Abstract
Purpose
To investigate factors associated with pain intensity following intravitreal injection and factors that might be associated with changes in pain intensity in patients who received repeated injections.
Methods
A total of 172 eyes (147 patients) were prospectively enrolled. Patients rated their pain from 0 to 10 using a visual analogue scale. Multiple linear regression analysis was used to evaluate factors associated with pain score. Sixty-eight patients evaluated their degree of pain more than once and were divided into three groups according to changes in pain during repeated injections. Clinical factors were compared among the three groups.
Results
Pain scores of women (women, 3.1 ± 1.5 vs. men, 2.4 ± 1.2; p = 0.003), those who received dexamethasone implant injection (dexamethasone implant, 3.5 ± 1.1 vs. anti-vascular endothelial growth factor, 2.7 ± 1.4; p = 0.028), and those who did not undergo anterior chamber paracentesis (ACP) (ACP, 2.6 ± 1.3 vs. no ACP, 3.0 ± 1.6; p = 0.047) were significantly higher than those of the other groups. On multiple linear regression analysis, only female sex and ACP were significantly associated with degree of pain. The waiting time during the second injection was significantly associated with change in degree of pain in patients who received repeated injections.
Conclusions
Women were more prone to perceive pain, and the ACP procedure reduced pain during intravitreal injections. Most patients who received repeated injections felt that pain was similar or decreased compared to that experienced during the previous injection. However, increased waiting time might have been associated with increased discomfort for patients who received repeated injections.
Intravitreal injection is used as the primary treatment for diseases such as neovascular age-related macular degeneration [1], diabetic macular oedema [2], and macular oedema associated with retinal vein occlusion [3]. Although intravitreal injection is known to be a safe procedure with few complications, multiple treatments are often needed because of the high rate of disease recurrence and short half-life of the drug.
Topical anaesthesia is usually administered before the procedure [4], and a 30-gauge fine needle is used to minimize pain [5]. However, patients report different perceptions of pain.
Many studies have investigated the degree of pain following intravitreal injections [678910111213]. However, in most studies, the pain associated with a single injection was measured. Few studies, however, have measured the degree of pain after repeated injections in the same patient [14], and the degree of subjective pain felt after injection might be different for each injection.
Thus, the purpose of this study was to evaluate clinical factors that might affect the degree of pain following intravitreal injections. In addition, we evaluated factors that might be associated with changes in the degree of pain in patients who received repeated injections.
This was a prospective, observational study. All patients were given an explanation of the aims of the study, and informed consent was obtained from each patient before intravitreal injection. This study was reviewed and approved by the institutional review board of Kangdong Sacred Heart Hospital, Seoul, Korea (2015-12-020). All study conduct adhered to the tenets of the Declaration of Helsinki.
We consecutively enrolled patients who underwent intravitreal injection from December 1, 2015 to November 30, 2016. Inclusion criteria were as follows: patients with neovascular age-related macular degeneration, diabetic macular oedema, retinal vein occlusion with macular oedema, and others who underwent intravitreal injection. Exclusion criteria were as follows: patients with any ophthalmic diseases that might affect the degree of pain, such as severe dry eye or corneal diseases; patients with systemic conditions that might affect the degree of pain, such as diabetic polyneuropathy; or patients who were unable to read and respond to the questionnaire. Drugs used for intravitreal injection were bevacizumab, ranibizumab, aflibercept, and dexamethasone implant.
