INTRODUCTION
Functional defecation disorder (FDD) is diagnostic terminology defined in the Rome III criteria [
1], and is consistent with functional constipation (FC) caused by functional outlet obstruction including dyssynergic defecation (DD) and inadequate defecatory propulsion (IDP). As a subtype of FC, FDD has been estimated to underlie the symptoms of straining, incomplete evacuation and residual sensation in as many as 50% of patients with FC [
23]. Distinguishing FDD from other subtypes of FC is important clinically, because FDD may be less likely to respond to traditional medical and dietary therapies and may be more likely to respond to biofeedback therapy [
456]. However, symptoms alone are not enough to discriminate between subtypes of FC, and diagnostic testing for FDD is needed to properly treat patients with FC.
According to the Rome III criteria [
1], objective findings of at least 2 of the following during repeated attempts to defecate are essential for the diagnosis of FDD; (1) impaired evacuation, based on balloon expulsion test (BET) or imaging, (2) inappropriate contraction of the pelvic floor muscles or less than 20% relaxation of basal resting sphincter pressure assessed with anorectal manometry (ARM), imaging, or electromyography (EMG), (3) inadequate propulsive forces assessed using ARM or imaging. Current guidelines from the American Gastrointestinal Association recommend ARM with or without BET as a basic test that should be done first to distinguish FDD in constipated patients after a therapeutic trial of fibers and/or over-the-counter laxatives have failed [
7]. Other physiologic tests including defecography, EMG and colonic transit study are performed according to the result of ARM.
In addition to conventional absolute pressures such as anal resting and squeeze pressures, some other parameters of ARM have recently been used to diagnose FDD. One of these parameters was the pattern classification of pressure changes in the rectum and anus during attempted defecation. Theoretically, normal pattern is characterized by adequate increase in rectal pressure accompanied by a simultaneous adequate reduction in anal pressure. Abnormal patterns include adequate increase in rectal pressure with paradoxical increase in anal pressure, inadequate increase in rectal pressure with paradoxical increase in anal pressure, adequate increase in rectal pressure with absent or incomplete reduction in anal pressure, and inadequate increase in rectal pressure with absent or incomplete reduction in anal pressure.
Quantification of pressure changes in the rectum and anus during attempted defecation was also attempted by the creation of the defecation index which is the calculated ratio between rectal pressure and anal residual pressure during attempted defecation. A defecation index less than 1.2 was suggested to correlate with FDD [
89]. Multiple studies, however, have demonstrated that such abnormal findings of ARM in constipated patients are also common occurrences among asymptomatic controls [
10111213], limiting the utility of these criteria in clinical practice.
In this study, a retrospective evaluation of all the parameters of ARM was performed to assess the clinical significance of ARM in diagnosing FDD. The specific aim was to evaluate the accuracy of not only conventional absolute pressures, but also the pattern classification and quantification of pressure changes in the rectum and anus during attempted defecation for use in discrimination between nonconstipated (NC) subjects and FC subjects, and between FC subjects with and without FDD.
METHODS
All female patients who visited the anorectal physiology unit at Konkuk University Hospital between March 2013 and October 2016 were considered for study enrollment. Electronic medical records were retrospectively reviewed. Those who could be grouped into the following categories were included; functionally constipated subjects (FC group) with FDD (+FDD subgroup), or without FDD (−FDD subgroup) and NC subjects (NC group). Subjects with a significant gastrointestinal disease, severe endocrine diseases, neurologic disease, pregnancy, fecal incontinence, or previous history of anal or abdominal surgery were excluded. FC was defined according to the Rome III criteria [
6]. FDD was defined as the occurrence of positive findings on both defecography and EMG. NC subjects were mainly those with hemorrhoids (grades I–II) or simple anal fistula, but without FC. This study was approved by the Institutional Review Board (IRB) at Konkuk University Hospital (approval number: KUH 1020080). Informed consent was exempted by the IRB.
