Abstract
Three dogs were evaluated for severe hyperproteinemia and hyperglobulinemia secondary to Leishmania infantum. Double filtration plasmapheresis (DFPP) was performed in two dogs at days 1, 2, and 6 after presentation. The third dog received DFPP at days 1 and 3 after presentation and eleven hemodialysis treatments. Significant reduction in serum total protein (p < 0.0001), alpha-1 (p = 0.023), alpha-2 (p = 0.018), gamma globulins (p = 0.0105), and a significant increase in albumin/globulin ratio (p = 0.0018) were found. DFPP may be a promising therapeutic technique for rapid resolution of signs of hyperproteinemia in dogs affected by L. infantum.
Double filtration plasmapheresis (DFPP) has been used in human medicine for several pathological conditions, such as metabolic (hypercholesterolemia, hyperproteinemia), neurologic (myasthenia gravis, polyneuropathy), hematologic (thrombotic thrombocytopenia purpura), dermatological (pemphigus), rheumatologic (systemic lupus erythematosus), and renal diseases (acute glomerulonephritis) [6]. In veterinary medicine, the use of plasmapheresis (therapeutic plasma exchange or double filtration) has been reported for use in systemic lupus erythematosus [7], myasthenia gravis [1], immune-mediated hemolytic anemia [39], and hyperviscosity syndrome (HVS) [268]. Canine leishmaniasis is a disease, caused by Leishmania infantum, that is often associated with glomerulonephritis due to immune complex deposition [413]. Clinical manifestations of the disease may include anemia, hypo-albuminemia, hyperglobulinemia, azotemia, and proteinuria [13]. Recently, HVS has been documented in dogs affected by leishmaniosis [10].
The present paper reports the first clinical application of DFPP to reduce hyperproteinemia and hyperglobulinemia in three dogs affected by L. infantum.
A 2-year-old, intact male, 43 kg, Bernese mountain dog, presented to the Veterinary Teaching Hospital of University of Pisa with acute epistaxis. The dog had been diagnosed with visceral leishmaniasis (serum IFAT 1:2860) one week prior to presentation. The dog was severely depressed, with pale pink mucous membranes, hypotensive (100/65/70 mmHg), and tachycardic (150 bpm). Blood tests showed regenerative anemia, thrombocytopenia, mild azotemia, and severe hyperproteinemia with hyperglobulinemia (Table 1). Serum protein electrophoresis revealed a significant spike in gamma globulins. The dog had been previously treated with meglumine antimoniate (100 mg/kg subcutaneous [SC] every 24 h) and allopurinol (10 mg/kg by oral administration [PO] every 12 h) for one month. The patient received three DFPP treatments at days 1, 2, and 6 after presentation. Total plasma volume was estimated to be approximately 2,253 mL. Blood flow and plasma flow were set at 130 mL/min and 10 to 20 mL/min respectively, and treatment time was set at 2 h. The estimated macromolecule reduction ratio (MRR) was 70%. We treated 2,600 mL of plasma during the first treatment and 2,900 mL during the other two treatments.
A heparin bolus of 20 IU/kg (IU, international unit) was administered via an arterial port 5 min before starting the procedure, after which, heparin was administered as an intravenous continuous rate infusion at 50 IU/kg/h. Activated clotted time (ACT) was measured every 30 min and anticoagulation was monitored and adjusted accordingly. No complications occurred during the treatments. After the first treatment, an MRR of 44.5% was obtained; after the second and third treatments MRRs of 59% and 40.1%, respectively, were obtained. Complete resolution of the clinical signs was obtained after completion of the first treatment. At discharge from the hospital (day 7) the dog's condition was brilliant and showed only minimal rebound of total protein (7.8 mg/dL).
A 3-year-old, spayed female, 17 kg, mixed breed dog, presented to the ANUBI Companion Animal Hospital, Moncalieri (Italy) with a diagnosis of visceral leishmaniasis (IFAT 1:3200). Biochemistry panel showed hyperproteinemia, with hyperglobulinemia and an UP/UC of 0.4 (Table 1). The dog had received three previous treatments with miltefosine (2 mg/kg PO every 12 h for 28 days) over the past year. One month prior to presentation the dog was started on meglumine antimoniate (100 mg/kg SC every 24 h), allopurinol (15 mg/kg PO every 12 h), benazepril (0.5 mg/kg PO every 24 h), and a renal diet. The dog showed lameness and diffuse articular pain and was on tramadol at 2 mg/kg PO every 8 h.
The patient received a total of three DFPP at day 1, 2 and 6 after presentation. Total plasma volume of the dog was estimated to be 870 mL. Blood and plasma flow were set at 60 mL/min and at 10 to 15 mL/min, respectively. Treatment time was set at 2 h. For each treatment, 1,700 mL of plasma were processed. A heparin bolus of 50 IU/kg was administered through the arterial port 30 min before starting the procedure, after which heparin was administered as an intravenous continuous rate infusion at 50 IU/kg/h. ACT was maintained between 200 and 250 sec. No complications occurred during the treatments. After the first treatment, an MRR of 60.3% was obtained; after the second and third treatments MRRs of 78.5% and 72.9%, respectively, were obtained. Lameness and articular pain resolved completely within one week after the end of the third treatment.
A 7-year-old, intact male, 35 kg, Labrador retriever, with visceral leishmaniasis (IFAT 1:1600), presented to the ANUBI Companion Animal Hospital for oliguric, acute kidney injury (AKI) IRIS grade 5. The AKI developed after completion of a one-month treatment with meglumine antimoniate (100 mg/kg SC every 24 h). The dog was extremely lethargic with lymphadenopathy, abdominal effusion, and diffuse peripheral edema. Blood testing showed non-regenerative anemia, severe azotemia, and hype-proteinemia with hypoalbuminemia (Table 1). As renal function support was needed, DFPP was coupled with hemodialysis. The patient received two DFPP (on days 1 and 3 after presentation) and twelve intermittent hemodialysis (IHD) treatments. The total plasma volume of the dog was estimated to be 2,128 mL. Blood flow and plasma flow were set at 100 mL/min and at 25 mL/min, respectively. Treatment time was set at 120 min, in order to treat 3,000 mL of plasma. MRRs of 32.8% and 60.5% were obtained during the first and the second treatment, respectively. During the first dialysis, blood flow and dialysate flow were set at 50 mL/min and 500 mL/min, respectively. During the following treatments (11 IHD) blood flow was set between 100 and 200 mL/min and dialysate flow at 500 mL/min. As the renal disease progressed, owners elected to euthanize the dog.
