INTRODUCTION
Spindle epithelial tumor with thymus-like differentiation (SETTLE) is a very rare tumor of the thyroid gland which occurs predominantly in young patients [
12]. It is thought to develop from ectopic thymic tissue or remnants of branchial pouches [
1]. Furthermore, it is considered a low grade malignant neoplasm due to its indolent clinical course [
3]. Metastasis has been documented in several case reports and close follow-up is important in clinical management [
34]. Herein, we report a case of the oldest patient so far. The clinicoradiopathological features of reported cases in the English literature have also been reviewed.
Go to :

CASE REPORT
A 70-year-old man was referred to Korea University Anam Hospital with a large painless mass in the right neck. The mass was firstly discovered when the patient visited a local hospital with symptoms of exercise-induced dyspnea. He was taking medication for hypertension and had no history of thyroid disease, or family history of thyroid disease. Informed consent was gotten from the patient and the Institutional Review Board approval was waived.
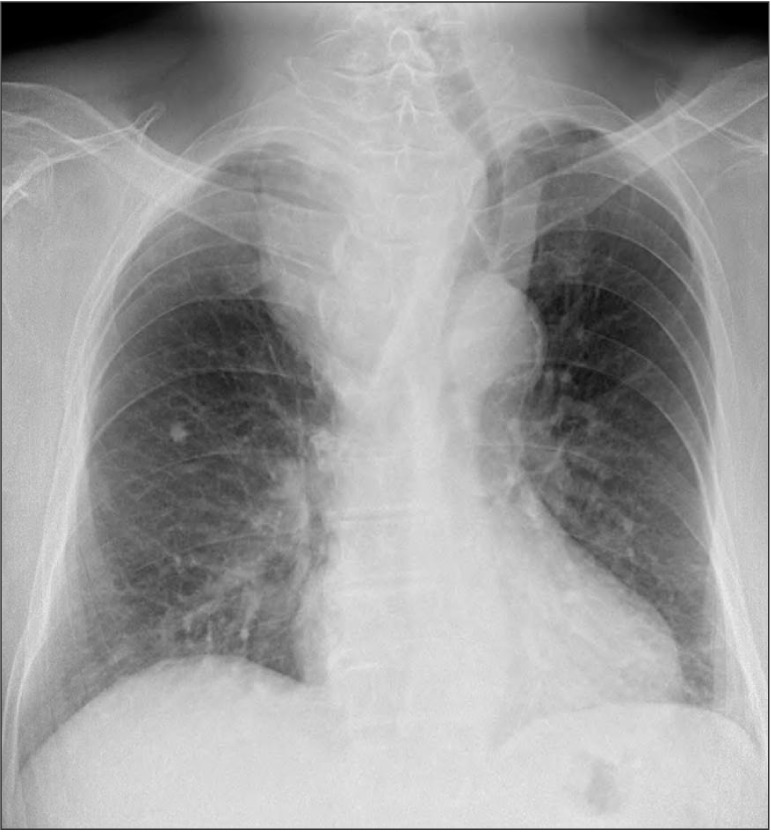