ARM was performed with a standard water-perfusion system, comprising a water-perfused catheters with 8 channels attached to a hydraulic capillary infusion system (Medtronics, Minneapolis, MN, USA). The catheter was 4.5 mm in diameter with side-holes of 0.8 mm in diameter, which were aligned spirally at 7 mm intervals along the longitudinal axis. Examination was performed in the lateral decubitus position. After calibrating the system, the catheter was inserted into the anal canal until the outermost side-hole was placed at the anal verge.
While the catheter was in position, rectal and anal pressures were measured synchronously at squeeze and push (attempted defecation) with intervening resting periods. Rectal and anal channels were distinguished by pressure change during squeeze. Anal squeeze pressure (ASP) and anal resting pressure were expressed as peak and average values during each period. Anal push pressure (APP) was expressed as minimum value or the value at peak point of rectal push pressure (RPP). RPP was expressed as peak value.
ARM was interpreted not only with conventional absolute pressures, but also with pattern classification and quantification of pressure changes in the rectum and anus during attempted defecation. The patterns of pressure changes were classified into 6 types to include all possible patterns of occurrence (
Fig. 1).
Type 0: an adequate increase in rectal pressure (≥40 mmHg) accompanied by a simultaneous reduction in anal pressure (>20% baseline pressure)
Type 1: an adequate increase in rectal pressure (≥40 mmHg) accompanied by a paradoxical simultaneous increase in anal pressure
Type 2: an inadequate increase in rectal pressure (<40 mmHg) accompanied by a paradoxical simultaneous increase in anal pressure
Type 3: an adequate increase in rectal pressure (≥40 mmHg) accompanied by failure of reduction in anal pressure (≤20% baseline pressure)
Type 4: an inadequate increase in rectal pressure of (<40 mmHg) accompanied by failure of reduction in anal pressure (≤20% baseline pressure)
Type 5: an inadequate increase in rectal pressure (<40 mmHg) accompanied by a simultaneous reduction in anal pressure (>20% baseline pressure)
Among the pattern types, 0 was considered ‘normal’ and 1–5 were regarded as ‘abnormal’ responses as defined by previous studies [
89].
As a quantification parameter of the pressure changes during attempted defecation, the manometric defecation index (MDI) was used. The MDI is the ratio of rectal pressure to anal pressure during attempted defecation (rectal pressure/anal pressure). In addition to MDI, the rectoanal pressure gradient (RAG) was also calculated. This was defined by the difference between the pressures during attempted defecation (rectal pressure-anal pressure).
Defecography was performed with a fluoroscopic system. With the subject in the left lateral position, 50 mL of liquid barium was inserted into the rectum using a catheter syringe. The vaginal wall of the subject was coated with an appropriate amount of water-soluble contrast. After barium paste was inserted until the patient felt a constant desire to defecate, the patient was asked to sit down on a specially designed commode in their usual sitting position for defecation. Fluoroscopic dynamic imaging was obtained while the patient was trying to evacuate the rectum. The result was interpreted as positive when there was poor emptying of the rectum with poor opening of the anal canal and/or persistent posterior angulation of the rectum. However, poor emptying with structural changes such as rectocele or intussusception but without poor opening or persistent angulation were interpreted as negative [
14].
EMG was performed with subjects in the sitting position. A plug-type electrode was inserted into the anal canal and another surface-type electrode was attached to the abdominal wall. After the patient adjusted to the sensation of having a plug in the anal canal, EMG was recorded using a biofeedback system (HMT2000, HMT Inc., Seoul, Korea) at rest, squeeze, and push. EMG findings were considered positive when paradoxical contraction or nonrelaxation of electrical activity was present while the patient was attempting to push the plug out.
Statistical analysis was completed with SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) and dBSTAT ver. 5.0 (dBSTAT Inc., Seoul, Korea). Distributions in the patterns of pressure changes were compared between the groups, or between the subgroups with the chi-square test or Fisher exact test according to sample size. Continuous variables were expressed as mean ± standard deviation, and compared with the Student t-test or Mann-Whitney test according to the normality of distribution. The Shapiro-Wilk test was used to confirm the normality of data distribution. Diagnostic utility and optimal cutoff values of continuous variables were defined with receiver operating characteristic (ROC) curves. A P-value of <0.05 was considered statistically significant.
