Abstract
Purpose
There is no standardized single-incision laparoscopic cholecystectomy (SILC) technique in contrast to robot single-site cholecystectomy (RSSC). We tried to implement the array of instruments used in RSSC to SILC.
Methods
A series of 108 consecutive patients underwent SILC between September 2014 and July 2017 by 2 surgeons. The indication was benign disease of the gallbladder. The perioperative outcomes were reviewed. We used the 4-channel Glove port and conventional laparoscopic instruments.
Results
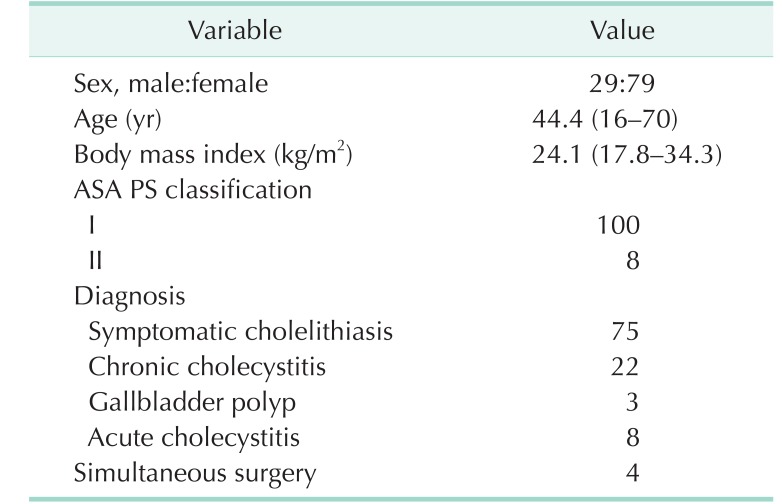
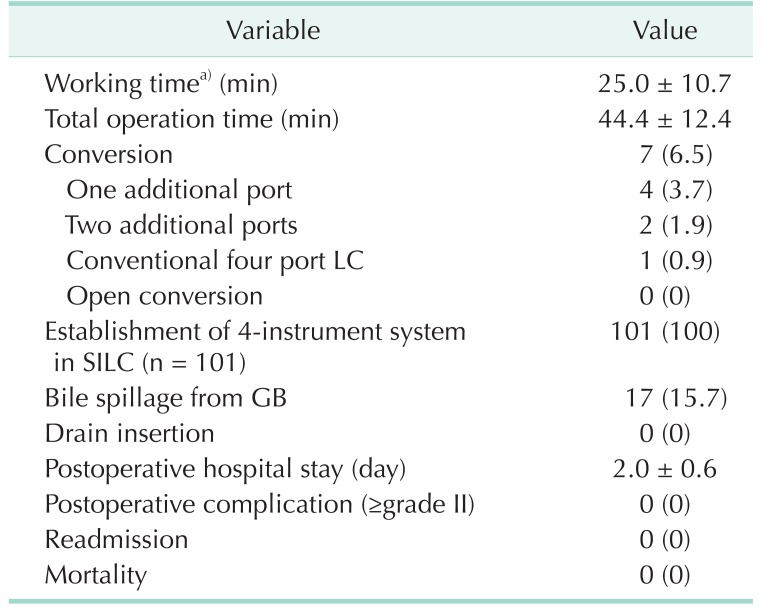
The study subjects consisted of 29 males and 79 females, and the mean age was 44.4 years (range, 16–70 years). Mean body mass index was 24.1 kg/m2. The mean working time was 25.0 ± 10.7 minutes and total operation time was 44.4 ± 12.4 minutes. There were 7 cases of conversion (additional 1 port in 4 patients, additional 2 ports in 2, and conventional 4 port technique in 1). Bile spillage from the gallbladder during the procedure occurred in 17 (15.7%). There were no postoperative complications. Postoperative hospital stay was 2.0 ± 0.6 days.
Minimization of surgical trauma is a major goal of minimally invasive surgery. Single-incision surgery is often attempted for the putative benefits that fewer surgical wounds will result in faster recovery by reducing surgical stress and pain and will lead to better cosmesis [1]. However, there is still a lack of evidence on the advantages of single-incision laparoscopic surgery [2]. A recent meta-analysis by Haueter et al. [3] found that single-incision laparoscopic cholecystectomy (SILC) has advantages in cosmesis, body image, and postoperative pain compared with conventional laparoscopic cholecystectomy, but the incidence of incisional hernia is high. Nonetheless, single-incision laparoscopic surgery has continued to evolve in response to surgeons' preferences and patient demands.
With single-incision laparoscopic surgery, surgeons face new challenges, such as collisions between instruments, poor ergonomics, and novel retraction techniques. Conventional laparoscopic cholecystectomy is a 4-port technique. Numerous methods and instruments have been introduced to implement the 4-port technique in SILC [456]. The biggest hurdles are to achieve triangulation between the instruments in the operative field and appropriate retraction of the gallbladder. Various single-port systems and laparoscopic instruments have been devised to overcome these challenges [7]. To date, however, there is no consensus on a standardized SILC technique, and different surgeons use different techniques, suggesting that there are inherent limitations of SILC itself. Recently, introduction of robotic single-site (Intuitive Surgical, Sunnyvale, CA, USA) cholecystectomy (RSSC) has improved ergonomics and triangulation among instruments, and provides a standardized procedure [8]. But the high price of the robotic surgical system remains prohibitive for many patients.
At our clinic, RSSC was introduced before SILC. During our early experience of RSSC [9], we tried to implement the array of instruments used in RSSC to SILC. Our SILC technique, which involves an almost identical configuration of instruments as in RSSC, has been successful. Here, we introduce our SILC technique and its outcomes.
A series of 108 consecutive patients underwent SILC between September 2014 and July 2017 by 2 surgeons at Bundang CHA Medical Center, CHA University School of Medicine, Seongnam, Korea. The indication of SILC was benign disease of the gallbladder, including symptomatic gallstones, benign gallbladder polyp with little possibility of malignancy, chronic cholecystitis including adenomyomatosis, and mild (grade I) acute cholecystitis [10]. Patients with suspicious malignancy, acute cholecystitis above moderate (grade II), and age over 70 years were fundamentally not indicated. Patients with a history of upper abdominal surgery were excluded. Patients requiring multiorgan surgery were not contraindicated.
Data on the demographics and perioperative outcomes of all patients were prospectively collected and analyzed retrospectively. We evaluated the successful establishment of the 4-instrument system, the conversion rate to an additional port or the conventional laparoscopic technique, and postoperative complications
Postoperative complications were graded on the basis of the Dindo-Clavien-Strasberg classification [1112].
This study was approved by the Institutional Review Board and ethics committees of CHA Bundang Medical Center of CHA University School of Medicine, Seongnam, Korea, and was conducted according to the principles of the Declaration of Helsinki (IRB No. 2018-05-023). A waiver of informed consent was requested, and approval was obtained.