After the patient reclined for the injection, two drops of topical anaesthetic (proparacaine hydrochloride 0.5%; Alcaine, Novartis, Basel, Switzerland) were administered. After 5 minutes, the periocular skin, eyelids, and eyebrows were disinfected with 10% povidone-iodine. Patients were kept waiting for 5 to 10 minutes before the operator entered the operating room. The waiting time was defined as the time interval between when the patient entered the room and when they received the injection. When the operator came into the room, a speculum was placed into the patient's eye, and two drops of topical anaesthetics and 5% povidone-iodine were administered into the eye. After 1 minute, injections were administered to the superotemporal quadrant of the right eye and to the superonasal quadrant of the left eye because surgeons were right-handed, except in 5 cases where injections were administered to the other quadrants due to conjunctival lesions or scars. Drugs used for intravitreal injection were bevacizumab (0.05 mL; Genentech, San Francisco, CA, USA), ranibizumab (0.05 mL; Novartis, East Hanover, NJ, USA), aflibercept (0.05 mL; Regeneron, Tarrytown, NY, USA), and dexamethasone implant (0.7 mg; Allergan, Irvine, CA, USA). Anterior chamber paracentesis (ACP) was performed immediately after intravitreal injection using a manually bent 30-gauge needle penetrating the anterior chamber in the limbal region, and about 0.1 mL of aqueous humour was sampled. After the overall process of intravitreal injection, we recorded the presence or absence of subconjunctival haemorrhage and whether ACP was performed. ACP was performed at the surgeon's discretion and was performed in most patients to decrease the intraocular pressure spike after intravitreal injection [15]; however, ACP was not performed when the anterior chamber was very shallow in order to prevent lens damage. Degree of pain was assessed using a visual analogue scale (VAS) 5 minutes after the injection. The VAS ranged from 0 to 10. In patients who underwent repeated injections, the same surgeon performed the procedure, and patients were asked to describe changes in the degree of pain compared to previous injections using one of the following descriptive terms: increased, unchanged, or decreased.
IBM SPSS ver. 23.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis. A p-value <0.05 was considered significant. Student's t-test or one-way analysis of variance (ANOVA) was used for univariate analysis to investigate factors associated with the degree of pain following intravitreal injection. Multiple linear regression analysis was also used to evaluate factors associated with pain score. Patients who assessed their degree of pain more than once were classified into three groups: increased, unchanged, or decreased. The increased group was defined as patients who reported more pain during the current treatment than previous injections. The unchanged group included those who did not perceive a noticeable difference compared to the previous injection, and the decreased group included those who felt less pain compared to the previous injection. Clinical factors were compared among the three groups using a one-way ANOVA test.
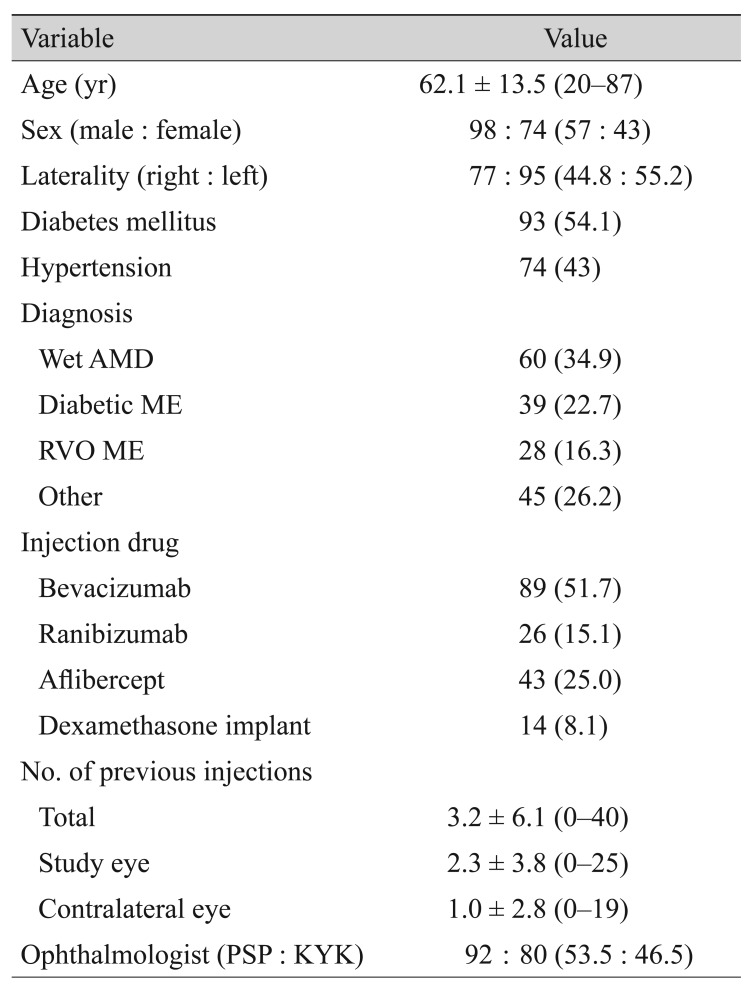
In this study, 172 eyes of 147 patients were finally enrolled for analysis. Indications for injection were wet age-related macular degeneration (34.9%), diabetic macular oedema (22.7%), macular oedema associated with retinal vein occlusion (16.3%), and other diseases such as diabetic vitreous haemorrhage, myopic choroidal neovascularisation, or pseudophakic cystoid macular oedema (26.2%). Drugs used for intravitreal injection were bevacizumab (51.7%), ranibizumab (15.1%), aflibercept (25%), and dexamethasone implant (8.1%) (Table 1).
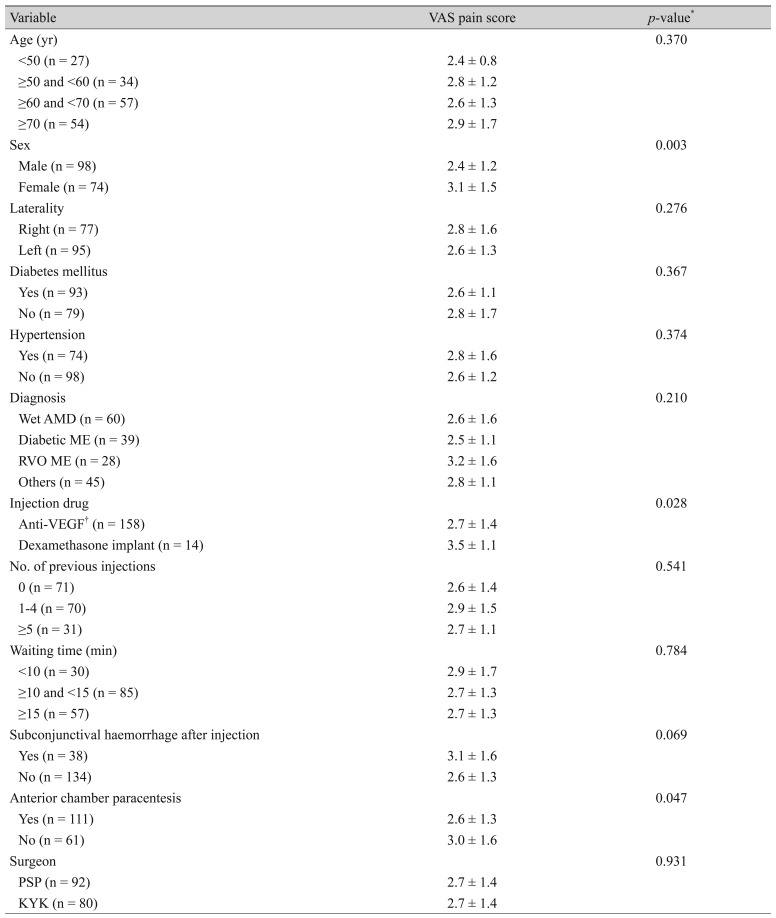
Pain score was significantly higher in women than in men (women, 3.1 ± 1.5 vs. men, 2.4 ± 1.2; p = 0.003, Student's t-test). Pain score of the dexamethasone implant injection group was significantly higher than that of the anti-vascular endothelial growth factor (VEGF; bevacizumab, ranibizumab, and aflibercept) injection group (dexamethasone implant, 3.5 ± 1.1 vs. anti-VEGF, 2.7 ± 1.4; p = 0.028). In addition, the pain score was significantly lower in patients who underwent ACP than in patients who did not (ACP, 2.6 ± 1.3 vs. no ACP, 3.0 ± 1.6; p = 0.047). There was no significant difference between the group that experienced subconjunctival haemorrhages (SCHs) and the group that did not, but the group with SCHs tended to have a higher pain score (SCH, 3.1 ± 1.6 vs. no SCH, 2.6 ± 1.3; p = 0.069). However, factors such as age, laterality, underlying disease, indications for injection, and previous injection experience were not associated with degree of pain (Table 2).
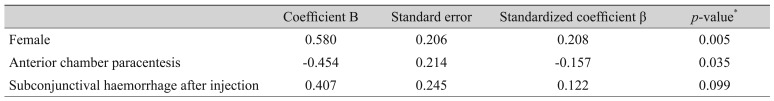
On multiple linear regression analysis, only female sex (standardized coefficient β = 0.208; p = 0.005, multiple linear regression) and ACP (standardized coefficient β = −0.214, p = 0.035) were significantly associated with degree of pain (Table 3).
