Abstract
Gamma 3 rotation control lag screws (U-blade) are particularly useful when treating rotational and unstable fractures of the proximal femur. A 93-year-old woman who underwent closed reduction of a trochanteric fracture and internal fixation with a Gamma 3 nail rotation control lag screw. The patient presented with metal failure and U-blade bending following a fall occurring 4 weeks after surgery. Here, we present a case report summarizing removal of the failed lag screw.
Trochanteric fractures account for 10% to 34% of total hip fractures and most occur in elderly patients12). Proximal femur intramedullary nails are frequently used for reduction of trochanteric fractures. Gamma 3 Nail (Trochanteric Nail 170; Stryker Trauma GmbH, Schoenkirchen, Germany) and PFNA (Proximal Femoral Nail Antirotation; Synthes, Paoli, Switzerland) are commonly used options; however, neither are reported to provide improved anti-rotation or cut-out rate outcomes3). The Gamma 3 nail model designed with a U-blade lag screw was developed to provide improved outcomes when treating unstable proximal femur fractures and those at high risk of rotation. However, evidence suggesting improved outcomes with the use of the U-blade lag screw compared with conventional Gamma 3 nails are limited45).
Complications associated with the use of proximal femur intramedullary nails are intraoperative fractures, cut-out and pull-out, cut through of the lag screw and postoperative femoral shaft fractures6). We recently experienced a loss of reduction with bent U-clip within lag screw following a slip and fall four weeks after treatment of a stable trochanteric fracture, AO/OTA type A1.2, with Gamma 3 nail U-blade lag screw. Here, we describe the removal of the failed U-blade lag screw and pertinent literature.
The patient and her family were informed that this case would be submitted for publication. The fracture pattern was a stable AO/OTA type A1.2 fracture (Fig. 1). The patient had a past medical history of asthma, hypertension, and had previously undergone a total hysterectomy. Previous ambulatory ability was Koval grade 1 (independent ambulator) before she fell from a ground height. The patient's height was 140 cm and she weighed 48 kg (body mass index, 24.5 kg/m2). T-score was −3.5 on the bone mineral density test, and there was no previous treatment for osteoporosis.
The patient underwent surgery three days after injury. After spinal anesthesia, the patient was transferred to the fracture table and fixed with U-blade lag screw Gamma 3 nail after closed reduction with a C-arm-guide (Fig. 2). The Gamma 3 nail used was 10 mm in thickness, 170 mm in length, with a 125° angle, 80-mm lag screw and U-blade. Following the operation, the patient was moved to the general ward. The patient started a partial weight bearing physical therapy using a tilt table two days after the operation, and started walking using a standing walker four days after surgery. The patient was discharged to the nursing hospital 14 days after surgery without any complications (e.g., delirium, cardiovascular disease, wound infection). After discharge, she walked independently using walker for a month.
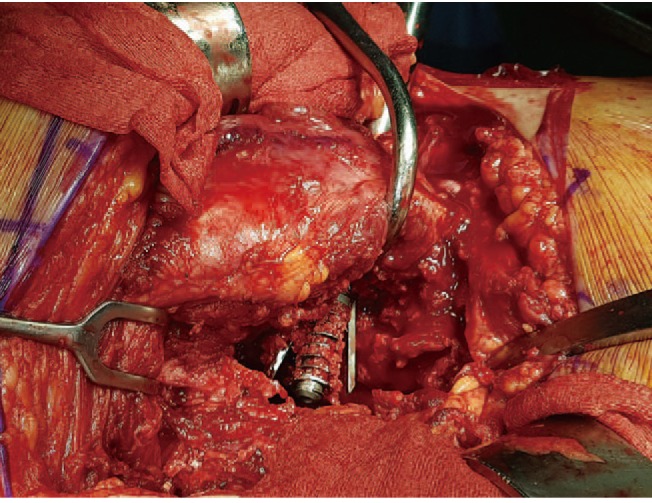
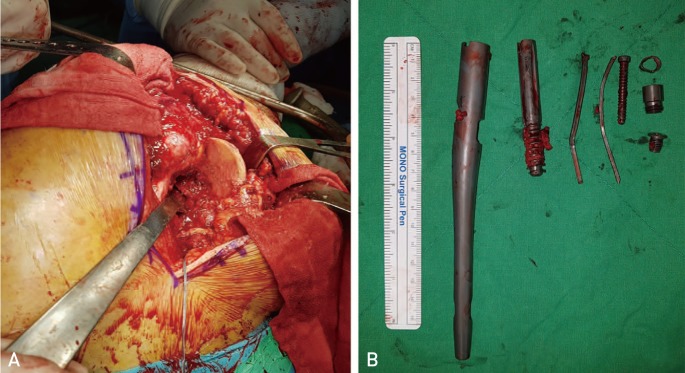
One month after the operation, the patient slipped while using a walker at the nursing hospital, and experienced pain near the site of the previous operation. Simple radiography revealed no breakage of the intramedullary nail and the lag screw, but showed a bent U-blade and loss of proximal femur reduction (Fig. 3). Two days after refracture, metal removal and bipolar hemiarthroplasty were performed. The patient was placed on the lateral position on the operative bed and the femoral head was accessed using a posterior approach. To remove the inserted lag screw and U-blade after reaching the femoral head, the U-blade connector and screw driver were connected. However, the two blades of the U-blade were bent while expanding to both sides, preventing its removal (Fig. 4). The femoral head was cut by saw, but as the lag screw and the proximal portion of the U-blade were inserted from the external cortex of femur, it was difficult to proceed.
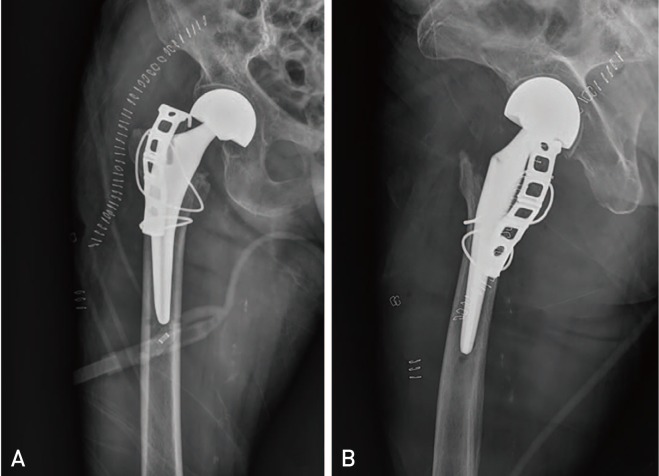