We used the Glove port (Nelis, Bucheon, Korea) with four channels (Fig. 1). The channels were highly elastic, so devices of various sizes, ranging from 3 to 15 mm, could be applied. Installation methods were described in detail in the previous paper [913]. The blue channel for the laparoscopic camera was placed toward the gallbladder. The 2 channels for the working instruments and the camera channel were arranged in a triangle, and the remaining channel for gallbladder traction was located on the left side of the patient (Fig. 1).
In RSSC, the instrumental arrangement consists of a retraction grasper, a robotic camera, and 2 working instruments from the top in a single skin incision (Fig. 2) [9]. Such a configuration of the instruments was equally applied to our SILC technique.
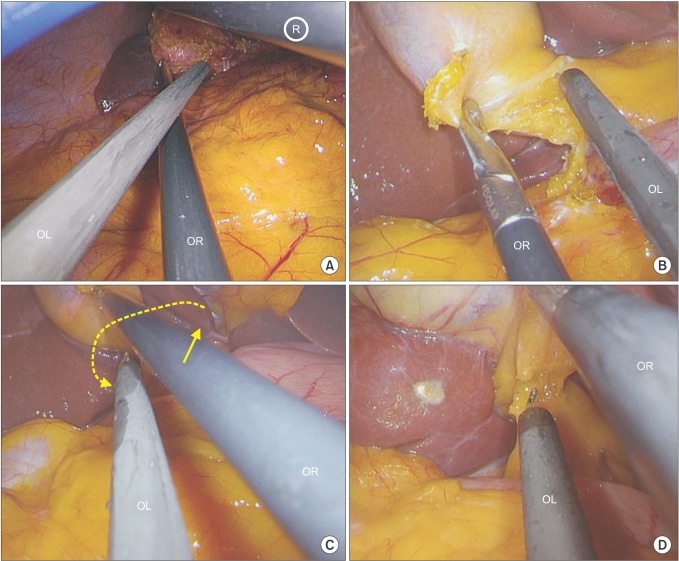
We used conventional linear laparoscopic instruments and a 10 mm 30° laparoscope. The laparoscopic camera entered through the blue channel, and the operative field was checked for possibility of SILC. The laparoscopic grasper (retraction grasper) was inserted for upward retraction of the gallbladder through the lateral channel (channel 1) and was fixed to the operative drape using a towel clip (Fig. 3). At this time, the laparoscope was moved to the bottom of the grasper (Fig. 4). The 2 working channels (channels 2 and 3) were located on the left and right sides of the laparoscope (Fig. 3). First, another laparoscopic grasper (working grasper) entered below the laparoscope through channel 2 and held the infundibulum of the gallbladder for lateral traction, widening Calot's triangle. Next, the laparoscopic hook coagulator entered between the working grasper and the laparoscope through channel 3. Thereby, the surgeon initiated lateral traction of the gallbladder using the working grasper with the right hand, and the anterior aspect of Calot's triangle was dissected using the hook coagulator with the left hand (Fig. 3B). Here, in order to dissect the posterior aspect of Calot's triangle, the 2 working instruments that were crossed could be exchanged up and down; it was not necessary for the surgeon to change hands (Fig. 3C, D). In this way, when the gallbladder was detached from the liver bed, it could be retracted freely from side to side by simply changing the positions of the working instruments. Once the gallbladder has been partially detached, the retraction grasper was removed, and the remaining gallbladder was dissected from the liver bed using only the working grasper. This occurred because, as the instruments (including the laparoscope) approached the gallbladder fundus, they collided with each other. This problem could be solved by removing the retraction grasper. After completing the cholecystectomy, the specimen was retrieved through the wound protector directly, removing the port cap without aid of a plastic bag.
A total of 108 patients underwent SILC (Table 1). The study subjects consisted of 29 males and 79 females, and the mean age was 44.4 years (range, 16–70 years). Mean body mass index (BMI) was 24.1 kg/m2 (range, 17.8–34.3 kg/m2), and 12 patients had high BMI over 30 kg/m2. All patients had an ASA score less than 2. Symptomatic cholelithiasis was present in 75 patients, chronic cholecystitis in 22, gallbladder polyp in 3, and grade I acute cholecystitis in 8. Four patients underwent simultaneous surgery, including 1 appendectomy, 2 ovarian cystectomies, and 1 inguinal hernioplasty.
The mean working time was 25.0 ± 10.7 minutes and total operation time was 44.4 ± 12.4 minutes (Table 2). There were 7 cases of conversion. Only 1 patient was converted to conventional 4-port laparoscopic cholecystectomy. Two ports of 2 mm and 5 mm were added in each of 2 patients. The remaining 4 patients had one 5-mm port added. All conversion cases were the result of severe inflammation, adhesion, and difficult exposure of Calot's triangle. Four-instrument system was successfully established in all patients who completed SILC without conversion. Bile spillage from the gallbladder during the procedure occurred in 17 patients (15.7%). There was no drain tube insertion. There was no injury of intra-abdominal organs during the procedure. Mean postoperative hospital stay was 2.0 ± 0.6 days. There were no postoperative complications, readmission or mortality.