RESULTS
A total of 151 subjects fulfilled selection criteria. All were female. There were 76 subjects in the NC group and 75 in the FC group. Both groups were similar in age distribution (55.33 ± 16.45 years vs. 54.04 ± 16.91 years, P = 0.635). Among the FC group, 63 subjects were in the −FDD subgroup and 12 in the +FDD subgroup. Subjects in the −FDD subgroup were slightly older than those in the +FDD subgroup (55.14 ± 15.82 years vs. 48.25 ± 19.14 years, P = 0.185).
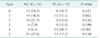
In the pattern classification of pressure changes in the rectum and anus during attempted defecation, Type 0, as the ‘normal’ response, was only slightly more prevalent in the NC group than in the FC group (19.7%
vs. 10.7%, P = 0.121). Among the FC group, type 0 was comparable in frequency between the −FDD and +FDD subgroups (11.1%
vs. 8.3%, P > 0.999). Type 4 was significantly more prevalent in the FC group than in the NC group (30.7%
vs. 5.3%, P < 0.001). Type 4 was the only ‘abnormal’ type that showed significantly different prevalence between the NC and FC groups. However, among the FC group, type 4 was more prevalent in the −FDD subgroup, rather than in the +FDD subgroup (33.3%
vs. 16.7%, P = 0.321). Other ‘abnormal’ types were comparable in prevalence between the groups, and between the subgroups. When all ‘abnormal’ types (types 1–5) were considered together as positive findings, the sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio for use of pattern classification in diagnosing FC among all subjects were 89.3%, 22.7%, 1.16, and 0.47, respectively. Those values of pattern classification in diagnosing FDD among the FC subjects were 91.7%, 11.1%, 1.03, and 0.75, respectively (
Tables 1,
2).
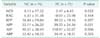
The quantification parameters of pressure changes during attempted defecation, MDI and RAG were markedly different between the NC and FC groups, but without statistical significance (8.13 ± 17.32
vs. 2.47 ± 6.45, P = 0.052) (6.33 ± 31.38
vs. −0.03 ± 23.98, P = 0.164). However, the parameters were significantly different between the −FDD and +FDD subgroups in the FC group (2.78 ± 7.00
vs. 0.80 ± 0.47, P = 0.022) (3.43 ± 22.06
vs. −18.91 ± 24.50, P = 0.003) (
Tables 3,
4). ROC curves of MDI and RAG had an area of 0.694 and 0.703, respectively, for discrimination between the −FDD and +FDD subgroups in the FC group. Optimal cutoff values were 1.0 and 0, respectively, with sensitivity 66.7% and specificity 61.9% in common (
Figs. 2,
3).
Among absolute pressure values, APP was significantly higher in the FC group than in the NC group (39.55 ± 24.36 vs. 32.11 ± 26.20, P = 0.031). It was also markedly higher in the +FDD subgroup than in the −FDD subgroup, but without significance (56.70 ± 36.16 vs. 36.29 ± 20.22, P = 0.052). Additionally, ASP was significantly higher in the FC group than in the NC group (90.51 ± 38.44 vs. 110.97 ± 52.07, P = 0.006). Other pressure values were comparable between the groups, and between the subgroups.