Even after removal of the femoral head by neck cutting, removal of the damaged hardware was possible only after additional separation of the femoral head (Fig. 5). After the previous implant was removed, bipolar hemiarthroplasty was performed using a classical method. Since the refracture occurred while a nail was present, we conducted additional fixation of the femoral stem with a hook plate and a steel wire for added stability (Fig. 6). The patient was admitted to the intensive care unit because of low blood pressure and old age. After about 2 days of delirium, she was transferred to the general ward on the 3rd day after the surgery and her vital signs returned to normal. After 1 week, firm fixation of the surgical site was confirmed using simple radiography and weight bearing was started using the tilt table. Two weeks after the operation, the patient was transferred to the nursing hospital. Follow ups with simple radiographs were performed for 3 months following the surgery. The patient is using a wheelchair and has not experienced any additional complications.
Most trochanteric fractures of the femur occur in elderly patients and require adequate treatment as soon as possible. Proximal femoral intramedullary nails—particularly PFNA and Gamma 3—are the most common choice during surgical treatment, however complications (e.g., cut through and cut-out) have been reported123). Therefore, gamma 3 nails with a U-blade lag screw are used for unstable fractures and high risk patients, but there are no comprehensive studies reporting postoperative outcomes4). The U-blade lag screw is designed to prevent rotation, but no clinical trials describing the risk-benefit profile have been published4). Because of the characteristics of trochanteric fractures, there are many elderly patients and many dependent ambulators. Therefore, postoperative refractures or metal failure must be considered. Trochanteric fractures can fail because of inappropriate axial load of body weight, the relative strengths of hip flexors and external rotators or displacement of fracture fragments. Fixation failure (e.g., metal breakage and nonunion after surgery) are most commonly the result of varus fixation, excessive weight bearing, and stress fracture caused by poor nutrition during recovery1789). Gamma-3 nails are known to have a postoperative fracture rate of 2.0% to 5.7%, in part because of their structural design and material durability. Most postoperative fractures are stress fractures occurring between 6 months and 10 months1810). When fixation failures occur because of metal breakage, additional internal fixation (e.g., replacement of lag screw or nail with a long intramedullary nail, arthroplasty after removal of the broken nail) is necessary. In these cases, U-clip failure makes it difficult to remove the failed lag screw by the normal method (i.e., with the Gamma 3 U-blade connector), thus other surgical instruments are used. We cut the one bent leg of the U blade and extracted the remaining elements of the U-blade using a vise grip. Failure and removal of the Gamma 3 lag screws have been reported8910). For our case, the patient's T-score was as low as −3.5; however, we believe that metal failure in this case is more similar to a traumatic fracture than stress fracture, and the direction or size of the external force at the time of accident are not known. As a result, there was no metal breakage, but the deviation of the each U-blade occurred in opposite directions, making it impossible to remove it using the normal approach. One leg of the U-blade was engaged within the femoral head and firmly seated, increasing the time required for hardware removal, overall operating time, and led to additional bleeding. Most patients with trochanteric fractures are older in age, therefore patients who undergo reoperation due to fixation failure will have a reduced recovery function. The reoperation may have a significant impact on the overall prognosis for older patients.
Reduction quality and implant positioning are keys to surgical outcomes of trochanteric fracture treatment. In our case, the reduction quality was poor and the tip apex distance is outside of the normal range. The lag screw is too low in the anteroposterior view of X-ray and anterior in the lateral X-ray, so these factors may contribute the lag screw failure. Lag screw failure is suspected if proper reduction and implant positioning are achieved. Additionally, the stem for the conversional arthroplasty should pass 2 inches from the distal screw holes to prevent stress riser fracture, however this was not considered at the time of treatment.
Although U-blades are designed to complement the antirotational force, more detail and appropriate consideration of overall stability should be considered when treating patients with similar conditions. Additionally, proper lag screw positioning and reduction should be ensured.
References
1. Sbiyaa M, El Alaoui A, Admi M, Lahrach K, Marzouki A, Boutayeb F. Intertrochanteric fracture non-unions with implant failure of the gamma nail. Pan Afr Med J. 2016; 23:57. PMID: 27217882.

