also cannot explain why patients with similar BIS values had significant differences in ocular elevation. Individual differences in BIS monitoring or eye movements are one potential explanation. The BIS value has been shown to correlate well with sevoflurane concentration (or consciousness level) during anesthesia in adults and children, but not in infants due to maturational differences represented in their EEG results [8]. Although we excluded children younger than 3 years and found that the BIS value did not differ significantly with age, there may be inter-individual differences in EEG patterns in young children due to different maturation rates. Also, contraction of the orbicularis oculi muscle may cause the electromyography to appear as an artifact, thereby increasing the BIS value, especially in children with small foreheads [21]. One study that compared clinical eye signs with EEG polysomnography under anesthesia reported that the deepest level of sleep occurred an average of 3 minutes prior to the onset of eccentric ocular positioning [16]. Therefore, eye movement may still occur when anesthesia appears to be satisfactory. Further studies of individual differences in ocular elevation under anesthesia are warranted.
There are several limitations to our study. First, we only evaluated vertical eye position, not horizontal position. Divergence during anesthesia must have occurred [1]. However, our focus was on ocular elevation that could interrupt the surgical field during an operation. Because of the ocular contour, vertical eye movement might be more uncomfortable than horizontal eye movement during surgery. Second, we excluded patients with strabismus, and eye movements in these patients might be different [12]. Third, we selected the highest BIS value within each 5-minute window to detect subtle movements. In practice, hemodynamic monitoring is usually performed at 5-minute intervals. Thus, we analyzed values representative of each 5-minute period, similar to practice, even though we collected data at 1-minute intervals. Thus, we could not determine the exact timing of the different events. Finally, we evaluated eye position using a scoring system, not actual values, to facilitate statistical analysis. However, we validated our scoring system by the use of reference values to reduce bias.
In summary, we found that a shallower level of anesthesia was associated with a higher BIS value and a higher eye position score. This suggests that BIS monitoring may be beneficial in predicting eye position during anesthesia. In ophthalmic surgeries, an appropriate depth of anesthesia can be maintained by monitoring BIS values and ensuring they remain in the range of 35 to 65, especially for congenital ptosis in which eye position is important. Moreover, BIS monitoring during anesthesia may help achieve better surgical results and prevent complications. In addition, the findings presented here could be used as the basis for further studies.
Figures and Tables
Fig. 1
Method used to score eye position (height) in relation to the medial canthus indicated with a yellow arrow. (A) A positive value indicates a superior position and a negative value indicates an inferior position. (B) A higher eye position in relation to the medial canthus is assigned a higher eye position score. A 15-mm circular tape was used as a reference to score eye position in this analysis.

Fig. 2
Linear regression analysis of eye position and bispectral index (BIS) value (eye position = 0.014 × BIS + 0.699, r = 0.181, p = 0.011).
References
1. von Noorden GK, Campos EC. Classification of neuromuscular anomalies of the eyes. In : von Noorden GK, Campos EC, editors. Binocular vision and ocular motility: theory and management of strabismus. 6th ed. St. Louis: CV Mosby;2002. p. 110–128.
2. Rossiter JD, Wood M, Lockwood A, Lewis K. Operating conditions for ocular surgery under general anaesthesia: an eccentric problem. Eye (Lond). 2006; 20:55–58.

3. Snow JD. On the inhalation of the vapour of ether in surgical operations. Br J Anaesth. 1953; 25:253–267.

4. Guedel AE. Inhalation anaesthesia: a fundamental guide. 1st ed. Macmillan: New York;1937. p. 63–64.
5. Sebel PS, Lang E, Rampil IJ, et al. A multicenter study of bispectral electroencephalogram analysis for monitoring anesthetic effect. Anesth Analg. 1997; 84:891–899.

6. McCann ME, Bacsik J, Davidson A, et al. The correlation of bispectral index with endtidal sevoflurane concentration and haemodynamic parameters in preschoolers. Paediatr Anaesth. 2002; 12:519–525.

7. Denman WT, Swanson EL, Rosow D, et al. Pediatric evaluation of the bispectral index (BIS) monitor and correlation of BIS with end-tidal sevoflurane concentration in infants and children. Anesth Analg. 2000; 90:872–877.

8. Davidson AJ, McCann ME, Devavaram P, et al. The differences in the bispectral index between infants and children during emergence from anesthesia after circumcision surgery. Anesth Analg. 2001; 93:326–330.

9. Ganesh A, Watcha MF. Bispectral index monitoring in pediatric anesthesia. Curr Opin Anaesthesiol. 2004; 17:229–234.

10. Apt L, Isenberg S. Eye position of strabismus patients under general anesthesia. Am J Ophthalmol. 1977; 84:574–579.

11. Romano P, Gabriel L. Intraoperative adjustment of eye muscle surgery: correction based on eye position during general anesthesia. Arch Ophthalmol. 1985; 103:351–353.
12. Castanera de Molina A, Giner Munoz ML. Ocular alignment under general anesthesia in congenital esotropia. J Pediatr Ophthalmol Strabismus. 1991; 28:278–282.

13. Cheeseman JF, Merry AF, Pawley MD, et al. The effect of time of day on the duration of neuromuscular blockade elicited by rocuronium. Anaesthesia. 2007; 62:1114–1120.

14. Kevin LG, Cunningham AJ, Bolger C. Comparison of ocular microtremor and bispectral index during sevoflurane anaesthesia. Br J Anaesth. 2002; 89:551–555.
15. Deletis V, Urriza J, Ulkatan S, et al. The feasibility of recording blink reflexes under general anesthesia. Muscle Nerve. 2009; 39:642–646.

16. Power C, Crowe C, Higgins P, Moriarty DC. Anaesthetic depth at induction. An evaluation using clinical eye signs and EEG polysomnography. Anaesthesia. 1998; 53:736–743.
17. Boukadoum AM, Ktonas PY. EOG-based recording and automated detection of sleep rapid eye movements: a critical review, and some recommendations. Psychophysiology. 1986; 23:598–611.

18. Collins CC, Carlson MR, Scott AB, Jampolsky A. Extraocular muscle forces in normal human subjects. Invest Ophthalmol Vis Sci. 1981; 20:652–664.
19. Harrad RA, Stoddart P. Operating conditions for ocular surgery under general anaesthesia: an eccentric problem. Eye (Lond). 2007; 21:256–257.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download