This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Intraosseous lipoma is a very rare lesion that constitutes no more than 0.1% of all bone tumors. We analyzed 21 cases of intraosseous lipoma at a single institution for clinical and radiographic characteristics.
Methods
A retrospective study was performed on 21 pathologically confirmed intraosseous lipomas treated in our hospital from 2000 to 2017. Simple X-ray and magnetic resonance imaging findings and medical records were reviewed. Patients' age, sex, and clinical symptoms were investigated. From the radiographic images, the site of the lesion, calcification, bony expansion, and stage of the lesion were evaluated. Correlations between the degree of involution and clinical symptoms were analyzed.
Results
The mean age of patients was 50 years (range, 20 to 67 years), and there were 13 males and eight females. The mean lesion size was 6.1 cm (range, 2.5 to 13.6 cm). The most common anatomical site of the lesion was the femur (seven cases), and three cases occurred in flat bones such as the ilium and scapula. Visual analogue scale score for pain was 3 to 6 in 15 patients. There were no complaints of functional limitation. There was no correlation between the degree of degeneration and clinical symptoms (p = 1.000). Curettage was performed as a surgical treatment in 20 patients, and bone graft was performed using a bone chip. Excision was performed in one patient. Pain was resolved in seven of 11 patients with a complaint of preoperative pain; intermittent pain remained in four cases. There was no local recurrence or malignant change during the follow-up.
Conclusions
There was no correlation between the degree of degeneration and clinical symptoms. Pain was the most common clinical symptom, but it was rarely accompanied by functional limitation. However, it is important to distinguish it from other pain-inducing disorders. The incidence of intraosseous lipomas is low, and detection based on various imaging findings can be difficult. Clear understanding of the radiographic findings and symptoms of intraosseous lipoma is helpful for diagnosis and differentiation.
Go to :

Keywords: Bone neoplasms, Intraosseous, Lipoma
Intraosseous lipoma is a very rare lesion that constitutes no more than 0.1% of all bone tumors.
1) It may undergo varying degrees of degenerative changes and manifests with areas of fat necrosis, cystic changes, and calcification. Based on histological findings, an intraosseous lipoma can be classified by Milgram classification system as follows: stage I, a lesion composed of mature fat cells without calcification; stage II, a predominantly fatty lesion with necrosis, focal calcification, or ossification; and stage III, a fat-containing lesion with multiple necroses, extensive calcification, and cystic degeneration.
2) Diagnosis of intraosseous lipoma with simple X-ray may not be easy. Pain is the major symptom reported by patients, but more than 30% of the cases are found incidentally on imaging studies performed for other reasons.
345) Intraosseous lipomas occur mainly in the lower limbs, but they can occur anywhere in the skeleton.
6) For this reason, the lesions are difficult to diagnose.
Contrary to previous studies centered on radiological findings and degree of histological degeneration,
267) this study focuses on radiographic and clinical characteristics of intraosseous lipoma. We reviewed intraosseous lipomas treated at our institution to elucidate the clinical and radiological characteristics and investigated the correlations between the stage of the lesion and clinical symptoms. In addition, postoperative results were analyzed.
METHODS
The study was approved by the Institutional Review Board of Kosin University Gospel Hospital (IRB No. 2016-11-032-001). The study included a total of 21 patients who were pathologically confirmed as having an intraosseous lipoma and treated at Kosin University Gospel Hospital from January 2000 to December 2017. The mean follow-up period was 17 months (range, 12 to 38 months). The diagnosis was made by radiographic and histological evaluation. The study was conducted retrospectively by reviewing plain radiographs, magnetic resonance imaging (MRI) scans, and medical records. Patients' age, sex, and clinical symptoms were investigated. From radiographic images (simple X-ray and MRI), the site of the lesion, pattern, calcification, bony expansion, and stage of the lesion were analyzed. MRI included T1-weighted, T2-weighted, and fat-suppressed images in all cases. Subjective symptoms reported by the patient and objective signs observed by the physician in physical examination were analyzed. Visual analogue scale (VAS) score was evaluated preoperatively and during the follow-up in patients with a complaint of pain.