Although SILC has grown in popularity, it is not yet associated with a standardized technique. Rather, most surgeons use their own procedures, with different instruments and port systems [451415161718]. Without a standard technique, it is difficult to select the best method when first trying SILC. Many studies on SILC have described the different instruments, ports, and traction methods, but there has been little explanation of the alignment of the instruments within the narrow single-incision; therefore, there is little description of the movement of the instruments. When we used SILC for the first time, we found it very frustrating to try to arrange the instruments in such a limited space. In contrast to SILC, robotic single-site cholecystectomy provides relatively standardized technique, which allows surgeons easy access during single-incision cholecystectomy with short learning curve [1920]. As we performed RSSC, we were able to experience and understand the proper configuration and dynamics of the instruments in the single-port system. We then applied this instrument array from the RSSC system to the SILC system to assess its feasibility.
Shortly after single-incision laparoscopic surgery was introduced, some doctors developed and used a home-made glove port. This home-made glove port was commercialized by Dr. Woo Jung Lee, Yonsei University, Seoul, Korea, under the name Glove port (Nelis). Although there are now many single-port systems, the Glove port is light and can accommodate various laparoscopic instruments ranging in size from 5 to 15 mm. Above all, the Glove port allows freedom to arrange instruments within the port system. The Glove port also provides more space for movement of the instruments compared to other port systems. The Glove port can be adopted for use in RSSC [921]. We have used the Glove port for the docking process in RSSC. In RSSC, from the top of the incision, an assistant laparoscopic grasper for upward retraction of the gallbladder is inserted, and the robotic camera is introduced underneath to push the laparoscopic grasper up. Then, 1 of the 2 robotic instruments lies across the other at the bottom of the incision (Fig. 2) [92223]. In the SILC system, the array of the instruments is identical to that of RSSC. From the top, the retraction grasper, camera, and 2 working instruments are arranged (Fig. 4A).
The biggest difference is that, unlike in SILC, RSSC has improved ergonomics by left-right hand coordination by electronic reverse recognition. In contrast, in most SILC systems, including our technique, the main instruments intersect each other at a fulcrum of the umbilicus for proper triangulation. Thus, the surgeon has to perform the main task with the left hand. Some surgeons operate at the right side of the patient or work by crossing one hand over the other in order to perform the primary task with the right hand [24]. However, with the exception of acute cholecystitis of grade II or more, most tasks in cholecystectomy are relatively simple, and surgeons can rapidly adapt even with the left hand. Previous reports on SILC have found an average working time of 15 to 20 minutes and a learning curve of 20 to 30 patients [62526]. In our study, the operation time showed similar results, with an average working time of 25.0 minutes.
Another disadvantage of SILC is difficult exposure of the posterior aspect of Calot's triangle [5]. With our technique, we used conventional laparoscopic instruments and simply changed the top and bottom of the 2 crossed instruments. This made it possible to safely expose and dissect the posterior aspect of Calot's triangle (Fig. 4). To prevent critical complications such as biliary damage, surgeons must accurately examine the major structures by exposing the critical view forward and backward according to the tenets of the SAGES Safe Cholecystectomy Taskforce [27]. Other studies have reported postoperative complication rates of 4% to 7% [2829], with bile leakages reported to occur in around 1% of cases [1]. Fortunately, we did not experience any complications during our study series. However, there were seven cases of conversion to an additional port or multiport laparoscopic cholecystectomy without open conversion because of the difficulty of exposure of the critical view. These cases were most common when Calot's triangle was completely obscured by the protruding lateral segment represented by the ‘beaver-tail liver’ [22], and safe operation was impossible. This suggested that the risk factor of conversion was the exposure issue rather than the technical issue.
Although the recent introduction of RSSC has allowed surgeons to easily perform single-incision cholecystectomy [19], the high cost makes the procedure inaccessible for many patients. The alignment of the instruments in RSSC is optimal, enabling free movement between the devices. This arrangement was introduced into our SILC system, so that an equally effective and safe operation was possible in well-selected patients.
References
1. Evers L, Bouvy N, Branje D, Peeters A. Single-incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy: a systematic review and meta-analysis. Surg Endosc. 2017; 31:3437–3448. PMID: 28039641.