We classified patients who assessed their degree of pain more than once during the study period into three groups. Seven patients reported that their degree of pain increased compared to the previous injection (increased group), 44 patients reported a similar level of pain (unchanged group), and 17 patients reported decreased pain compared to the previous injection (decreased group). The increased group also rated significantly higher pain scores for the second injection (second pain score, 4.4 ± 0.8 vs. first pain score, 2.1 ± 1.5; p < 0.001, one-way ANOVA test). The unchanged group reported a similar level of pain for both injections (second pain score, 2.8 ± 0.8 vs. first pain score, 2.9 ± 1.5; p = 0.514), while the decreased group reported a decreased level of pain on the second injection (second pain score, 1.5 ± 1.1 vs. first pain score, 3.5 ± 1.7; p = 0.005). The waiting time during the second injection was significantly longer in the increased group compared to the other groups (increased group, 16.0 ± 5.4 minutes; unchanged group, 13.2 ± 4.4 minutes; decreased group, 11.2 ± 2.7 minutes; p = 0.036). The waiting time during the first injection tended to be longer in the increased group, although there was no statistical significance (p = 0.097). There were also no significant differences among the three groups regarding age, sex, underlying diseases, accompanying SCH, or ACP (Table 4).
According to previous studies, there was a significant difference in the degree of pain following intravitreal injections between men and women. Of these studies, that by Rifkin and Schaal [14] reported that women probably reported lower pain scores due to personality, emotional state, or expectation of a positive result; Haas et al. [16] reported that females reported higher pain scores due to multiple factors such as sensitivity to noxious stimuli, sex hormones, and others. According to studies investigating the relationship between general pain and sex [1718], women are more prone to perceive pain compared to men. Suggested mechanisms for higher perceived pain in women include menstruation-related hormonal changes, a higher level of activity in the endogenous opioid system that controls pain sensitivity, differences of spatial patterns in brain imaging, and a stronger analgesic response. The increased perceived pain in women after intravitreal injections in our study could also be interpreted based on these factors.
Several studies have investigated the relationship between needle size and pain. One study reported that there was no difference in the degree of pain between 30-gauge and 27-gauge needles [5], but patients in several other studies reported less pain when using a 30-gauge needle compared to a 27-gauge needle [1316]. Moisseiev et al. [8] also reported that there was no significant difference in the degree of pain between bevacizumab and dexamethasone implant injections, which might be because of the tunnelled technique to prevent vitreal reflux used in dexamethasone implant injection. In our study, univariate analysis revealed that pain scores were higher in the dexamethasone group compared to the anti-VEGF injection group; however, there were no significant differences according to multivariate analysis. It seems that, if appropriate anaesthesia is applied, a 27-gauge dexamethasone implant injection does not induce significantly greater pain compared to a 30-gauge fine needle injection.
Interestingly, in this study, patients who underwent ACP during the injection procedure reported less pain than those who did not. There have been reports that ACP after intravitreal injection can decrease intraocular damage by decreasing intraocular pressure after injection [151920]. Knip and Valimaki [19] also reported that ACP did not significantly increase pain. Based on the previous study results and our results, it seems that the additional ACP procedure during intravitreal injection does not cause additive pain in patients or can alleviate discomfort by reducing the initial intraocular pressure spike following intravitreal injections. In previous studies, ACP was performed before intravitreal injections, while ACP was performed immediately after intravitreal injections in our study. The procedure order might have affected the degree of pain. Thus, further study is needed to reconfirm whether ACP is associated with the degree of pain of patients who undergo intravitreal injections.