We analyzed the correlations between the stage of the lesion and clinical symptoms. For this, the patients were divided according to the Milgram classification system into two groups, stage I group and stage III group. Treatment results were also analyzed.
Statistical analysis was performed using IBM SPSS ver. 24.0 (IBM Corp., Armonk, NY, USA). Fisher exact test was used to compare clinical symptoms between the two groups. We considered a p-value < 0.05 to indicate statistical significance.
Go to :

RESULTS
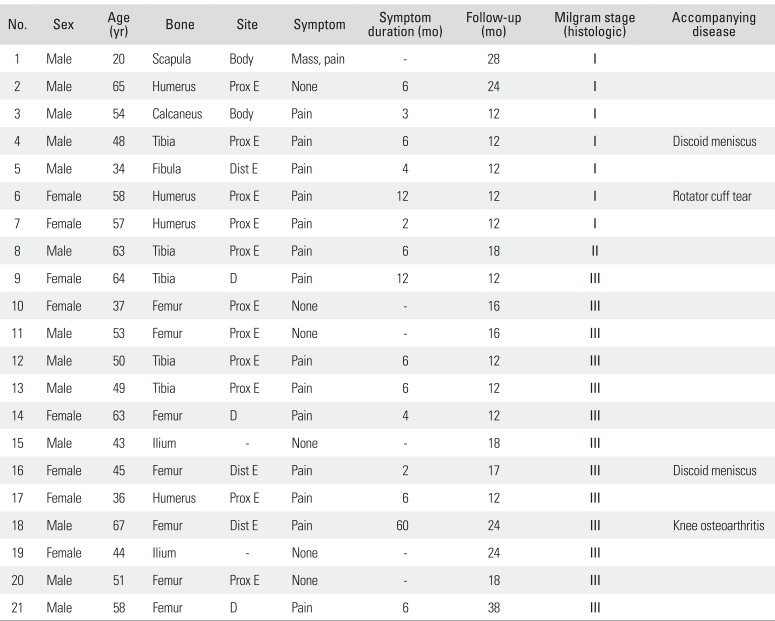
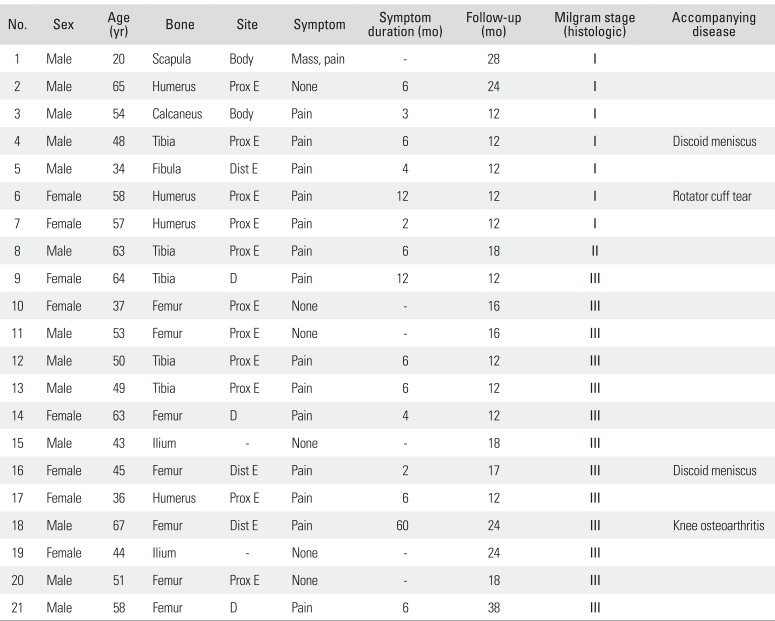
The mean age of the patients was 50 years (range, 20 to 67 years), and the study included 13 males and eight females. The mean size of the lesions was 6.1 cm (range, 2.5 to 13.6 cm). The most common anatomical site of the lesion was the femur in seven cases, and three cases occurred in flat bones such as the ilium and scapula (