The chest radiography showed tracheal deviation to the left side with mild narrowing of the midtrachea due to the mass in the right lower neck and anterior mediastinum (
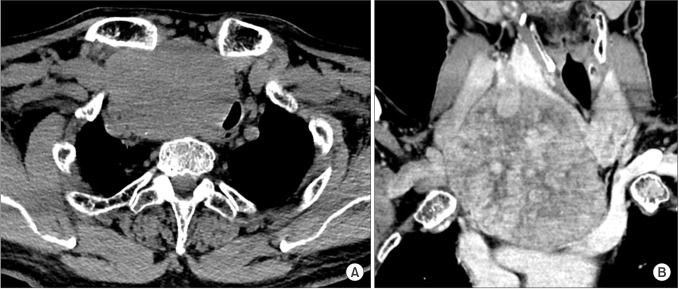
Fig. 1). The CT scan revealed an approximately 8.8 × 9.1-cm-sized heterogeneous enhanced circumscribed mass in the right lower lobe of the thyroid gland with exophytic growth into the mediastinum (
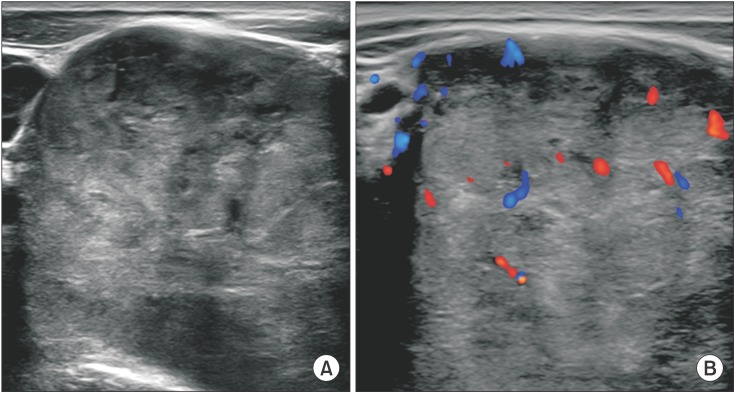
Fig. 2). Tracheal deviation and compression by the mass were also noticed. There was no definite evidence of local invasion to the adjacent structures, including the trachea, large vessels, and mediastinal soft tissue. However, there were two solid nodules in the right and left lower lobes of the lungs, each measuring approximately 1.0 and 1.3 cm, respectively, in size. The lung nodules were considered to be possible metastatic lesions. The mass showed heterogeneous echogenicity with some increased intratumoral vascularity on the ultrasound (
Fig. 3). An ultrasound-guided biopsy revealed that the mass was a spindle cell tumor. Thyroid function tests were normal.
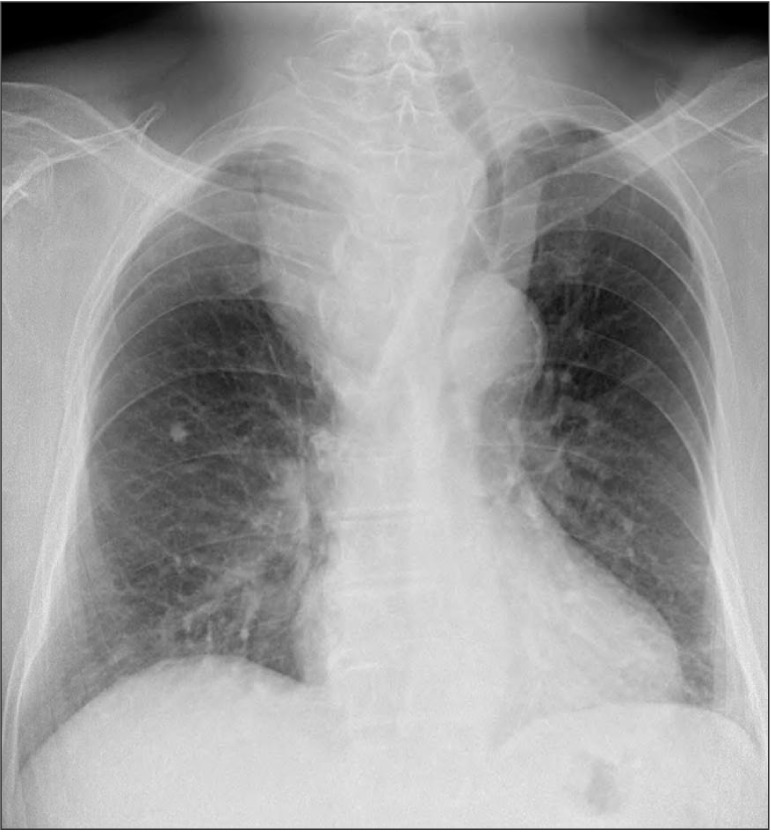 | Fig. 1Chest radiography showing tracheal deviation to left side with narrowing of midtrachea due to mass in right lower neck and anterior mediastinum.