2. Sajid MS, Ladwa N, Kalra L, Hutson KK, Singh KK, Sayegh M. Single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy: meta-analysis and systematic review of randomized controlled trials. World J Surg. 2012; 36:2644–2653. PMID: 22855214.

3. Haueter R, Schutz T, Raptis DA, Clavien PA, Zuber M. Meta-analysis of single-port versus conventional laparoscopic cholecystectomy comparing body image and cosmesis. Br J Surg. 2017; 104:1141–1159. PMID: 28569406.

4. Bucher P, Pugin F, Buchs N, Ostermann S, Charara F, Morel P. Single port access laparoscopic cholecystectomy (with video). World J Surg. 2009; 33:1015–1019. PMID: 19116734.

5. Choi SH, Hwang HK, Kang CM, Lee WJ. Single-fulcrum laparoscopic cholecystectomy: a single-incision and multi-port technique. ANZ J Surg. 2012; 82:529–534. PMID: 22776541.

6. Duron VP, Nicastri GR, Gill PS. Novel technique for a single-incision laparoscopic surgery (SILS) approach to cholecystectomy: single-institution case series. Surg Endosc. 2011; 25:1666–1671. PMID: 21057963.

7. Wakasugi M, Tei M, Omori T, Anno K, Mikami T, Tsukada R, et al. Single-incision laparoscopic surgery as a teaching procedure: a single-center experience of more than 2100 procedures. Surg Today. 2016; 46:1318–1324. PMID: 26922213.