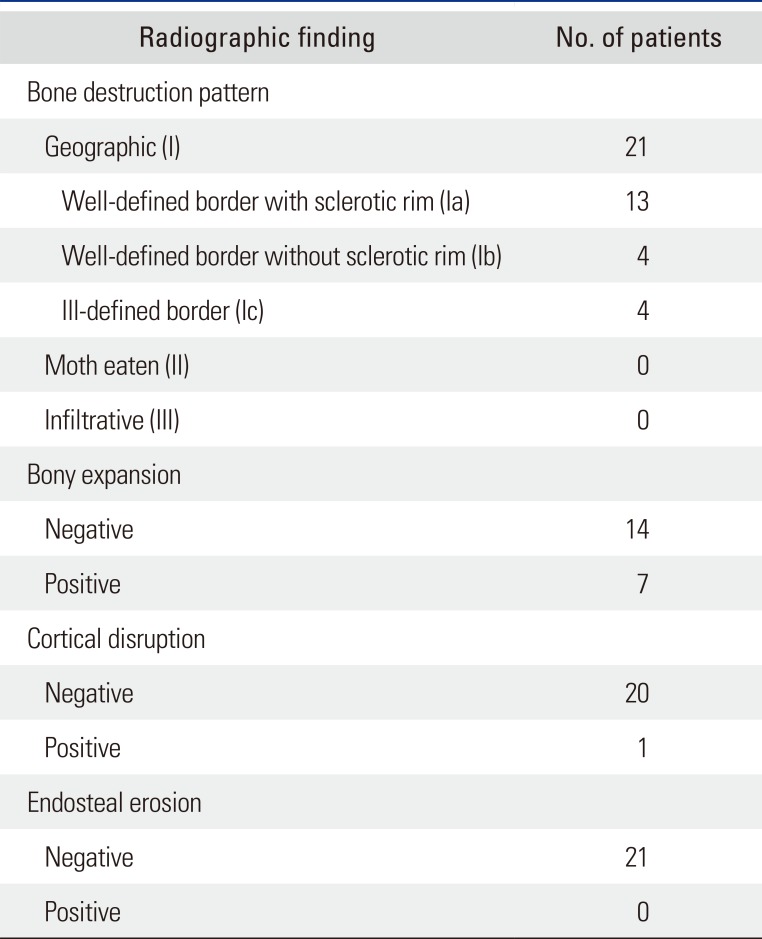
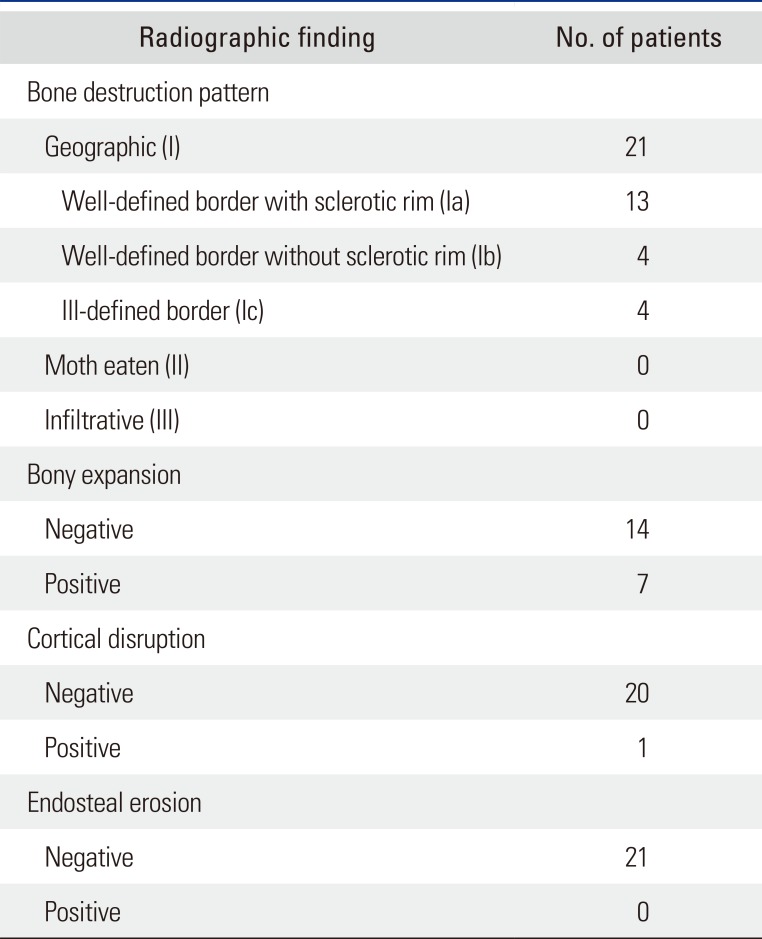
Table 1). The size of the lesion defined as the longest diameter of the lesion ranged from 2.5 cm to 13.6 cm; in 15 cases, the size was smaller than 6 cm. All lesions exhibited a geographic bone destruction pattern; 13 cases with a sclerotic rim, four cases without a sclerotic rim, and four cases with unclear margin. Bony expansion was observed in seven cases. There was one case in which cortical disruption was observed. Endosteal erosion was not observed (
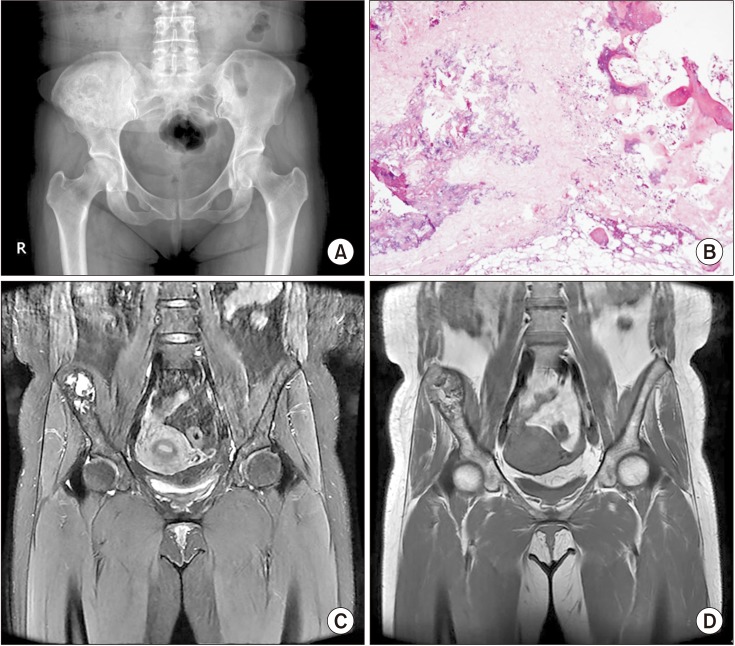
Table 2). Regarding the stage of the lesion according to the Milgram classification system, stage III was most common, which was found in 13 cases and accompanied by cystic formation and extensive calcification (