|
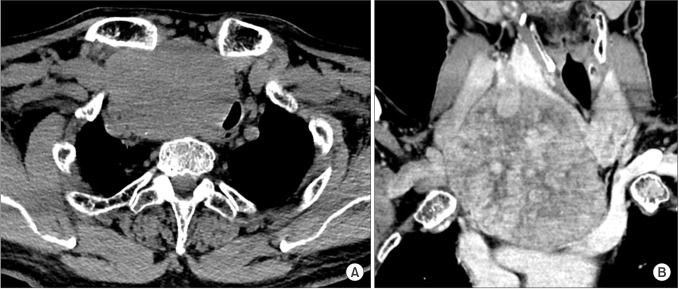 | Fig. 2Axial and coronal view of the mass showing heterogeneous enhancement with displacing trachea to left side and compression to lumen on contrast-enhanced CT (CECT) scan. (A) Axial non CECT revealed bulky mass lesion in the right paratracheal space, displacing the trachea. (B) Coronal reconstructed CECT scan showed a huge mass with heterogenous contrast enhancement and compress the trachea.
|
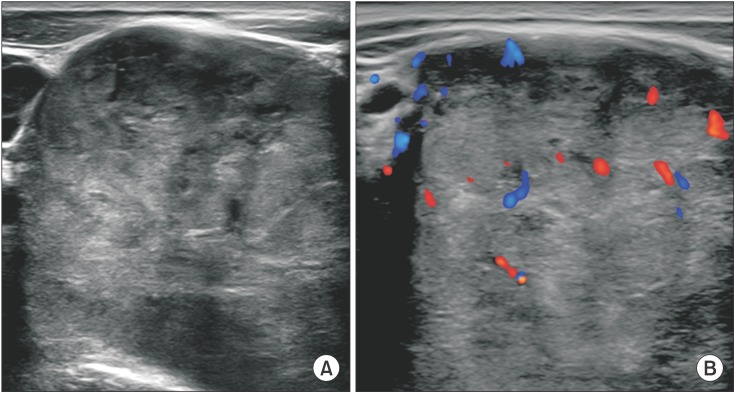 | Fig. 3On ultrasound, mass showed heterogeneous echogenicity and increased vascularity. (A) Transverse neck ultrasound revealed bulky mass with heterogenous echo pattern. (B) On color Doppler application, increased tumor vascular flow was shown.
|
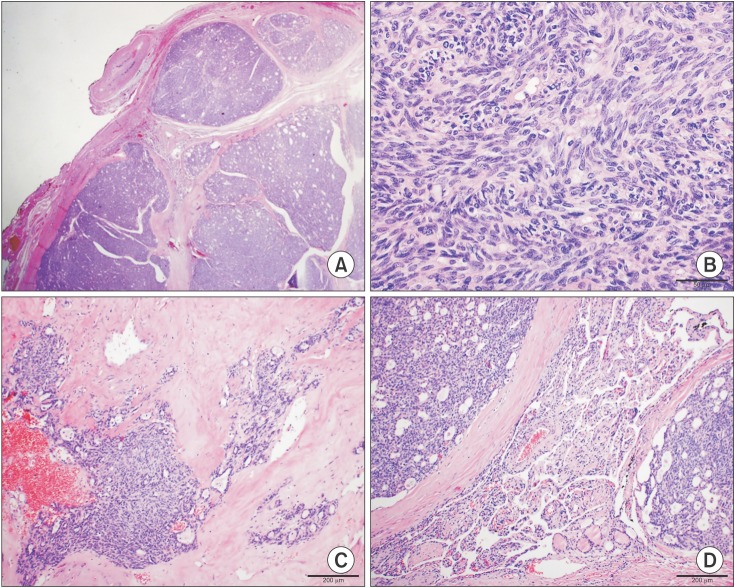
The patient underwent a right lobectomy of the thyroid and mass excision. On the section of the gross specimen, the cut surface showed a well-circumscribed whitish gray solid mass, measuring 9.0 × 8.6 cm. Histological examination showed a totally encapsulated neoplasm traversed by an irregular thin or thick band-like fibrotic tissue. The tumor had a biphasic pattern which was composed of predominantly solid dense groups of spindle cells and small quantities of intermixed epithelial components. The uniform plump spindle cells were arranged in tight streaming short fascicular patterns with occasional microcystic changes (
Fig. 4A). These cells had elongated cigar-shaped nuclei with fine chromatin, and scant to moderate quantity of pale eosinophilic cytoplasm. Nuclear atypism, prominent nucleoli, and mitotic figures were very rare (
Fig. 4B). Sparse epithelial components were occasionally observed, particularly in the more sclerotic area at the center of the tumor. These cells were flat to cuboidal epithelial cells forming tubulocystic structures and merged imperceptibly with the spindle cell components (