Prior to the first DFPP treatment, each of the aforementioned three dogs were anesthetized for placement of a dual lumen temporary catheter (Hemo-Cath 13.5F, 28 cm; MedComp, USA) in the external right jugular vein. For all dogs, a Diapact CRRT machine (B Braun Avitum, Germany) was used in plasmapheresis modality (Fig. 1). A 0.2 m2 polyethylene plasma separator (Plasmaflo OP-02; Asahi Kasei Kuraray Medical, Japan) with a maximum pore size of 0.3 µm was used for separating plasma, while a 2 m2 ethylene vinyl alcohol copolymer plasma filter (Cascadeflo EC-30W; Asahi Kasei Kuraray Medical) with 110 mL of priming volume was used for filtrating plasma. The total volume of the extracorporeal circuit was 160 mL. Pre-treatment blood samples were collected 10 min before starting the procedure. Post-treatment blood samples were collected 15 sec after the end of the procedure, at a blood flow of 50 mL/min. No substitution solution was used after DFPP, as purified plasma was infused back to the patients at the end of each DFPP session.
For the IHD sessions, an AK200US (Gambro, Sweden) dialysis machine was used with pediatric lines (100 mL) and a Fresenius F4HPS dialyzer (51 mL; Fresenius Medical Care, Germany).
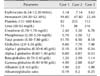
In the three dogs of this study, pre- and post-treatment concentrations of serum total protein, albumin, globulins, alpha-1, alpha-2, beta and gamma globulins, and albumin/globulin ratio (A/G ratio) were statistically evaluated by applying paired t-tests (with significance at p < 0.05) in GraphPad Prism software (GraphPad, USA), and the results are summarized in Table 2.
Plasmapheresis can be performed by using either centrifugal or membrane filtration techniques. In humans, centrifugal plasmapheresis is the primary modality used in North America to separate plasma from other blood components, while membrane filtration for plasma separation is more common in Europe and Japan [615]. The term DFPP refers to the apheresis technique, which uses a membrane plasma separator to separate plasma from blood cells. Plasma is then forced through a second filter (plasma fractionator; PF) in order to remove target solutes. Target molecules are trapped in the PF, on the basis of their molecular size and weight, while depurated plasma is returned to the patient [1114]. In human medicine, plasmapheresis has been used in the treatment of hypercholesterolemia, cryoglobulinemia, Waldenstrom's macroglobulinemia [1112], other immune-mediated diseases, and HVS [14]. In recent years, plasmapheresis has been used also in veterinary medicine to treat HVS [6] and immune-mediated hemolytic anemia [3].
The three patients reported herein showed significant reductions in the post-treatment levels of serum total protein (p < 0.0001) (Table 2). In the first case, the reduction was associated with complete remission of clinical signs of hyperproteinemia, and occurred immediately after the first treatment, whereas, in the second and third dogs, complete resolution of hyperproteinemia occurred after completion of third and second treatment, respectively. These results appear to support our previous observations in a dog affected by multiple myeloma and treated with DFPP, in which resolution of clinical signs of HVS occurred quite rapidly [6]. Significant reductions in post-treatment serum globulins (p < 0.0001), alpha-1 globulins (p = 0.023), alpha-2 globulins (p = 0.018) and gamma globulins (p = 0.0105) were also observed. These results may indicate a potential efficacy of DFPP in reducing inflammatory compounds. The effective reduction in serum protein was based on the calculation of MRR. Typically, the largest MRR occurs with removal of the first volume of plasma and becomes progressively less effective as subsequent plasma volumes are processed [5]. For this reason, we opted to process no more than two plasma volumes for each DFPP treatment. The intravascular rebound of macromolecules is driven initially by the diffusion of solutes from the extravascular to the intravascular space and by endogenous production. Immunoglobin G (IgG) has a long half-life (approximately 21 days), a molecular weight (MW) of 180,000 Da, and an approximate 50% intravascular distribution [5]. The plasma fractionator used in this study (Cascadeflo EC-30W) is generally considered the first-choice fractionator for the treatment of immune-diseases in humans; its sieving coefficient (about 0.4) is ideal for reduction of IgG (75% removal, MW 150,000 Da) with only mild loss of albumin (40%). Although in our study, post-treatment concentrations of serum albumin were significantly reduced (Table 2), no clinical signs of hypoalbuminemia were detected. Therefore, there was no need for exogenous plasma or albumin supplementation after the procedure.
This study documented the first clinical use of DFPP in the treatment of hyperproteinemia and hyperglobulinemia due to Leishmania infection in three dogs. DFPP seemed to be a safe, innovative, and promising technique that may contribute to quickly correcting hyperproteinemia and hyperglobulinemia in dogs affected by L. infantum. Further investigations to test the efficacy of different plasma fractionators and to determine the minimum number of treatments required should be encouraged.
Figures and Tables
Fig. 1
A Diapact CRRT machine (B Braun Avitum) continuous renal replacement therapy machine was used as the plasmapheresis modality.

