Abstract
Traumatic diaphragmatic rupture (TDR) is uncommon, and may be associated with other severe life-threatening injuries after blunt trauma. Recently, we experienced a right-sided TDR patient with other multiple life-threatening injuries. A 59-year-old female inflicted with a right-sided TDR accompanied by herniated liver was treated with thoracoscopic exploration. We successfully managed associated life-threatening injuries such as traumatic brain injury and pelvic bone fractures with bleeding, simultaneously.
Traumatic diaphragmatic rupture (TDR) is uncommon with incidence ranging from 1% to 7% in blunt trauma patients, and 10% to 15% in penetrating trauma patients, and the side of diaphragmatic rupture correlates with the direction of impact [123]. TDR is almost always accompanied by other severe injuries that are associated with higher mortality and morbidity. Recent improvements of modern radiologic devices have allowed for an easier diagnosis of TDR. Nevertheless, missed diagnosis is frequently reported, because TDR is often asymptomatic or ignored [4]. This is why trauma surgeons must have a high index of suspicion for patients with an incidence associated with risk of TDR. We experienced and here present a case of right-sided TDR in a patient with other multiple life-threatening injuries. We then discuss the clinical implications of high index of suspicion for patients with an incidence associated with TDR.
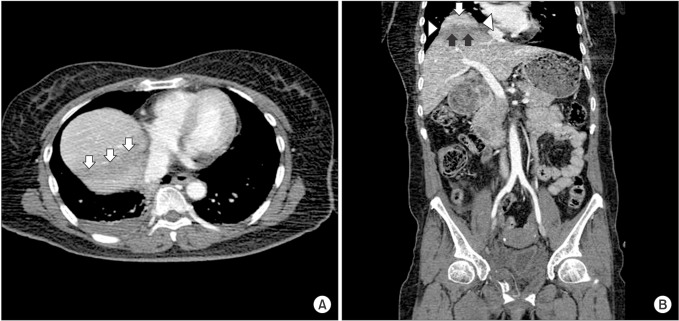
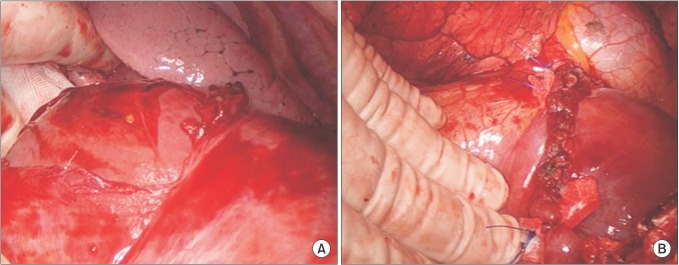
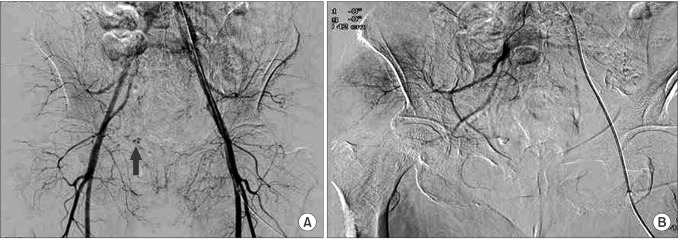
A 59-year-old female patient presented to our Emergency Department (ED) semicomatose. Her vital signs were: blood pressure at 70/50 mmHg, heart rate at 113 beats per minute, respiratory rate 24 per minute, and body temperature at 36.0℃ with peripheral O2 saturation at 92%. The incident was a pedestrian traffic accident that occurred 30 minutes prior to arrival at ED. After crystalloid resuscitation, systolic blood pressure recovered to 110 mmHg, and she showed irritability with drowsiness. We had performed primary and secondary surveys after intubation with sedation. Initial chest radiology findings showed elevated liver enzymes (Fig. 1), and pelvis radiology findings showed fractures in both superior and inferior rami. The patient underwent CT scans of brain, c-spine, chest, abdomen, and pelvis with intravenous contrast. The brain CT showed a small amount of intraventricular hemorrhage (IVH) in the left lateral ventricle. Enhanced chest CT showed a small amount of right-sided hemothorax with focal right upper lobe contusion, and there was no evidence of rib fracture. Enhanced abdomen and pelvic CT (APCT) showed multiple pelvic bone fractures including left sacral ala along with focal extravasation of contrast media at right aspect of the pelvic cavity. After seeing coronal images of APCT, we were able to strongly doubt TDR. The axial images showed an area of hypoattenuation in the dome of the liver (Fig. 2A), whereas the coronal images showed herniation of the liver dome through a diaphragmatic rupture (hump sign) with waist-like constriction of the liver (collar sign), and linear area of subtle hypoattenuation (band sign) from the coronal view of APCT showing elevation of liver (Fig. 2B). The 1-hour follow-up brain CT identified new subdural hematoma along the falx and tentorium cerebella. The neurosurgeon decided to only observe because its amount was small and IVH was not increased. The patient showed hemodynamic instability after secondary survey, and laboratory findings showed declining of serum hemoglobin from 12.2 to 9.2 g/dL. She was immediately treated with blood transfusion and started on an inotropic infusion to maintain blood pressure after which she was transferred to the operating room for thoracoscopic exploration. The operative findings were: (1) 15-cm diaphragmatic laceration in the anterolateral aspect from the inferior pericardium, (2) herniation of the liver and no evidence of liver laceration, and (3) bleeding from the soft tissue of the mediastinum and lacerated diaphragm (Fig. 3A). Diaphragm repair was done by interrupted pledgeted sutures of Prolene 2-0, and operation was adjourned after bleeding control and chest tube insertion (Fig. 3B). The operation time was 1 hour, and after that, immediate angiography was performed. Extravasation of contrast media was identified at the anterior branch of the right internal iliac artery, which was embolized successfully (Fig. 4). Although she remained hemodynamically stable, she was admitted to the intensive care unit (ICU) for ventilator care and hemodynamic monitoring. Ventilator weaning was done three days after operation. After managing her right pleural effusion, she was transferred to the general ward ten days after operation. Pelvic bone fractures were treated conservatively with bed rest, and 1 month later she was transferred to the rehabilitation department.