Fig. 4C). Lymphoplasmacytic infiltration was rarely observed in the peripheral areas and no TdT-positive lymphocytes were revealed. In the peripheral areas, one small focus of entrapped normal thyroid follicles and several foci of papillary endothelial hyperplasia of blood vessels were observed (
Fig. 4D). Several foci of vascular invasion in the tumoral capsule were also observed. On immunostaining, the tumor cells were positive for pan-cytokeratin, CAM 5.2, p63, Bcl-2, and CD99, and negative for CD5, c-kit, and TTF-1. The final pathological diagnosis was spindle epithelial tumor with thymus-like differentiation (SETTLE). Follow-up chest CT scans after 3 and 6 months revealed no local recurrence or interval growth of the lung nodules in either lower lobe.
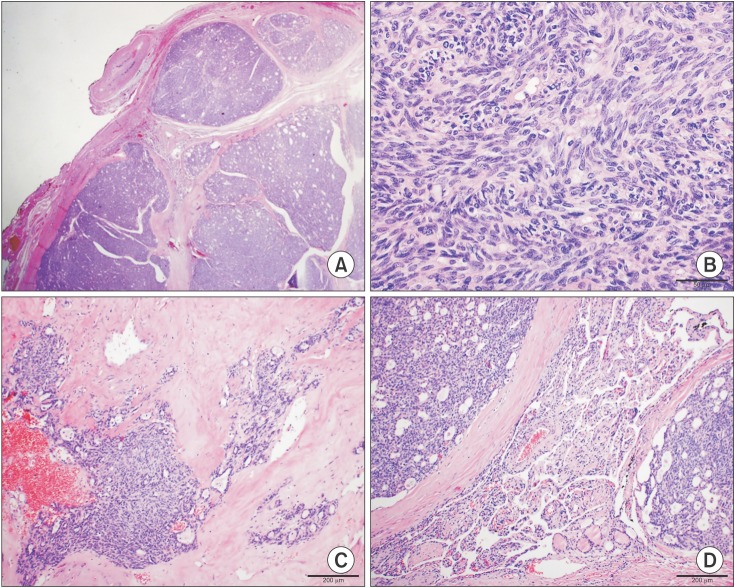 | Fig. 4Microscopic findings of the tumor of H&E stain. (A) An encapsulated multilobular tumor traversed by fibrous band is seen on low power field (×12.5). (B) On high power field (×400), tumor cells were uniformly plump spindle cells with elongated nuclei and arranged in short fascicular pattern. (C) Spindle cell component merged into epithelial component with tubulocystic configuration in central area. (D) Entrapped normal thyroid follicles (lower center) were observed in peripheral areas of tumor.
|
Go to :

DISCUSSION
Spindle epithelial tumor with thymus-like differentiation (SETTLE) is a very rare malignant thyroid tumor, described by Chan and Rosai [
1] as tumors demonstrating thymic or related branchial pouch differentiation. It has been previously reported as a “thyroid spindle cell tumor with mucous cyst,” a “malignant teratoma,” a “thyroid thymoma in childhood,” and an “unusual thyroid tumor in a child” [
256]. Painless neck mass is the first clinical presentation for the majority of patients. There was only one reported case with tracheal compression at presentation [
1]. According to the reported cases, SETTLE tumors measure between 0.5 and 12 cm [
7]. They typically occur in children, adolescents, and young adults. The present case of a 70-year-old man is the oldest patient reported so far.