DISCUSSION
The results of this study are summarized as the following four points. First, the pattern classification of pressure changes in the rectum and anus during attempted defecation was not useful for diagnosing FDD. Type 0, the ‘normal’ pattern, was only slightly more prevalent in the −FDD subgroup than in the +FDD subgroup in the FC group. Even in the NC group, the prevalence of type 0 was low and not significantly different from the prevalence in the FC group. Even when all ‘abnormal’ types (types 1–5) were considered together as positive findings, the diagnostic accuracy of ‘abnormal’ types for discriminating +FDD subgroup among FC group was poor with very low specificity. Second, the quantification parameters of pressure changes in the rectum and anus during attempted defecation, MDI and RAG, were useful to diagnose FDD among FC patients. They were significantly different between the −FDD and +FDD subgroups. The optimal cutoff values for FDD in ROC curves analysis were 1.0 and 0, respectively. Third, APP was significantly higher in the FC group than in the NC group. It was also markedly higher in the +FDD subgroup than in the −FDD subgroup, although not statistically significant. These results may suggest that impaired defecation in patients with FDD was attributed mainly to increased resistance to evacuation, rather than weak propulsive force. Lastly, other conventional absolute pressures were not useful to diagnose FDD. They were mostly comparable not only between the −FDD and +FDD subgroups, but also between the NC and FC groups.
ARM is commonly used as a diagnostic adjunct in patients with constipation and incontinence. Although recent progress in technology has enabled high-resolution ARM, conventional water-perfusion ARM is still a commonly used physiologic test for anorectal functional disorders, allowing inexpensive screening with limited space and minimal laboratory staff [
15]. When ARM is used for chronic constipation, the most important take-away point is the identification of FDD. Indeed, patients with FDD should be identified early and referred for biofeedback therapy, which has proven benefit over laxatives in this patients group [
45615]. In the absence of a gold standard, various tests such as defecography and anal EMG in addition to ARM have been used for the diagnosis of FDD with variable correlations between the tests. Nevertheless, dyssynergic findings identified with ARM have been widely used to diagnose and classify FDD, because of its convenience and availability in clinical practice.
According to the Rome III criteria, ARM for the diagnosis of FDD should clarify whether there is inappropriate contraction of the pelvic floor or less than 20% relaxation of basal resting sphincter pressure with adequate propulsive forces during attempted defecation, or inadequate propulsive forces with or without inappropriate contraction of the pelvic floor or less than 20% relaxation of basal resting sphincter pressure during attempted defecation. While conventional ARM parameters including anal and rectal pressures are routinely used to investigate the above criteria, some other metrics have also been used recently to make the interpretation easier. One of these is the pattern classification of pressure changes in the rectum and anus during attempted defecation. Quantifying pressure changes by the creation of an additional parameter such as the MDI is another option.
Abnormal patterns of pressure changes in the rectum and anus were usually classified into 3 or 4 types. Normally, when a subject attempts to defecate, there is a rise in rectal pressure, which is synchronized with a relaxation of the external anal sphincter. The inability to perform this coordinated movement represents the main pathophysiologic abnormality in patients with FDD. This may either be due to impaired rectal contraction, paradoxical anal contraction or impaired anal relaxation or a combination of these mechanisms. Based on these features abnormal dyssynergic patterns of pressure changes were suggested to help diagnose FDD [
8916].
On the other hand, there is some controversy in their clinical application. It is not obvious how much rectal pressure should rise by push action for a normally adequate propulsive force. Although 40 mmHg is suggested as a minimum requirement for the adequacy, it does not take into account gender and age differences. And 3 or 4 types may not be enough to include all possible occurrences. Moreover, in addition to motor abnormalities, there could also be other features of FDD such as sensory dysfunction of the rectum that are not incorporated into the pattern analysis [
1718]. These controversial points may have undermined the diagnostic value of the pattern classification. Indeed, more than half or up to 87% of healthy subjects were reported to have a pattern that was considered abnormal [
1219].
In this study, the patterns of pressure changes were classified into 6 types to include all possible occurrences. According to the Rome III criteria, Type 0 should represent normal physiology. Types 1, 3 and 2, 4, 5 should occur in DD and IDP, respectively. However, type 0 was found in only 19.7% of the NC group, and was comparable to the FC group in this study. Type 4 was reported in one study as the only type that could differentiate constipated patients from normal controls [
12]. Although type 4 was also significantly more prevalent in the FC group than in the NC group in this study, its prevalence was predominant in the −FDD subgroup, rather than in +FDD subgroup.