In addition to the aforementioned factors, there have been some reports on differences in the degree of pain according to age [81416], type of anaesthetic [471121], and location of injection [1222]. Rifkin and Schaal [14] reported that older patients perceived more pain during intravitreal injections; however, others reported that older patients were associated with lower degree of pain [816]. In this study, we did not find any difference in the degree of pain according to patient age. Regarding injection location, some reported that there were no differences according to injection location [22]; however, some reported that less pain was associated with the superotemporal quadrant injections [12]. In this study, we used uniform methods of anaesthesia and injection location; thus, we were not able to assess the influence of these factors on the degree of pain.
In patients who received repeated injections, previous injection experience might affect the degree of pain. Rifkin and Schaal [14] reported that pain decreased as the number of injections increased. However, Haas et al. [16] reported that the degree of pain is greater in patients with a higher number of previous injections. There have also been reports that the degree of pain was not associated with previous injections [12]. Direct comparison is difficult because the type and interval of injections were different among studies; thus, the effect of previous injection experience on post-injection pain has not yet been established.
In our study, there was no difference in the degree of pain according to the number of previous injections. In this study, 68 patients assessed their degree of pain at least twice. Of these, most patients assessed the degree of pain as similar to that experienced during the previous injection, and the majority (90%) reported that pain was similar or decreased compared to that experienced during the previous injection. Those who evaluated the degree of pain following the later injection as different from the first injection actually rated it differently on the VAS. Thus, we could reconfirm that these patients actually felt differently between the two procedures. We investigated possible factors that might affect changes in the degree of pain; however, there were no significant differences among the 3 groups except waiting time for the second injection. It is plausible that patients who waited longer in the procedure room might have experienced more anxiety, which could have increased discomfort, and a recent study also reported a relationship between preprocedural anxiety and pain in intravitreal injections [23]. However, there were no significant differences among groups in terms of sex, performance of the ACP procedure, or SCH occurrence, which were shown to be associated with the degree of pain in multivariate analysis. There were also no significant differences among the 3 groups in waiting time difference between the first and the second injections, and further studies with a large number of patients are needed to clarify the relationship between waiting time and degree of pain.
Our study has some limitations. It included both treatment-naïve patients and those who had undergone previous injections. The interval of injection treatment in patients varied. These could have reflected a real-world treatment environment; however, the small sample size might have reduced the power to detect factors that might be associated with pain following intravitreal injections. ACP was associated with less pain; however, the intraocular pressure change after injection was not measured in this study. Additional factors such as personal characteristics or psychosocial factors should also be considered in evaluating the degree of perceived pain. Further studies that include a larger number of patients in a controlled setting are needed.
In conclusion, women were more prone to perceive pain, and the ACP procedure reduced pain during intravitreal injections. Most patients felt that the degree of pain following intravitreal injection was similar or decreased compared to that experienced during previous injections. However, increased waiting time might be associated with increased discomfort in patients who received repeated injections. Further study is needed to determine whether treatment delay affects the patient's psychological state, such as level of anxiety, and whether these factors affect the degree of pain.
References
1. Brown DM, Michels M, Kaiser PK, et al. Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology. 2009; 116:57–65. PMID: 19118696.