SETTLE is considered to be a low grade malignant neoplasm due to its indolent growth, protracted clinical course, and tendency to develop delayed blood-borne metastasis [
8]. Owing to this tendency, long-term follow-up following the treatment of the lesion is essential and close attention is required at the time of the initial diagnosis. There are 2 case reports of metastasis developed over more than 20 years following the initial diagnosis [
9]. The latency between diagnosis and detection of metastasis varies from a few months after the primary tumor manifestation to 25 years [
910]. Ippolito et al. [
7] proposed that neck ultrasound, chest radiography, CT, and MRI should be performed annually, despite the absence of specific symptoms. Metastatic spread was reported to the lungs, mediastinum, local lymph nodes, and kidney. The most common site of metastasis is thought to be the lungs [
359].
Histologically, SETTLE tumors predominantly consist of spindle cells of epithelial nature which form fascicles, merging into glandular structures, and taking the form of tubules, papillae, and cystic spaces. In certain cases, there may be cysts or glands lined by mucinous or respiratory epithelium. Residual thyroid follicles are sometimes entrapped within the tumor. Immunohistochemistry is essential for the diagnosis of SETTLE and it is typically positive for the epithelial markers of cytokeratin and vimentin, seldom positive for the smooth muscle actin marker and negative for the follicular thyroid markers (thyroglobulin and TTF1), CEA, S-100 protein and the C-cell marker calcitonin [
710]. Fine needle aspiration biopsy (FNAB) is a quick and minimally invasive method used in preoperative diagnosis of tumors. In SETTLE tumors, all descriptions of FNAB show a highly cellular aspirate primarily composed of cohesive or isolated sheets of spindle cells.
The majority of the previous literature on SETTLE focused on the clinical and pathological characteristics of SETTLE, with a few reports mentioning the imaging findings of SETTLE. Due to the lack of literature data, there are no established characteristic findings of SETTLE in all possible modalities, including ultrasound, CT, magnetic resonance imaging, and thyroid scans. Lee et al. [
10] reported that the patients' CT scans showed well-defined, lobulated solid masses with a significant mass effect. According to Ippolito et al. [
7], the tumor is normally described as circumscribed, partially circumscribed, or infiltrative in the case of larger tumors, and it is usually cold at thyroid scan with a heterogeneous pattern. The present case demonstrated a well-defined large heterogeneously enhanced mass on a CT scan and heterogeneous echogenicity on an ultrasound.
Surgery is the gold standard treatment for SETTLE. Similar to other thyroid cancers, preoperative ultrasound may be useful in evaluating abnormalities in the thyroid gland as well as the size, number, and localization of suspicious lymph nodes. Chemotherapy and radiotherapy could be another possible option for patients with advanced stage SETTLE to control the tumor growth, and for patients with infiltrative local disease, vascular invasion or metastasis. The best regimen, dose and duration of chemotherapeutic agents are yet to be determined. However, cisplatin, etoposide, and cyclofosfamide have been reported as effective in certain cases. Radiotherapy may be used as a neo-adjuvant therapy in cases of nonresectable tumors, painful masses, or bone metastases [
7].
SETTLE is a very rare tumor that should be considered in the differential diagnosis of spindle cell tumors in the thyroid gland. The imaging findings of SETTLE tumors are yet to be determined, however, as they are usually described as well-defined heterogeneously enhanced masses on CT scans and masses with heterogeneous echogenicity on ultrasound. Differential diagnosis of SETTLE could be included in cases of bulky thyroid mass extending to the mediastinum. As there is a possibility of late metastasis, close follow-up should be considered.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download