8. Vyas D, Weiner C, Vyas AK. Current status of single-site robotic cholecystectomy, its feasibility, economic and overall impact. Am J Robot Surg. 2014; 1:1–64.

9. Ko JW, Lee JW, Kwon SW, Choi SH. Advantages of the glove port docking technique in robotic single-site cholecystectomy: comparison with the conventional silicone port. J Robot Surg. 2017; 9. 21. DOI: 10.1007/s11701-017-0754-5. [Epub].

10. Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, et al. TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2013; 20:35–46. PMID: 23340953.

11. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.
12. Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg. 2009; 250:177–186. PMID: 19638919.

13. Choi SH, Hwang HK, Kang CM, Lee WJ. Transumbilical single port laparoscopic adrenalectomy: a technical report on right and left adrenalectomy using the glove port. Yonsei Med J. 2012; 53:442–445. PMID: 22318837.

14. Abe N, Takeuchi H, Ohki A, Aoki H, Masaki T, Mori T, et al. Single-incision multiport laparoendoscopic surgery using a newly developed short-type flexible endoscope: a combined procedure of flexible endoscopic and laparoscopic surgery. J Hepatobiliary Pancreat Sci. 2012; 19:426–430. PMID: 21927879.

15. Allemann P, Schafer M, Demartines N. Critical appraisal of single port access cholecystectomy. Br J Surg. 2010; 97:1476–1480. PMID: 20641051.

16. Bhandarkar D, Mittal G, Shah R, Katara A, Udwadia TE. Single-incision laparoscopic cholecystectomy: How I do it? J Minim Access Surg. 2011; 7:17–23. PMID: 21197237.

17. Kuon Lee S, You YK, Park JH, Kim HJ, Lee KK, Kim DG. Single-port transumbilical laparoscopic cholecystectomy: a preliminary study in 37 patients with gallbladder disease. J Laparoendosc Adv Surg Tech A. 2009; 19:495–499. PMID: 19630589.

18. Ryu YB, Lee JW, Park YH, Lim MS, Cho JW, Jeon JY. One-year experience with single incision laparoscopic cholecystectomy in a single center: without the use of inverse triangulation. Ann Surg Treat Res. 2016; 90:72–78. PMID: 26878014.

19. Angus AA, Sahi SL, McIntosh BB. Learning curve and early clinical outcomes for a robotic surgery novice performing robotic single site cholecystectomy. Int J Med Robot. 2014; 10:203–207. PMID: 24030910.

20. Buzad FA, Corne LM, Brown TC, Fagin RS, Hebert AE, Kaczmarek CA, et al. Single-site robotic cholecystectomy: efficiency and cost analysis. Int J Med Robot. 2013; 9:365–370. PMID: 23640914.

21. Lee H, Lee DH, Kim H, Han Y, Kim SW, Jang JY. Single-incision robotic cholecystectomy: a special emphasis on utilization of transparent glove ports to overcome limitations of single-site port. Int J Med Robot. 2017; 13.

22. Konstantinidis KM, Hirides P, Hirides S, Chrysocheris P, Georgiou M. Cholecystectomy using a novel Single-Site(®) robotic platform: early experience from 45 consecutive cases. Surg Endosc. 2012; 26:2687–2694. PMID: 22476831.

23. Kiriyama S, Takada T, Hwang TL, Akazawa K, Miura F, Gomi H, et al. Clinical application and verification of the TG13 diagnostic and severity grading criteria for acute cholangitis: an international multicenter observational study. J Hepatobiliary Pancreat Sci. 2017; 24:329–337. PMID: 28419764.

24. Romanelli JR, Earle DB. Single-port laparoscopic surgery: an overview. Surg Endosc. 2009; 23:1419–1427. PMID: 19347400.

25. Erbella J Jr, Bunch GM. Single-incision laparoscopic cholecystectomy: the first 100 outpatients. Surg Endosc. 2010; 24:1958–1961. PMID: 20112110.

26. Rivas H, Varela E, Scott D. Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc. 2010; 24:1403–1412. PMID: 20035355.

27. Pucher PH, Brunt LM, Fanelli RD, Asbun HJ, Aggarwal R. SAGES expert Delphi consensus: critical factors for safe surgical practice in laparoscopic cholecystectomy. Surg Endosc. 2015; 29:3074–3085. PMID: 25669635.

