Abstract
A 62-year-old man underwent endoscopic mucosal resection for early gastric cancer. The follow-up computed tomography revealed biliary dilatation. The tumor was located in the lower bile duct with biliary dilatation, and no evidence of metastasis in other organs was noted. The patient underwent subtotal stomach-preserving pancreatoduodenectomy with pancreaticogastrostomy and Billroth I anastomosis. At 13 months after the operation, gastrointestinal endoscopy revealed a tumor lesion in the pancreaticogastrostomy site. Computed tomography revealed that the lesion was low enhanced in the pancreaticogastrostomy site and there was no evidence of other distant metastasis. Partial pancreatectomy was performed. Pathological findings of the tumor in the stump of the pancreas revealed findings similar to that of primary biliary carcinoma. Apparently, the patient was diagnosed with recurrence of bile duct cancer via the pancreatic duct. The patient underwent adjuvant chemotherapy for one year subsequent to partial pancreatectomy as the second operation. For 40 months after the second operation, there has been no evidence of recurrence of cancer.
Biliary cancer is rare and often presents with aggressive malignancy. This cancer includes four distinct categories such as intrahepatic cholangiocarcinoma, extrahepatic cholangiocarcinoma, gallbladder cancer, and ampullary carcinoma. Complete surgical resection is the only treatment option for patients. However, even if curative intent surgery is applied to the resectable biliary cancer patients, the 5-year survival rates still remain low: 33.1% for bile duct cancer, 52.8% for ampullary cancer, and 41.6% for gallbladder cancer.1 The high rate of recurrence is the reason behind poor prognosis in biliary cancer. However, treatment for recurrent cancer such as chemotherapy is not sufficient. Therefore, surgery is needed for recurrent biliary tract cancer in resectable cases. We report a rare case of advanced bile duct cancer with long-term survival by repeated resection due to recurrence in the pancreaticogastrostomy site after subtotal stomach-preserving pancreatoduodenectomy (SSPPD).
The patient was a 62-year-old man who underwent endoscopic mucosal resection for early gastric cancer nine years ago and follow-up computed tomography revealed biliary dilatation.
The physical examination at the time of admission showed no abnormal findings. Serum liver enzyme levels were on a slightly higher side and other laboratory findings were normal.