This study was waived by the Institutional Review Board.
The most common cause of TDR is blunt thoracoabdominal trauma, such as road traffic accidents and falls from heights [5]. TDR is thought to be produced by a sudden increase in the pleuroperitoneal pressure gradient, probably occurring at areas of congenital weakness, the left side of the diaphragm [1]. However, other studies have found no evidence for congenital weakness [6]. It was reported that this is probably due to the protective effect of the liver by the right hemidiaphragm in blunt trauma, and the fact that most people use their right hand for protection against penetrating trauma [7]. As mentioned above, the side of the diaphragmatic rupture correlates with the direction of impact [3]. In this case, although the patient was inflicted with right-sided TDR, we could not determine the direction of impact due to insufficient medical records.
TDR usually requires incidence of high-energy compression; hence associated injuries being common. Traumatic brain injury (TBI) is most common, presenting in half of the patients and is one of the predictors for mortality [1]. Other associated injuries include pelvic bone fractures, long bone fractures, and rib fractures. Intrathoracic injuries include pneumothorax, pulmonary contusion, lung lacerations, blunt cardiac injury, and aortic rupture [168]. Intra-abdominal injuries include solid organ injury such as liver, spleen, and hollow-viscus injuries [468]. This patient had SDH, IVH, and pelvic bone fractures with bleeding in the branch of the internal iliac artery. Her TBI was only observed because the hemorrhage, fortunately, did not increase. She also had pelvic bone fractures with internal bleeding. Her blood pressure was well managed by fluid resuscitation, transfusion, and inotropics. Thoracoscopy was decided on first rather than angio-embolization. Other intrathoracic injuries such as lung laceration, blunt cardiac injury, or aortic ruptures were not identified during operation, thus we could achieve a short operative time by primary repair of the ruptured diaphragm. After operation, immediate angio-embolization was performed successfully, maintaining hemodynamic stability.
TDR is difficult to diagnose because it is often asymptomatic, or the presentation is often dominated by other symptoms from associated injuries. Recent studies, show that helical CT and multislice CT, such as 64-slice multidetector row spiral CT (64-MDCT), may allow better demonstration of most subtle signs of diaphragmatic injury with high sensitivity, specificity, and accuracy [9]. Nineteen suggestive of TDR by CT images have been described in the radiologic study. The useful features of right-sided TDR seen on MDCT scan are thickened diaphragm, hump, and band signs from herniation of the liver [10]. Segmental diaphragmatic defect, herniation through a defect, Collar sign (waistlike constriction of the herniated structure at the site of the diaphragmatic rupture) are more useful features of left-sided TDR than right-sided TDR [9]. Nevertheless, trauma surgeons should always have a high index of suspicion in blunt thoraco-abdominal injury patients, and obtain detailed information about the mechanism of injury.
Traditionally, laparotomy approach was preferred for the acute TDR because it allowed better exposure of associated intra-abdominal injuries. Thoracotomy is indicated in cases of late diaphragmatic hernia, isolated lesions of the right diaphragm and in cases of suspicion of intrathoracic injury. Minimally invasive surgery to repair TDR has advantages over open surgery in that it provides good surgical view, is minimally invasive, promotes early recovery, and decreases hospital stay. Hemodynamically stable TDR patients without significant associated injuries may be indicated by minimally invasive surgery [410]. Our patient was operated on with thoracoscopy due to right liver herniation without associated intra-abdominal organ injuries. Thoracoscopy could be a treatment option in cases of one-sided TDR and patients with no other associated intra-abdominal injuries.
We experienced and presented a case of a right-sided TDR patient with other multiple life-threatening injuries. TDR is often difficult to diagnose and is associated with life-threatening injuries. Trauma surgeons must have a high index of suspicion for patients with incidence associated with risk of TDR.
References
1. Hanna WC, Ferri LE. Acute traumatic diaphragmatic injury. Thorac Surg Clin. 2009; 19:485–489. PMID: 20112631.

