1. Chow SC. Bioavailability and bioequivalence in drug development. Wiley Interdiscip Rev Comput Stat. 2014; 6:304–312. PMID:
25215170.

2. Sanchez MP, Ocana J, Carrasco JL. The effect of variability and carryover on average bioequivalence assessment: a simulation study. Pharm Stat. 2011; 10:135–142. PMID:
22432131.
3. Shen M, Russek-Cohen E, Slud EV. Letter to the editor by the authors of Exact Calculation of Power and Sample Size in Bioequivalence Studies Using Two One-sided Tests. Pharm Stat. 2015; 14:272. DOI:
10.1002/pst.1677. PMID:
25807931.
4. Ahmed S. A pooling methodology for coefficient of variation. Sankhya Ser B. 1995; 57:57–75.
5. Phillips KF. Power of the two one-sided tests procedure in bioequivalence. J Pharmacokinet Biopharm. 1990; 18:137–144. PMID:
2348380.

6. Chow SC, Wang H. On sample size calculation in bioequivalence trials. J Pharmacokinet Pharmacodyn. 2001; 28:155–169. PMID:
11381568.
7. Worley JW, Morrell JA, Duewer DL, Peterfreund LA. Alternate indexes of variation for the analysis of experimental data. Anal Chem. 1984; 56:462–466.

9. Chen ML, Shah V, Patnaik R, Adams W, Hussain A, Conner D, et al. Bioavailability and bioequivalence: an FDA regulatory overview. Pharm Res. 2001; 18:1645–1650. PMID:
11785681.
10. Yuen KH, Wong JW, Yap SP, Billa N. Estimated coefficient of variation values for sample size planning in bioequivalence studies. Int J Clin Pharmacol Ther. 2001; 39:37–40. PMID:
11204936.

12. Diletti E, Hauschke D, Steinijans VW. Sample size determination for bioequivalence assessment by means of confidence intervals. Int J Clin Pharmacol Ther Toxicol. 1991; 29:1–8. PMID:
2004861.
13. Diletti E, Hauschke D, Steinijans VW. Sample size determination for bioequivalence assessment by means of confidence intervals. Int J Clin Pharmacol Ther Toxicol. 1992; 30(Suppl 1):S51–S58. PMID:
1601532.
16. Ramirez E, Laosa O, Guerra P, Duque B, Mosquera B, Borobia AM, et al. Acceptability and characteristics of 124 human bioequivalence studies with active substances classified according to the Biopharmaceutic Classification System. Br J Clin Pharmacol. 2010; 70:694–702. DOI:
10.1111/j.1365-2125.2010.03757.x. PMID:
21039763.

17. Sato M, Narukawa M. Factors affecting intrasubject variability of PK exposure: absolute oral bioavailability and acidic nature of drugs. Int J Clin Pharmacol Ther. 2015; 53:955–962. DOI:
10.5414/CP202399. PMID:
26365336.

18. Harahap Y, Prasaja B, Azmi F, Lusthom W, Sinandang T, Felicia V, et al. Bioequivalence study of two rosuvastatin tablet formulations in healthy Indonesian subjects. Int J Clin Pharmacol Ther. 2016; 54:212–216. DOI:
10.5414/CP202345. PMID:
26073355.

19. Ju SY, Chen YC, Tzeng HK, Chen SW, Guo GT, Juan CH, et al. Bioequivalence Evaluation of Two Formulations of Celecoxib 200 mg Capsules in Healthy volunteers by using a validated LC/MS/MS method. Int J Bioanal Methods Bioequival Stud. 2015; 2:34–40.
20. Techatanawat I, Bhuket PRN, Teerawonganan P, Yoosakul E, Khaowroongrueng V, Paisarnsinsool W, et al. Bioequivalence study of duloxetine hydrochloride 60 mg ec capsules in the fasting and fed states in healthy Thai male volunteers. J Health Res. 2015; 29:165–169.
21. Davit BM, Chen ML, Conner DP, Haidar SH, Kim S, Lee CH, et al. Implementation of a reference-scaled average bioequivalence approach for highly variablegeneric drug products by the US Food and Drug Administration. AAPS J. 2012; 14:915–924. PMID:
22972221.
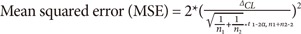
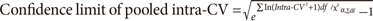
 : critical value of chi square estimates)
: critical value of chi square estimates)




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download