Abdominal computed tomography (CT) revealed a tumor in the lower bile duct with biliary dilatation (Fig. 1), and no evidence of metastasis in other organs was noted. The tumor was low intensity at T1WI, iso-high intensity at T2WI, and high intensity at the diffusion-weighted image in magnetic resonance imaging (MRI) findings (Fig. 2). Biliary dilatation and filling defect of the lower bile duct were found in magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP) (Fig. 3). MRCP and ERCP revealed no abnormal findings in the pancreatic duct. Cytology of the bile juice was malignant cell-negative. Therefore, we performed subtotal stomach-preserving pancreatoduodenectomy (SSPPD, Pancreaticogastrostomy, Billroth I) (Fig. 4). The proximal 2 cm of the pancreatic remnant is dissected from the retroperitoneum and anastomosed end-to-side to the posterior wall of the stomach. With the suturing and tying, 1 cm of the pancreas was invaginated into the stomach. We sutured the pancreatic parenchyma and the seromuscular layer of the stomach at 2 cm radius from the pancreatic duct. The pathological findings revealed bile duct cancer of T2N0M0 StageIIA (TNM staging by the International Union Against Cancer [UICC] 7th edition), and there was no evidence of cancer invasion into the pancreatic duct. In addition, the perineural/lymphatic invasion was not observed.
On the 16th day after the operation, hematemesis occurred. Gastrointestinal endoscopy revealed blood coagulation in the stomach, but there was no obvious bleeding in the stomach. In angiography, development of pseudoaneurysm of the stump of the gastroduodenal artery was observed and extravasation was confirmed. Therefore, coil embolization of the common hepatic artery was performed. After the treatment, the patient recovered and was discharged from the hospital.
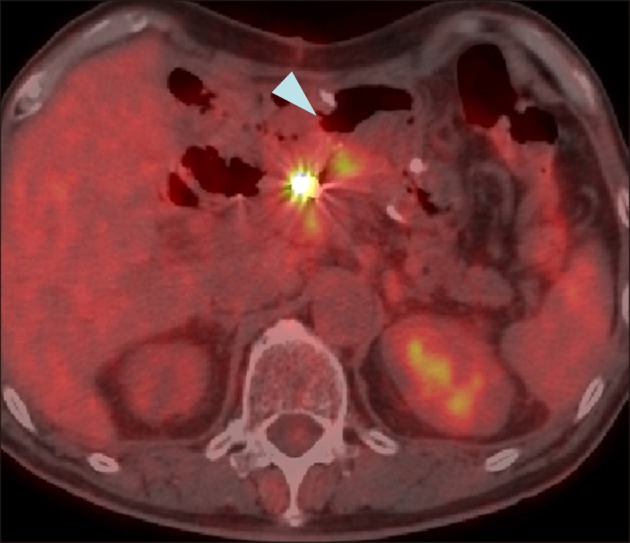
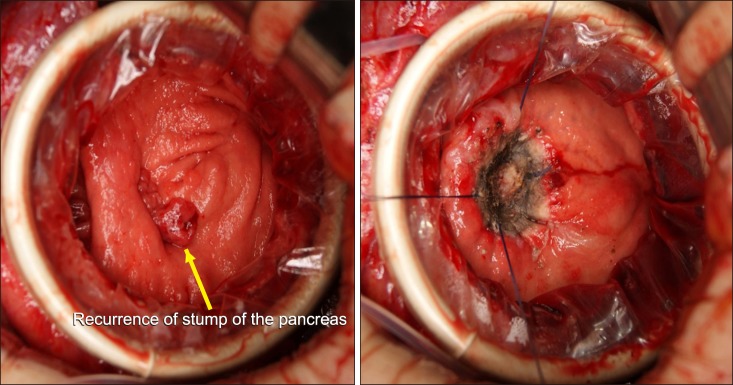
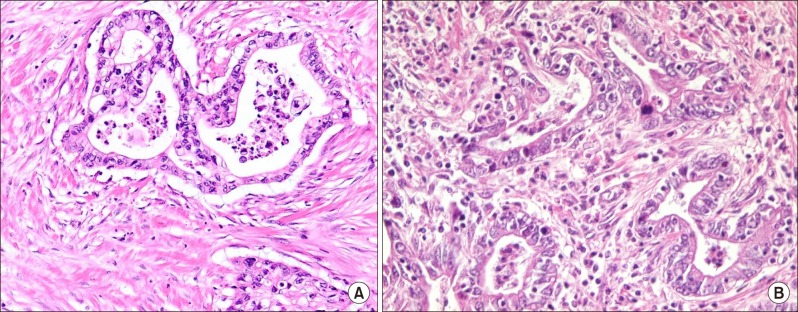
At 13 months after the operation, gastrointestinal endoscopy revealed an irregular shaped tumor in the pancreaticogastrostomy site and endoscopic biopsy revealed a well-differentiated tubular adenocarcinoma (Fig. 5). The lesion was low enhanced in the pancreaticogastrostomy site in CT scan. The lesion also showed the accumulation of fluorodeoxyglucose in positron emission tomography CT (Fig. 6). Although no changes in the level of serum tumor marker were noted. There was no evidence of other distant metastasis. The patient was diagnosed as having a recurrence of cholangiocarcinoma and a second surgery was performed. Partial pancreatectomy was performed from the opened anterior wall of the stomach (Fig. 7). The surgical margin of pancreatic duct was tumor-negative in intraoperative diagnosis. Pathological findings revealed atypical cells with abnormal karyotype and increased chromatin condensation. Pathological findings of the tumor in the stump of the pancreas revealed findings similar to that of primary biliary carcinoma. Consequently, the patient was diagnosed with recurrence of the bile duct cancer as well differentiated tubular adenocarcinoma (Fig. 8). The patient underwent chemotherapy of Tegafur/Gimeracil/Oteracil (TS-1) as adjuvant chemotherapy for bile duct cancer for one year after the second operation. For 40 months after the second operation, there has been no evidence of recurrence of cancer.