28. Hall TC, Dennison AR, Bilku DK, Metcalfe MS, Garcea G. Single-incision laparoscopic cholecystectomy: a systematic review. Arch Surg. 2012; 147:657–666. PMID: 22802063.
29. Sato N, Shibao K, Mori Y, Higure A, Yamaguchi K. Postoperative complications following single-incision laparoscopic cholecystectomy: a retrospective analysis in 360 consecutive patients. Surg Endosc. 2015; 29:708–713. PMID: 25052126.

Fig. 1
Setting of the Glove port. The blue channel for the laparoscopic camera was placed toward the gallbladder (arrow). The 2 channels for the working instruments and the camera channel were arranged in a triangle, and the remaining channel for gallbladder traction was located on the left side of the patient.
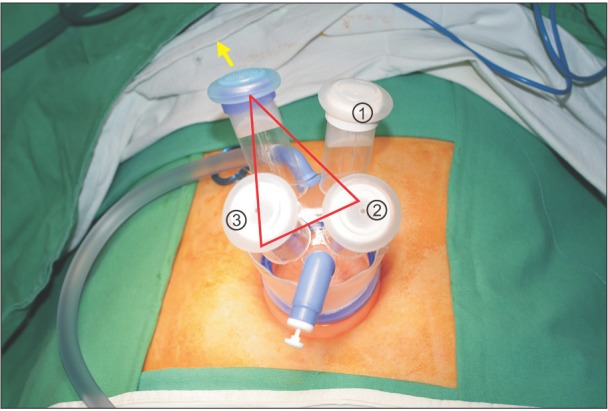
Fig. 2
Alignment of the instruments in robot single-site cholecystectomy. The instrumental arrangement consists of a retraction grasper, a robotic camera, and 2 working instruments from the top. The left lower figure shows the instrument sequence within skin incision. R, assistant retractor; C, camera; w1 and 2, working instruments.
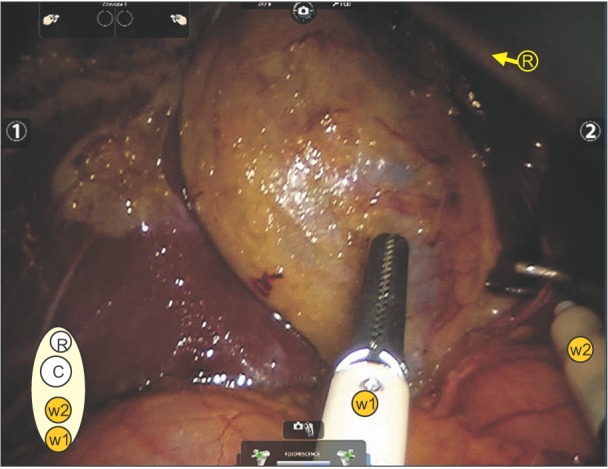
Fig. 3
External view of alignment of the instruments. (A) The laparoscopic grasper was inserted for upward retraction of the gallbladder through the lateral channel (channel ①) and was fixed to the operative drape using a towel clip (arrow). (B) The two working channels (channels ② and ③) were located on the left and right sides of the laparoscope. The traction of the gallbladder was made with the right hand of the operator, and the main work was performed with the left hand. ⓐ, assistant's hand; OR, operator's right hand; OL, operator's left hand.
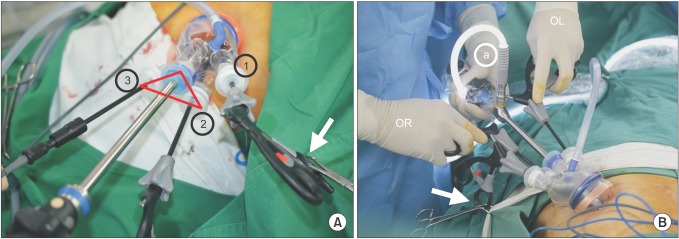
Fig. 4
Internal view of alignment of the intruments. (A) From top to bottom, retraction grasper, laparoscopic camera, coagulator, and working grasper. The laparoscopic camera was introduced first. Laparoscopic retraction grasper (®) was inserted for upward retraction of the gallbladder. At this time, the laparoscope was moved to the bottom of the grasper. Another laparoscopic working grasper entered below the laparoscope and the laparoscopic hook coagulator entered between the working grasper and the laparoscope. (B) Full exposure of the anterior Calot's triangle. (C) In order to dissect the posterior aspect of Calot's triangle, the 2 working instruments that were crossed could be exchanged up and down (arrows: direction of movement). (D) Full exposure of the posterior Calot's triagle. OR, operator's right hand (working grasper); OL, operator's left hand (laparoscopic coagulator).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download