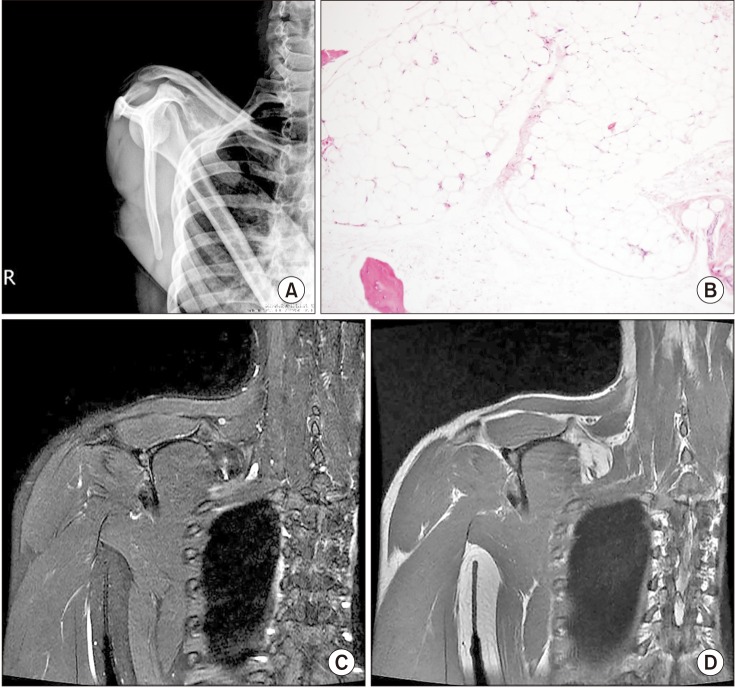
Fig. 1). Stage II was noted in one case and stage I, in seven cases (
Fig. 2). In 15 of 21 cases, the VAS score for pain was between 3 and 6. There were four cases with other causes of pain, such as osteoarthritis, rotator cuff tear, and discoid meniscus. Therefore, pain was caused by intraosseous lipoma in 11 cases. A palpable mass was present in one case. There was no range of motion limitation in all cases. In the stage I group, four of seven cases had pain; in the stage III group, six of 13 cases had pain. There was no correlation between the stage of the lesion and clinical symptoms (