As a quantification parameter, MDI was originally defined as the ratio of the intrarectal pressure to the anal residual pressure when a subject is attempting defecation. The anal residual pressure was defined as the difference between the baseline pressure and the lowest pressure within the anal canal [
89]. Intuitively, it is more important for diagnosing FDD to evaluate the manometric condition of the rectum and anus synchronously, not to evaluate them separately. MDI reflects synchronous pressures of the rectum and anus. MDI ≥ 1.2 was thought to be necessary for normal evacuation, while MDI < 1.2 describes difficult defecation [
89].
However, several observations suggested an imperfect correlation between MDI and the results of other physiologic studies [
10111213]. They also reported considerable overlap in MDI or RAG among NC subjects and constipated subjects with or without FDD. Some technical problems of traditional water-perfused catheters may partly explain these observations. Although the configuration of pressure sensors on these traditional systems is variable, no traditional catheter can simultaneously measure circumferential pressures throughout the anal canal and in the rectum [
10]. Besides, it is not easy to determine the representative value of anal pressure during synchronous measurement of rectal and anal pressures, because the pressure varies considerably along the length of the anal canal, depending on the location of pressure sensor. Attempting defecation may drive the recording catheter against the wall of the anal canal producing a ‘contact pressure’ that may result in higher anal pressure [
20]. Moreover, there could be a sampling error in addition to technical errors. Because there was not a gold standard for diagnosing FDD, participants in most previous studies were patients with symptomatic constipation or poorly confirmed FDD, rather than definitely confirmed FDD [
1216]. Subjects with constipation but without FDD would exhibit normal findings in ARM.
In this study, pressure measurement was done using a water-perfused catheter with 8 channels. The catheter had 8 side-holes which were aligned spirally at 7-mm intervals along the longitudinal axis. Rectal and anal channels were distinguished based on pressure change during squeeze. The channels that responded sensitively to squeeze were considered anal channels. Among these, representative anal channel was also determined by a typical form of pressure wave. This maneuver with spirally aligned channels is believed to reduce technical errors caused by incorrect determination of the representative anal channel.
FDD is usually defined as the occurrence of at least 2 positive findings among 3 or more physiologic tests, which include ARM with or without BET, defecography and EMG. However, FDD was defined in this study as the occurrence of positive findings on both defecography and EMG. This definition was as strict as possible, reducing sampling errors in collecting the +FDD subgroup, although such strictness also reduced sample size.
MDI did not exhibit differences between the NC and FC groups, but did exhibit significant differences between the −FDD and +FDD subgroups. The optimal diagnostic cutoff value for FDD in ROC curve analysis was 1.0 (sensitivity, 66.7%; specificity, 61.9%), rather than 1.2. RAG is another option for quantification of pressure changes during attempted defecation. RAG is similar to MDI with regard to mathematical and clinical significance. RAG 0 corresponds to MDI 1.0.
Obstructed defecation in FDD may arise from weak propulsive forces, increased resistance to evacuation, or both. However, it is unclear whether these disturbances reflect similar or separate pathophysiological mechanisms [
11]. In this study, RPP was comparable between the groups, but APP was significantly higher in the FC group than in the NC group and also markedly higher in the +FDD subgroup than in the −FDD subgroup, although this was not statistically significant. It could be inferred from these results that dyssynergia in FDD was largely due to paradoxical increase in anal pressure, and impaired defecation was attributed mainly to increased resistance to evacuation, rather than weak propulsive force. This means that DD would be more predominant than IDP in FDD.
This study has the following limitations. First, subjects in the NC group were not healthy asymptomatic persons, but NC patients with mild anal diseases. These anal diseases could distort the results of ARM, even though the severity was mild. However, history of constipation was cleared completely by routine check-up in anorectal physiology unit for functional bowel symptoms, especially infrequency, straining, and incompleteness. Second, small sample size in the +FDD subgroup could limit statistical power. The definition of FDD in this study was as strict as possible to reduce sampling errors in collecting the +FDD subgroup. This inevitably reduced the sample size. Further studies with an adequate +FDD subgroup size are needed to confirm the findings of this study.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download