2. Do DV, Nguyen QD, Boyer D, et al. One-year outcomes of the da Vinci Study of VEGF Trap-Eye in eyes with diabetic macular edema. Ophthalmology. 2012; 119:1658–1665. PMID: 22537617.

3. Brown DM, Campochiaro PA, Singh RP, et al. Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010; 117:1124–1133. PMID: 20381871.
4. Davis MJ, Pollack JS, Shott S. Comparison of topical anesthetics for intravitreal injections: a randomized clinical trial. Retina. 2012; 32:701–705. PMID: 22282296.
5. Rodrigues EB, Grumann A Jr, Penha FM, et al. Effect of needle type and injection technique on pain level and vitreal reflux in intravitreal injection. J Ocul Pharmacol Ther. 2011; 27:197–203. PMID: 21314588.

6. Rifkin L, Schaal S. Shortening ocular pain duration following intravitreal injections. Eur J Ophthalmol. 2012; 22:1008–1012. PMID: 22562296.

7. Hernandez-Siman J, Marra K, Arroyo J. Sub-conjunctival lidocaine injection before intravitreal injection. Surv Ophthalmol. 2014; 59:672–673. PMID: 25444367.

8. Moisseiev E, Regenbogen M, Rabinovitch T, et al. Evaluation of pain during intravitreal Ozurdex injections vs. intravitreal bevacizumab injections. Eye (Lond). 2014; 28:980–985. PMID: 24924442.

9. Ulrich JN. Topical nepafenac after intravitreal injection: a prospective double-masked randomized controlled trial. Retina. 2014; 34:509–511. PMID: 23928675.
10. Andrade GC, Carvalho AC. Comparison of 3 different anesthetic approaches for intravitreal injections: a prospective randomized trial. Arq Bras Oftalmol. 2015; 78:27–31. PMID: 25714534.

11. Karabas VL, Ozkan B, Kocer CA, et al. Comparison of two anesthetic methods for intravitreal ozurdex injection. J Ophthalmol. 2015; 2015:861535. PMID: 25949822.
12. Massamba N, Elluard M, Agoune W, et al. Assessment of ocular pain following ranibizumab intravitreal injection. Acta Ophthalmol. 2015; 93:e231–e232. PMID: 25123226.

13. van Asten F, van Middendorp H, Verkerk S, et al. Are intravitreal injections with ultrathin 33-G needles less painful than the commonly used 30-G needles? Retina. 2015; 35:1778–1785. PMID: 25901838.

