Abstract
Purpose
The aim of this study was to evaluate the long-term outcome of additional 4-week chemotherapy with capecitabine during the resting periods following a 6-week neoadjuvant chemoradiotherapy (NCRT) regimen, in patients with locally advanced rectal cancer.
Methods
Radiotherapy was delivered to the whole pelvis at a total dose of 50.4 Gy for 6 weeks. Oral capecitabine was administered at a dose of 825 mg/m2 twice daily for 10 weeks. Surgery was performed 2–4 weeks following the completion of chemotherapy.
Results
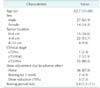
Between January 2010 and September 2011, 41 patients completed the scheduled neoadjuvant therapy and surgery. The pathologic complete response rate, 5-year overall survival, and 5-year disease-free survival rates were 22%, 85.4%, and 78.0%, respectively. The 5-year systemic recurrence and 5-year local recurrence rates were 22% and 0%, respectively.
Conclusion
Additional 4-week chemotherapy with capecitabine, during the resting periods following a 6-week NCRT regimen, has favorable long-term oncologic outcomes. Further randomized controlled trials are however necessary to evaluate if substantial improvement in local control is achieved with this additional chemotherapy modality for locally advanced rectal cancer.
Since the superiority of neoadjuvant concurrent chemoradiotherapy in terms of local control and safety has been demonstrated [1], it has become an essential component of standard therapeutic strategy for locally advanced rectal cancer. Although capecitabine and 5-fluorouracil (5-FU) are generally recommended as neoadjuvant concurrent chemotherapeutic agents [2], many researchers have been trying to find regimens that would improve oncologic outcomes by combination with other chemotherapeutic drugs [3] or biologic agents [45], or extension of duration of chemotherapy [6]. However, no regimen has yet been known to significantly improve survival. Many studies evaluating the efficacy of neoadjuvant therapy consider the pathologic complete response (pCR) rate as the primary endpoint, as it is well-known as a significant surrogate marker for oncologic prognosis in rectal cancer patients treated with chemoradiotherapy [7]. However, to evaluate oncologic outcomes of certain regimens, it is necessary to analyze survival data only after an acceptable follow-up period, because the pCR rate does not reflect the absolute survival rate. We performed the present study to evaluate the safety and efficacy of additional 4-week chemotherapy with capecitabine during the resting periods following 6-week NCRT in patients with locally advanced rectal cancer, and have reported its outcomes including pCR, tumor response, toxicity of chemoradiotherapy, and postoperative complications in 2013. This regimen has tolerable toxicity, is convenient for patients, and has a good pCR rate. After 5 years of follow-up, we analyzed the long-term oncologic outcomes in patients who completed the scheduled neoadjuvant therapy and surgery.
Consecutive patients with locally advanced rectal cancer within 12 cm from the anal verge, without distant metastasis, were eligible. The study was approved by the relevant Institutional Review Board of Chungnam National University Hospital (approval number: 2016-08-053). Baseline work-up for staging and assessment consisted of documenting history, physical and digital rectal examination, full colonoscopy or alternatively flexible sigmoidoscopy for obstructive lesions that endoscopy could not pass through, CEA, chest radiography, abdominopelvic CT, rectal MRI, and positron emission tomography. The inclusion criteria were as follows: (1) histologically verified adenocarcinoma, (2) cT3/4 or cN1/2 and M0 staging, (3) Eastern cooperative oncology group score 0–2, and (4) adequate function of major organs including the heart, liver, kidneys, or bone marrow. The exclusion criteria were as follows: (1) another malignant disease detected within the last 5 years, (2) severe underlying medical or psychiatric disorders, (3) previous radiotherapy to the pelvis, (4) refusal to undergo neoadjuvant therapy, and (5) pregnancy or lactation. Patients were enrolled after obtaining written informed consent.
Radiotherapy and chemotherapy were started simultaneously. Radiotherapy was delivered to the whole pelvic region by using a 3-field approach at a daily dose of 1.8 Gy in 25 fractions, followed by a boost of 5.4 Gy in 3 fractions, 5 days a week, for 6 weeks, with a total dose of 54 Gy. Oral capecitabine was administered at a dose of 825 mg/m2 twice a day for 6 weeks along with radiotherapy, and its administration continued at the same dose for another 4 weeks after completion of radiotherapy. In this period, postchemoradiotherapy work-up for evaluation of tumor response included CEA, flexible sigmoidoscopy, abdominopelvic CT, and rectal MRI. Radical surgery, including total mesorectal excision (TME), was performed 2–4 weeks after completion of chemotherapy by specialized, expert colorectal surgeons.
The primary endpoint was the pCR rate. Pathologic staging and evaluation of tumor response, according to the College of American Pathologist grading system, were performed by a specialized pathologist. The secondary endpoints were 5-year overall survival (OS) rate, 5-year disease-free survival (DFS) rate, 5-year systemic recurrence rate, and 5-year local recurrence rate.
The pCR rate has been reported to be 15%–30%. The authors previously reported a pCR rate of 20% for conventional NCRT, and therefore, it was decided as the primary endpoint. Given a desired statistical power of 80% and a significance level of 5%, the sample size was estimated to be 44 patients using G*Power 3 program. Descriptive statistics and survival analyses were performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA).
Between January 2010 and September 2011, 43 patients were enrolled. Two patients were excluded from the study because they discontinued chemotherapy 6 weeks after the onset of chemoradiotherapy due to Common Terminology Criteria for Adverse Events (CTCEA) grade 3 hand-foot syndrome (severe foot pain disabling walking 5 weeks after the onset of chemoradiotherapy, which improved after stop of capecitabine) and CTCEA grade 2 drug eruption (generalized rash with itching sensation of the trunk and extremities 5 weeks after the onset of chemoradiotherapy, which improved after stop of capecitabine and dermatologically conservative treatment), respectively. Ultimately, 41 patients who completed the scheduled neoadjuvant therapy for 10 weeks were analyzed. Clinical, surgical, and pathologic characteristics are presented in Tables 1 and 2. The pCR rate was 22% (n = 9). The mean follow-up period was 65.04 months (range, 17.91–79.54 months). The 5-year OS and DFS rates were 85.4 % and 78.0%, respectively. The 5-year systemic recurrence and local recurrence rates were 22% and 0%, respectively (Figs. 1, 2, 3). The sites of recurrence are presented in Table 3.
Radiotherapy is used to treat approximately 50% of cancers [8]. Ionizing radiation induces changes in the genetic makeup of various tumor cells and consequently disturbs basic cellular processes including cell signaling, proliferation, and damage response [9]. Cell damage occurs due to disruption of DNA integrity. Free radicals and reactive oxygen species break down the double-stranded DNA [10], and if there is failure in the repair of these damages, cell death occurs [9]. However, several factors including hypoxia, phases of cell cycle (most radiosensitive in the G2-M phase, less radiosensitive in the G1 phase, and least sensitive in the late S phase), tumor repopulation, or radioresistance are known to reduce radiotoxicity [11].