2. Queally JM, Harris E, Handoll HH, Parker MJ. Intramedullary nails for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2014; (9):CD004961. PMID: 25212485.

3. Yang YH, Wang YR, Jiang SD, Jiang LS. Proximal femoral nail antirotation and third-generation Gamma nail: which is a better device for the treatment of intertrochanteric fractures? Singapore Med J. 2013; 54:446–450. PMID: 24005451.

4. Lang NW, Arthold C, Joestl J, et al. Does an additional antirotation U-Blade (RC) lag screw improve treatment of AO/OTA 31 A1-3 fractures with gamma 3 nail? Injury. 2016; 47:2733–2738. PMID: 27832831.

5. Yaozeng X, Dechun G, Huilin Y, Guangming Z, Xianbin W. Comparative study of trochanteric fracture treated with the proximal femoral nail anti-rotation and the third generation of gamma nail. Injury. 2010; 41:1234–1238. PMID: 21374904.

6. Park BJ, Cho HM, Kim JH, Sin WJ. Excessive sliding of the helical blade and the femoral neck fracture after insertion of proximal femoral nail anti-rotation for type A2 intertrochanteric fractures: a case report. J Korean Fract Soc. 2013; 26:151–155.
7. Gaebler C, Stanzl-Tschegg S, Tschegg EK, et al. Implant failure of the gamma nail. Injury. 1999; 30:91–99. PMID: 10476276.

8. Iwakura T, Niikura T, Lee SY, et al. Breakage of a third generation gamma nail: a case report and review of the literature. Case Rep Orthop. 2013; 2013:172352. PMID: 23762698.

9. Tantigate D, Riansuwan K, Mahaisavariya B, Sukjaitham K. Breakage of a lag screw of cephalomedullary nail: a technique of removal. Clin Orthop Surg. 2015; 7:261–263. PMID: 26217475.

10. Wee JL, Sathappan SS, Yeo MS, Low YP. Management of gamma nail breakage with bipolar hemi-arthroplasty. Singapore Med J. 2009; 50:e44–e47. PMID: 19224071.
Fig. 2
(A) Radiograph immediately following surgery indicates good reduction quality. (B) Cross table lateral view.

Fig. 3
(A) Reduction loss is observed in the anteroposterior plane X-ray scan. (B) U-blade is bent in the femoral head in the cross table lateral view.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download