14. Rifkin L, Schaal S. Factors affecting patients' pain intensity during in office intravitreal injection procedure. Retina. 2012; 32:696–700. PMID: 22082694.

15. Ichiyama Y, Sawada T, Kakinoki M, et al. Anterior chamber paracentesis might prevent sustained intraocular pressure elevation after intravitreal injections of ranibizumab for age-related macular degeneration. Ophthalmic Res. 2014; 52:234–238. PMID: 25401265.

16. Haas P, Falkner-Radler C, Wimpissinger B, et al. Needle size in intravitreal injections - pain evaluation of a randomized clinical trial. Acta Ophthalmol. 2016; 94:198–202. PMID: 26521866.

17. Kozak I, Cheng L, Freeman WR. Lidocaine gel anesthesia for intravitreal drug administration. Retina. 2005; 25:994–998. PMID: 16340529.

18. Mogil JS, Bailey AL. Sex and gender differences in pain and analgesia. Prog Brain Res. 2010; 186:141–157. PMID: 21094890.

19. Knip MM, Valimaki J. Effects of pegaptanib injections on intraocular pressure with and without anterior chamber paracentesis: a prospective study. Acta Ophthalmol. 2012; 90:254–258. PMID: 20456259.

20. Katayama BY, Bonini-Filho MA, Messias AM, et al. Comparison of acetazolamide, brimonidine, and anterior chamber paracentesis for ocular hypertension control after initial intravitreal bevacizumab injection: a randomized clinical trial. J Glaucoma. 2014; 23:461–463. PMID: 23632404.
21. Ornek N, Apan A, Ornek K, Gunay F. Anesthetic effectiveness of topical levobupivacaine 0.75% versus topical proparacaine 0.5% for intravitreal injections. Saudi J Anaesth. 2014; 8:198–201. PMID: 24843332.

22. Moisseiev E, Regenbogen M, Bartfeld Y, Barak A. Evaluation of pain in intravitreal bevacizumab injections. Curr Eye Res. 2012; 37:813–817. PMID: 22667326.

23. Segal O, Segal-Trivitz Y, Nemet AY, et al. Anxiety levels and perceived pain intensity during intravitreal injections. Acta Ophthalmol. 2016; 94:203–204. PMID: 26215781.

Table 4
Difference in factors affecting pain score for second intravitreal injection among 3 groups
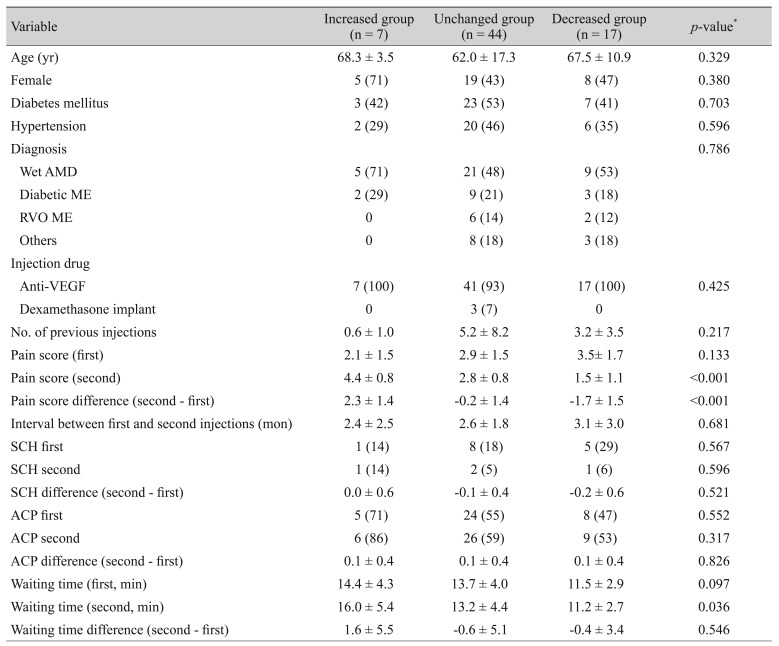
Patients in our study who underwent a second injection were classified into three groups according to change in the degree of pain of the second injection compared to the first; Values are presented as mean ± standard deviation or number (%).
AMD = age-related macular degeneration; ME = macular oedema; RVO = retinal vein occlusion; VEGF = vascular endothelial growth factor; first = first injection; second = second injection; SCH = subconjunctival haemorrhage; ACP = anterior chamber paracentesis.
*Calculated using one-way analysis of variance.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download