As radiotherapy has limitations, chemotherapeutic agents are combined concurrently as a radiosensitizer to augment the therapeutic effect of radiotherapy [12]. Chemoradiotherapy is proven to have superior oncologic outcomes to those of radiotherapy alone in most cancers, and in the field of rectal cancer treatment, it has been demonstrated to delay local recurrence significantly [1], and is even known to achieve a complete response. Both 5-FU and an oral 5-FU prodrug (capecitabine), which has been used most frequently and widely based on recommendations of various worldwide guidelines, are known to have equivalent efficacy [13]. As a radiosensitizer, 5-FU kills the S phase cells that are relatively radioresistant [14]. Capecitabine is metabolized into 5-FU in vivo, and it mimics the pharmacokinetics of a continuous 5-FU infusion. It has tolerable toxicity without requirement of intravenous administration [15]. Therefore, capecitabine has been considered an effective and patient-compliant drug for neoadjuvant therapy of rectal cancers.
To increase the pathologic response and improve outcomes including not only local recurrence but also OS and DFS, many investigators have been trying to develop a superior neoadjuvant chemotherapy regimen by combination with other drugs. Although the ACCORD 12, STAR-01, NSABP-R04, and PETACC-6 randomized phase III trials investigated the addition of oxaliplatin, no significant improvement was observed in the pCR rate [16171819], The German CAO/ARO/AIO-04 trial reported a significantly increased pCR rate and 3-year DFS on the addition of oxaliplatin to 5-FU neoadjuvant therapy in comparison to that of 5-FU-alone therapy (pCR: 17% vs. 13%, P = 0.038; 3-year DFS: 72.9 vs. 71.2, P = 0.03) [320]. However, the ACCORD 12, STAR-01, NSABP-R04 and German CAO/ARO/AIO-04 trials reported significantly increased grade 3–4 toxicities with oxaliplatin-added chemoradiotherapy compared to 5-FU-alone chemoradiotherapy [3161718]. A meta-analysis reported that, although oxaliplatin-added neoadjuvant therapy decreased DFS, it could not improve OS [21]. Another meta-analysis reported equal 5-year DFS and OS rates between the oxaliplatin group and 5-FU-alone group; the researchers insisted that the benefit of adding oxaliplatin was controversial and that the use of oxaliplatin could not be considered a stand-alone approach [22]. The oncologic benefit of the combination of oxaliplatin with conventional 5-FU chemoradiotherapy is still controversial owing to the significantly high rate of toxicity. In addition, many studies about the combination of biologic agents and NCRT have been reported. Although the addition of bevacizumab showed a favorable pCR rate, it is considered to significantly increase toxicity, including enteritis or perforation, and surgical complications, including delayed wound healing, fistula, or bleeding [23]. A combination of cetuximab has shown disappointing pCR [24].
Another effort to improve oncologic outcomes is to increase the interval to radical surgery. Many researchers have reported that an interval to TME longer than 6–8 weeks, the generally accepted resting period since the Lyon R90-01 trial [25], could improve pCR [26]. Macchia et al. [27] reported that the pCR rate increased as time to surgery increased (12.6% in the group that underwent TME within 6 weeks, 23% within 7–12 weeks, and 31.1% within 13 or more weeks, P < 0.001). As the strategy of lengthening interval to radical surgery has been adopted more commonly, organ-preserving procedures including local excision or even the “wait and see” approach have been attempted more often in good responders to neoadjuvant therapy [28]. However, for poor responders, there is a need for more effective neoadjuvant therapy during increased interval to surgery.
There are concerns about the therapeutic vacancy between NCRT and surgery, especially for poor responders. Several researches have tried consolidation chemotherapy for increased resting periods, to augment tumor downstaging and to improve oncologic outcomes including not only local control but also systemic control. The Timing of Rectal Cancer Response to Chemoradiation Consortium reported that the pCR rate increased as more cycles of mFOLFOX were performed during the resting period (pCR rate: 18%, 25%, 30%, and 38% for each group administered 0, 2, 4, and 6 cycles, respectively) [29]. They reported grade 3 toxicity in 26% of cases.
The pCR rate of present study and the pCR rate of our previous study that used for calculation of sample size were 22% and 20%. Both pCR rates cannot be compared directly and it is impossible to evaluate which therapeutic method is superior oncologically because the time of both studies is different, and there are also differences in the patient group and treatment strategy, and above all, the present study is designed as a single arm study. Nevertheless, both pCR rates are considered to be favorable comparing to the generally reported pCR, and the pCR rate of the present study could be considered to be not inferior to that of conventional NCRT.
In the present study, consolidation chemotherapy is a 4-week extension of capecitabine at the same dose of radiosensitizer. Therefore, it is hard to expect the equal effect of systemic chemotherapy. The 5-year OS, DFS, and systemic recurrence rates were 85.4%, 78.0%, and 22.0%, and they are considered to be equal compared to generally reported outcomes by other numerous studies. The 5-year of local recurrence rate was 0%, and in spite of the consideration of the small sample size of the present study, it is considered to be a positive result. However, the tumor response after radiotherapy continues during the resting period, which has been demonstrated by the fact that the time to surgery and pCR are proportional; the administration of capecitabine as a radiosensitizer may have the potential to increase the lasting effect of radiotherapy during the resting period, and to improve local control consequently. The pCR rate in the present study was favorable (22%), and there was no local recurrence for 5 years. As this regimen is a simple extension of an easily administrable oral drug, it has tolerable toxicity unlike the combination with oxaliplatin.
First, this was not a comparative study, and therefore, oncologic superiority cannot be confirmed. Second, the administered adjuvant chemotherapy regimens were heterogeneous because national insurance coverage for adjuvant therapy of rectal cancer was not established, and patient preference was reflected in selecting chemotherapeutic agent consequently. Third, when the present study was conducted, the widely implemented resting period was 6–8 weeks. However, lately, the optimal schedule is considered to more than 8 weeks. If this strategy of extended resting period is adopted, oncologic outcomes would improve with this consolidation therapy.
In conclusion, additional 4-week chemotherapy with capecitabine, during the resting periods following a 6-week NCRT, has favorable long-term oncologic outcomes. Further randomized controlled trials are, however, necessary to evaluate if substantial improvement in local control is achieved with this additional chemotherapy modality for locally advanced rectal cancer.
References
1. Bosset JF, Collette L, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, et al. Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med. 2006; 355:1114–1123.

2. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN Guidelines): Colon/rectal cancer. ver. 1. 2010 [Internet]. Fort Wathington (PA): National Comprehensive Cancer Network;c2017. cited 2017 Jul 19. Available from: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
3. Rodel C, Graeven U, Fietkau R, Hohenberger W, Hothorn T, Arnold D, et al. Oxaliplatin added to fluorouracil-based preoperative chemoradiotherapy and postoperative chemotherapy of locally advanced rectal cancer (the German CAO/ARO/AIO-04 study): final results of the multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2015; 16:979–989.
4. Gruenberger B, Tamandl D, Schueller J, Scheithauer W, Zielinski C, Herbst F, et al. Bevacizumab, capecitabine, and oxaliplatin as neoadjuvant therapy for patients with potentially curable metastatic colorectal cancer. J Clin Oncol. 2008; 26:1830–1835.

5. Eisterer W, Piringer G, DE Vries A, Ofner D, Greil R, Tschmelitsch J, et al. Neoadjuvant chemotherapy with capecitabine, oxaliplatin and bevacizumab followed by concomitant chemoradiation and surgical resection in locally advanced rectal cancer with high risk of recurrence - A Phase II Study. Anticancer Res. 2017; 37:2683–2691.
6. Habr-Gama A, Perez RO, Sao Juliao GP, Proscurshim I, Fernandez LM, Figueiredo MN, et al. Consolidation chemotherapy during neoadjuvant chemoradiation (CRT) for distal rectal cancer leads to sustained decrease in tumor metabolism when compared to standard CRT regimen. Radiat Oncol. 2016; 11:24.

