1. Nishida Y, Tsukushi S, Shido Y, Wasa J, Ishiguro N, Yamada Y. Successful treatment with meloxicam, a cyclooxygenase-2 inhibitor, of patients with extra-abdominal desmoid tumors: a pilot study. J Clin Oncol. 2010; 28(6):e107–e109. PMID:
20026797.

2. Patel SR, Evans HL, Benjamin RS. Combination chemotherapy in adult desmoid tumors. Cancer. 1993; 72(11):3244–3247. PMID:
8242548.

3. Weiss AJ, Lackman RD. Low-dose chemotherapy of desmoid tumors. Cancer. 1989; 64(6):1192–1194. PMID:
2766217.

4. Baumert BG, Spahr MO, Von Hochstetter A, et al. The impact of radiotherapy in the treatment of desmoid tumours: an international survey of 110 patients A study of the Rare Cancer Network. Radiat Oncol. 2007; 2:12. PMID:
17343751.

5. Sherman NE, Romsdahl M, Evans H, Zagars G, Oswald MJ. Desmoid tumors: a 20-year radiotherapy experience. Int J Radiat Oncol Biol Phys. 1990; 19(1):37–40. PMID:
2380093.

6. McCollough WM, Parsons JT, van der Griend R, Enneking WF, Heare T. Radiation therapy for aggressive fibromatosis: the experience at the University of Florida. J Bone Joint Surg Am. 1991; 73(5):717–725. PMID:
2045396.

7. Kinzbrunner B, Ritter S, Domingo J, Rosenthal CJ. Remission of rapidly growing desmoid tumors after tamoxifen therapy. Cancer. 1983; 52(12):2201–2204. PMID:
6640490.

8. Sportiello DJ, Hoogerland DL. A recurrent pelvic desmoid tumor successfully treated with tamoxifen. Cancer. 1991; 67(5):1443–1446. PMID:
1991311.

9. Fernberg JO, Brosjo O, Larsson O, Soderlund V, Strander H. Interferon-induced remission in aggressive fibromatosis of the lower extremity. Acta Oncol. 1999; 38(7):971–972. PMID:
10606429.

10. Leithner A, Schnack B, Katterschafka T, et al. Treatment of extra-abdominal desmoid tumors with interferon-alpha with or without tretinoin. J Surg Oncol. 2000; 73(1):21–25. PMID:
10649274.

11. Heinrich MC, McArthur GA, Demetri GD, et al. Clinical and molecular studies of the effect of imatinib on advanced aggressive fibromatosis (desmoid tumor). J Clin Oncol. 2006; 24(7):1195–1203. PMID:
16505440.

12. Mace J, Sybil Biermann J, Sondak V, et al. Response of extraabdominal desmoid tumors to therapy with imatinib mesylate. Cancer. 2002; 95(11):2373–2379. PMID:
12436445.

13. Dominguez-Malagon HR, Alfeiran-Ruiz A, Chavarria-Xicotencatl P, Duran-Hernandez MS. Clinical and cellular effects of colchicine in fibromatosis. Cancer. 1992; 69(10):2478–2483. PMID:
1568169.

14. Klein WA, Miller HH, Anderson M, DeCosse JJ. The use of indomethacin, sulindac, and tamoxifen for the treatment of desmoid tumors associated with familial polyposis. Cancer. 1987; 60(12):2863–2868. PMID:
2824015.

15. Waddell WR, Gerner RE. Indomethacin and ascorbate inhibit desmoid tumors. J Surg Oncol. 1980; 15(1):85–90. PMID:
7421272.

16. Skapek SX, Anderson JR, Hill DA, et al. Safety and efficacy of high-dose tamoxifen and sulindac for desmoid tumor in children: results of a Children's Oncology Group (COG) phase II study. Pediatr Blood Cancer. 2013; 60(7):1108–1112. PMID:
23281268.

17. Waddell WR, Kirsch WM. Testolactone, sulindac, warfarin, and vitamin K1 for unresectable desmoid tumors. Am J Surg. 1991; 161(4):416–421. PMID:
2035759.

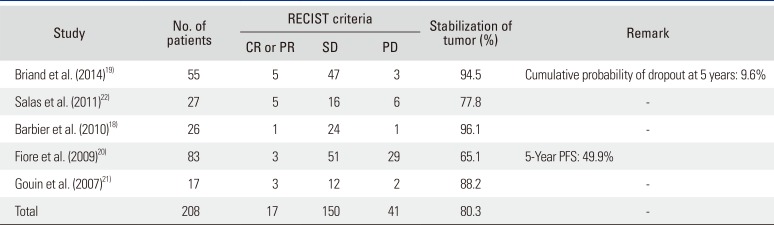
18. Barbier O, Anract P, Pluot E, et al. Primary or recurring extra-abdominal desmoid fibromatosis: assessment of treatment by observation only. Orthop Traumatol Surg Res. 2010; 96(8):884–889. PMID:
21075698.

19. Briand S, Barbier O, Biau D, et al. Wait-and-see policy as a first-line management for extra-abdominal desmoid tumors. J Bone Joint Surg Am. 2014; 96(8):631–638. PMID:
24740659.

20. Fiore M, Rimareix F, Mariani L, et al. Desmoid-type fibromatosis: a front-line conservative approach to select patients for surgical treatment. Ann Surg Oncol. 2009; 16(9):2587–2593. PMID:
19568815.

21. Gouin F, Tesson A, Bertrand-Vasseur A, Cassagnau E, Rolland F. Rating of tumoral growth in non-operated primary or recurrent extra-abdominal aggressive fibromatosis. Rev Chir Orthop Reparatrice Appar Mot. 2007; 93(6):546–554. PMID:
18065863.
22. Salas S, Dufresne A, Bui B, et al. Prognostic factors influencing progression-free survival determined from a series of sporadic desmoid tumors: a wait-and-see policy according to tumor presentation. J Clin Oncol. 2011; 29(26):3553–3558. PMID:
21844500.

23. Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000; 92(3):205–216. PMID:
10655437.
24. Prentice RL, Kalbfleisch JD, Peterson AV Jr, Flournoy N, Farewell VT, Breslow NE. The analysis of failure times in the presence of competing risks. Biometrics. 1978; 34(4):541–554. PMID:
373811.

25. Gronchi A, Casali PG, Mariani L, et al. Quality of surgery and outcome in extra-abdominal aggressive fibromatosis: a series of patients surgically treated at a single institution. J Clin Oncol. 2003; 21(7):1390–1397. PMID:
12663732.

26. Sobolewski C, Cerella C, Dicato M, Ghibelli L, Diederich M. The role of cyclooxygenase-2 in cell proliferation and cell death in human malignancies. Int J Cell Biol. 2010; 2010:215158. PMID:
20339581.

27. Francis WP, Zippel D, Mack LA, et al. Desmoids: a revelation in biology and treatment. Ann Surg Oncol. 2009; 16(6):1650–1654. PMID:
19306047.

28. Poon R, Smits R, Li C, et al. Cyclooxygenase-two (COX-2) modulates proliferation in aggressive fibromatosis (desmoid tumor). Oncogene. 2001; 20(4):451–460. PMID:
11313976.

29. Bonvalot S, Eldweny H, Haddad V, et al. Extra-abdominal primary fibromatosis: aggressive management could be avoided in a subgroup of patients. Eur J Surg Oncol. 2008; 34(4):462–468. PMID:
17709227.

30. von Mehren M, Benjamin RS, Bui MM, et al. Soft tissue sarcoma, version 2.2012: featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2012; 10(8):951–960. PMID:
22878820.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download