Biliary tract cancer is a rare malignancy associated with poor prognosis and complete surgical resection is the only curable treatment. However, biliary tract cancer patients are often diagnosed with advanced stages and treated employing systemic chemotherapy or palliative treatment settings rather than curative surgery.
In general, patients with recurrent biliary cancer are treated using various chemotherapies. Some clinical trials provided a certain degree of clinical benefit to patients; however, the results are not satisfactory.23 Regarding surgical treatment for the recurrence of extrahepatic biliary carcinoma, few reports have reported surgical indication. If it is considered in resectable, surgery appears to be feasible for recurrent extrahepatic biliary carcinoma and offers longer survival.45
Pancreaticogastrostomy is one of the methods of reconstruction after pancreaticoduodenectomy. When compared with pancreaticojejunostomy, pancreaticogastrostomy did not show any significant differences in the overall postoperative complication rate or reduction of pancreatic fistula. However, biliary fistula, postoperative collections, and delayed gastric emptying were significantly reduced in patients treated with pancreaticogastrostomy. In addition, pancreaticogastrostomy is associated with a significantly lower frequency of multiple surgical complications.678910 There exist several reports on pancreatic fistula, however, only a few reports have dealt with cancer recurrence after pancreaticogastrostomy. In our case, recurrence occurred in the anastomosed site of pancreaticogastrostomy. As the resected pancreatic duct was normal, it was hypothesized that the recurrent lesion was disseminated via the pancreatic duct. This type of metastasis is a very rare case. As far as we examined, no similar case was not found. The lesion was localized, and no evidence of other metastasis was observed, therefore, we performed the second operation. It was considered that curative resection was succeeded by partial pancreatectomy, but total pancreatectomy was difficult due to adhesion by the first operation. Pancreaticogastrostomy was identified as a useful method due to ease of observation of the anastomosed site by endoscopy and easy approach to the anastomosed site during the operation.
We report a rare case of advanced bile duct cancer with long-term survival by repeated resection of recurrence in the pancreaticogastrostomy site after SSPPD. Reoperation should be considered for accurate diagnosis for location and format of recurrence.
References
1. Miyakawa S, Ishihara S, Horiguchi A, Takada T, Miyazaki M, Nagakawa T. Biliary tract cancer treatment: 5,584 results from the Biliary Tract Cancer Statistics Registry from 1998 to 2004 in Japan. J Hepatobiliary Pancreat Surg. 2009; 16:1–7. PMID: 19110652.