7. Maas M, Nelemans PJ, Valentini V, Das P, Rodel C, Kuo LJ, et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data. Lancet Oncol. 2010; 11:835–844.

8. Garcia-Barros M, Paris F, Cordon-Cardo C, Lyden D, Rafii S, Haimovitz-Friedman A, et al. Tumor response to radiotherapy regulated by endothelial cell apoptosis. Science. 2003; 300:1155–1159.

9. Mueller AK, Lindner K, Hummel R, Haier J, Watson DI, Hussey DJ. MicroRNAs and their impact on radiotherapy for cancer. Radiat Res. 2016; 185:668–677.

10. Li L, Story M, Legerski RJ. Cellular responses to ionizing radiation damage. Int J Radiat Oncol Biol Phys. 2001; 49:1157–1162.

11. Pawlik TM, Keyomarsi K. Role of cell cycle in mediating sensitivity to radiotherapy. Int J Radiat Oncol Biol Phys. 2004; 59:928–942.

12. Lawrence TS, Blackstock AW, McGinn C. The mechanism of action of radiosensitization of conventional chemotherapeutic agents. Semin Radiat Oncol. 2003; 13:13–21.

13. Hofheinz RD, Wenz F, Post S, Matzdorff A, Laechelt S, Hartmann JT, et al. Chemoradiotherapy with capecitabine versus fluorouracil for locally advanced rectal cancer: a randomised, multicentre, non-inferiority, phase 3 trial. Lancet Oncol. 2012; 13:579–588.

14. Byfield JE. Useful interactions between 5-fluorouracil and radiation in man: 5-fluorouracil as a radiosensitizer. In : Hill BT, Bellamy AS, editors. Antitumor drugradiation interactions. Stuttgart (NY): CRC Press, Inc.;1990. p. 87–105.
15. Kim JS, Kim JS, Cho MJ, Song KS, Yoon WH. Preoperative chemoradiation using oral capecitabine in locally advanced rectal cancer. Int J Radiat Oncol Biol Phys. 2002; 54:403–408.