2. Scharff JR, Naunheim KS. Traumatic diaphragmatic injuries. Thorac Surg Clin. 2007; 17:81–85. PMID: 17650700.

3. Kearney PA, Rouhana SW, Burney RE. Blunt rupture of the diaphragm: mechanism, diagnosis, and treatment. Ann Emerg Med. 1989; 18:1326–1330. PMID: 2589701.

4. Thiam O, Konate I, Gueye ML, Toure AO, Seck M, Cisse M, et al. Traumatic diaphragmatic injuries: epidemiological, diagnostic and therapeutic aspects. Springerplus. 2016; 5:1614. PMID: 27652187.

5. Vermillion JM, Wilson EB, Smith RW. Traumatic diaphragmatic hernia presenting as a tension fecopneumothorax. Hernia. 2001; 5:158–160. PMID: 11759804.

6. Andrus CH, Morton JH. Rupture of the diaphragm after blunt trauma. Am J Surg. 1970; 119:686–693. PMID: 5445992.

7. Eren S, Ciris F. Diaphragmatic hernia: diagnostic approaches with review of the literature. Eur J Radiol. 2005; 54:448–459. PMID: 15899350.

8. Rodriguez-Morales G, Rodriguez A, Shatney CH. Acute rupture of the diaphragm in blunt trauma: analysis of 60 patients. J Trauma. 1986; 26:438–444. PMID: 3701892.

9. Dwivedi S, Banode P, Gharde P, Bhatt M, Ratanlal Johrapurkar S. Treating traumatic injuries of the diaphragm. J Emerg Trauma Shock. 2010; 3:173–176. PMID: 20606795.

10. Ties JS, Peschman JR, Moreno A, Mathiason MA, Kallies KJ, Martin RF, et al. Evolution in the management of traumatic diaphragmatic injuries: a multicenter review. J Trauma Acute Care Surg. 2014; 76:1024–1028. PMID: 24662867.
Fig. 2
(A) Abdomen and pelvic CT (APCT) shows an area of hypoattenuation in the dome of the liver (arrows). (B) APCT shows herniation of liver dome through a diaphragmatic rupture (white arrow, hump sign), waistlike constriction of liver (arrowhead, collar sign), and linear area of subtle hypoattenuation (black arrows, band sign).




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download