Table 1
Complete blood count and serum biochemistry results from the three case dogs at the time of hospital admission
Notes
References
1. Bartges JW, Klausner JS, Bostwick EF, Hakala JE, Lennon VA. Clinical remission following plasmapheresis and corticosteroid treatment in a dog with acquired myasthenia gravis. J Am Vet Med Assoc. 1990; 196:1276–1278.
2. Boyle TE, Holowaychuk MK, Adams AK, Marks SL. Treatment of three cats with hyperviscosity syndrome and congestive heart failure using plasmapheresis. J Am Anim Hosp Assoc. 2011; 47:50–55.

3. Crump KL, Seshadri R. Use of therapeutic plasmapheresis in a case of canine immune-mediated hemolytic anemia. J Vet Emerg Crit Care (San Antonio). 2009; 19:375–380.

4. García-Martínez JD, Martinez-Subiela S, Tvarijonaviciute A, Caldin M, Ceron JJ. Urinary ferritin and cystatin C concentrations at different stages of kidney disease in leishmaniotic dogs. Res Vet Sci. 2015; 99:204–207.

5. Ismail N, Kiprov DD, Hakim RM. Plasmapheresis. In : Daugirdas JT, Blake PG, Ing TS, editors. Handbook of Dialysis. 4th ed. Philadelphia: Lippincott Williams & Wilkins;2007. p. 276–299.
6. Lippi I, Perondi F, Ross SJ, Marchetti V, Lubas G, Guidi G. Double filtration plasmapheresis in a dog with multiple myeloma and hyperviscosity syndrome. Open Vet J. 2015; 5:108–112.
7. Matus RE, Gordon BR, Leifer CE, Saal S, Hurvitz AI. Plasmapheresis in five dogs with systemic immune-mediated disease. J Am Vet Med Assoc. 1985; 187:595–599.
8. Matus RE, Leifer CE, Gordon BR, MacEwen EG, Hurvitz AI. Plasmapheresis and chemotherapy of hyperviscosity syndrome associated with monoclonal gammopathy in the dog. J Am Vet Med Assoc. 1983; 183:215–218.
9. Matus RE, Schrader LA, Leifer CE, Gordon BR, Hurvitz AI. Plasmapheresis as adjuvant therapy for autoimmune hemolytic anemia in two dogs. J Am Vet Med Assoc. 1985; 186:691–693.
10. Proverbio D, Spada E, Perego R, de Giorgi GB. Seizures as a consequence of hyperviscosity syndrome in two dogs naturally infected with Leishmania infantum. J Am Anim Hosp Assoc. 2016; 52:119–123.

11. Sanchez AP, Cunard R, Ward DM. The selective therapeutic apheresis procedures. J Clin Apher. 2013; 28:20–29.

12. Siami GA, Siami FS. Plasmapheresis and paraproteinemia: cryoprotein-induced diseases, monoclonal gammopathy, Waldenström's macroglobulinemia, hyperviscosity syndrome, multiple myeloma, light chain disease, and amyloidosis. Ther Apher. 1999; 3:8–19.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download