2. Takashima A, Morizane C, Ishii H, Nakamura K, Fukuda H, Okusaka T, et al. Randomized phase II study of gemcitabine plus S-1 combination therapy vs. S-1 in advanced biliary tract cancer: Japan Clinical Oncology Group Study (JCOG0805). Jpn J Clin Oncol. 2010; 40:1189–1191. PMID: 20630899.

3. Valle JW. Advances in the treatment of metastatic or unresectable biliary tract cancer. Ann Oncol. 2010; 21(Suppl 7):vii345–vii348. PMID: 20943640.

4. Song SC, Heo JS, Choi DW, Choi SH, Kim WS, Kim MJ. Survival benefits of surgical resection in recurrent cholangiocarcinoma. J Korean Surg Soc. 2011; 81:187–194. PMID: 22066120.

5. Noji T, Tsuchikawa T, Mizota T, Okamura K, Nakamura T, Tamoto E, et al. Surgery for recurrent biliary carcinoma: results for 27 recurrent cases. World J Surg Oncol. 2015; 13:82. PMID: 25884694.

6. Ishikawa O, Ohigashi H, Eguchi H, Yokoyama S, Yamada T, Takachi K, et al. Long-term follow-up of glucose tolerance function after pancreaticoduodenectomy: comparison between pancreaticogastrostomy and pancreaticojejunostomy. Surgery. 2004; 136:617–623. PMID: 15349110.

7. Que W, Fang H, Yan B, Li J, Guo W, Zhai W, et al. Pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy: a meta-analysis of randomized controlled trials. Am J Surg. 2015; 209:1074–1082. PMID: 25743406.
8. Bassi C, Falconi M, Molinari E, Salvia R, Butturini G, Sartori N, et al. Reconstruction by pancreaticojejunostomy versus pancreaticogastrostomy following pancreatectomy: results of a comparative study. Ann Surg. 2005; 242:767–771. discussion 771–773. PMID: 16327486.
9. Fernández-Cruz L, Cosa R, Blanco L, López-Boado MA, Astudillo E. Pancreatogastrostomy with gastric partition after pylorus-preserving pancreatoduodenectomy versus conventional pancreatojejunostomy: a prospective randomized study. Ann Surg. 2008; 248:930–938. PMID: 19092337.
Fig. 1
Computed tomography findings showing tumor of the lower bile duct with biliary dilatation (arrow).

Fig. 2
Magnetic resonance imaging showed that the tumor was low intensity at T1WI, iso-high intensity at T2WI and high intensity at diffusion-weighted image (DWI) (arrows).

Fig. 3
Magnetic resonance cholangiopancreatography findings. (A) Biliary dilatation and filling defect of lower bile duct were observed. (B) No abnormality in the pancreatic duct was observed.
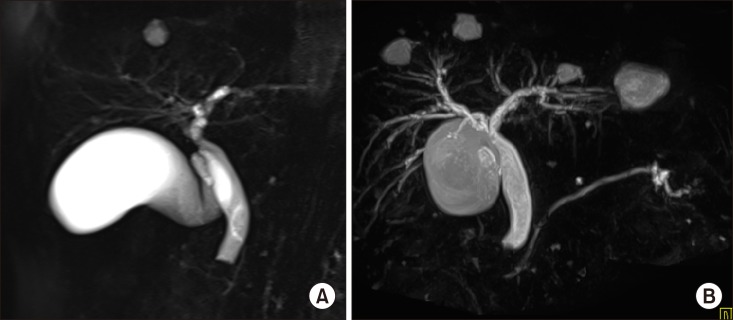
Fig. 4
Operative finding of the first operation. (A) Surgical findings of the pancreaticogastric anastomosis in the first operation (white arrow). (B) Transgastric pancreaticogastric anastomosis was performed. The pancreaticogastric anastomosis was made using full-thickness sutures of the stomach to the pancreas. Subsequently, gastrojejunectomy was performed using Billroth I method.
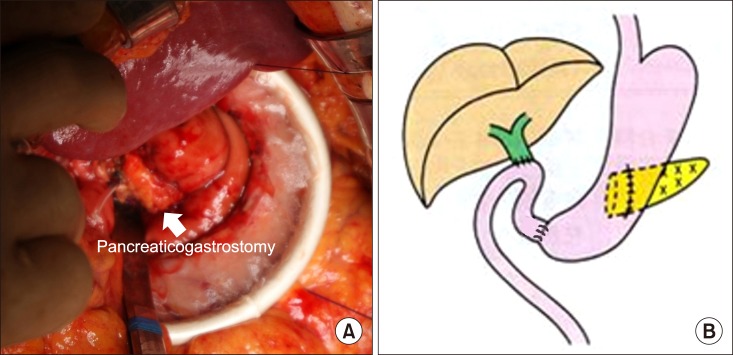
Fig. 5
Gastrointestinal endoscopy finding after 13 months of first operation: the recurrence at pancreaticogastrostomy site was noted.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download