16. Gerard JP, Azria D, Gourgou-Bourgade S, Martel-Laffay I, Hennequin C, Etienne PL, et al. Comparison of two neoadjuvant chemoradiotherapy regimens for locally advanced rectal cancer: results of the phase III trial ACCORD 12/0405-Prodige 2. J Clin Oncol. 2010; 28:1638–1644.
17. Aschele C, Cionini L, Lonardi S, Pinto C, Cordio S, Rosati G, et al. Primary tumor response to preoperative chemoradiation with or without oxaliplatin in locally advanced rectal cancer: pathologic results of the STAR-01 randomized phase III trial. J Clin Oncol. 2011; 29:2773–2780.
18. O'Connell MJ, Colangelo LH, Beart RW, Petrelli NJ, Allegra CJ, Sharif S, et al. Capecitabine and oxaliplatin in the preoperative multimodality treatment of rectal cancer: surgical end points from National Surgical Adjuvant Breast and Bowel Project trial R-04. J Clin Oncol. 2014; 32:1927–1934.
19. Schmoll HJ, Haustermans K, Price TJ, Nordlinger B, Hofheinz R, Daisne JF, et al. Preoperative chemoradiotherapy and postoperative chemotherapy with capecitabine and oxaliplatin versus capecitabine alone in locally advanced rectal cancer: disease-free survival results at interim analysis. J Clin Oncol. 2014; 32:15 Suppl. 3501.
20. Rodel C, Liersch T, Becker H, Fietkau R, Hohenberger W, Hothorn T, et al. Preoperative chemoradiotherapy and postoperative chemotherapy with fluorouracil and oxaliplatin versus fluorouracil alone in locally advanced rectal cancer: initial results of the German CAO/ARO/AIO-04 randomised phase 3 trial. Lancet Oncol. 2012; 13:679–687.
21. De Felice F, Benevento I, Magnante AL, Musio D, Bulzonetti N, Caiazzo R, et al. Clinical benefit of adding oxaliplatin to standard neoadjuvant chemoradiotherapy in locally advanced rectal cancer: a meta-analysis : oxaliplatin in neoadjuvant treatment for rectal cancer. BMC Cancer. 2017; 17:325.

22. Fu XL, Fang Z, Shu LH, Tao GQ, Wang JQ, Rui ZL, et al. Meta-analysis of oxaliplatin-based versus fluorouracil-based neoadjuvant chemoradiotherapy and adjuvant chemotherapy for locally advanced rectal cancer. Oncotarget. 2017; 8:34340–34351.

23. Fornaro L, Caparello C, Vivaldi C, Rotella V, Musettini G, Falcone A, et al. Bevacizumab in the pre-operative treatment of locally advanced rectal cancer: a systematic review. World J Gastroenterol. 2014; 20:6081–6091.

24. Weiss C, Arnold D, Dellas K, Liersch T, Hipp M, Fietkau R, et al. Preoperative radiotherapy of advanced rectal cancer with capecitabine and oxaliplatin with or without cetuximab: A pooled analysis of three prospective phase I-II trials. Int J Radiat Oncol Biol Phys. 2010; 78:472–478.

25. Francois Y, Nemoz CJ, Baulieux J, Vignal J, Grandjean JP, Partensky C, et al. Influence of the interval between preoperative radiation therapy and surgery on down-staging and on the rate of sphincter-sparing surgery for rectal cancer: the Lyon R90-01 randomized trial. J Clin Oncol. 1999; 17:2396.

26. Sloothaak DA, Geijsen DE, van Leersum NJ, Punt CJ, Buskens CJ, Bemelman WA, et al. Optimal time interval between neoadjuvant chemoradiotherapy and surgery for rectal cancer. Br J Surg. 2013; 100:933–939.

27. Macchia G, Gambacorta MA, Masciocchi C, Chiloiro G, Mantello G, di Benedetto M, et al. Time to surgery and pathologic complete response after neoadjuvant chemoradiation in rectal cancer: a population study on 2094 patients. Clin Transl Radiat Oncol. 2017; 4:8–14.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download