p = 1.000). There were no local recurrences or malignant changes during the follow-up. Curettage was performed as a surgical treatment in 20 cases, and bone graft was performed using a bone chip. Excision was performed in one case. Pain was resolved in seven of 11 cases with a complaint of preoperative pain. In four cases, intermittent pain remained.
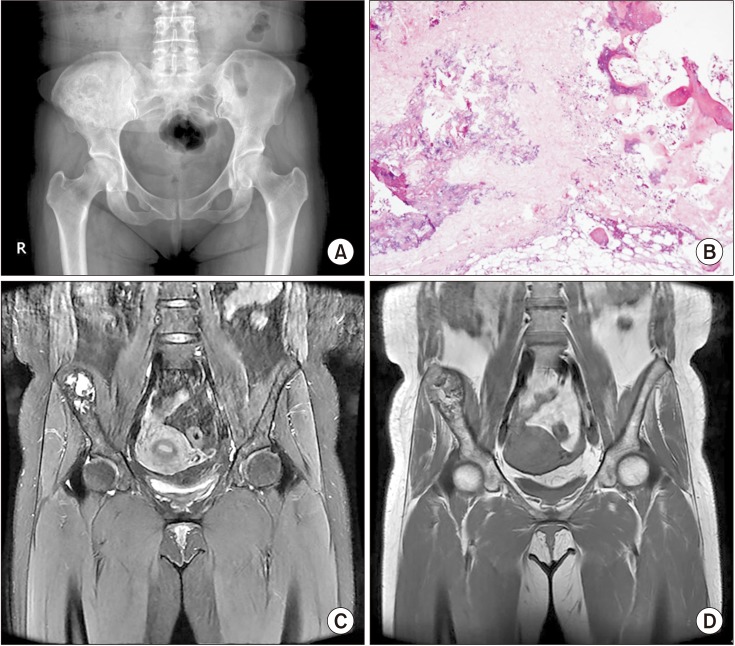 | Fig. 1A 44-year-old woman with an intraosseous lipoma (late phase) in the right ilium. (A) The anteroposterior pelvic radiograph shows a sclerotic-margined and expansile bone lesion in the right iliac bone. (B) Low power photomicrograph demonstrating fat necrosis with fine, powdery calcification and fibrosis, similar to what is seen in bone infarct. These features represent the late stage intraosseous lipoma (H&E, ×100). (C) On fat-suppressed coronal T2-weighted magnetic resonance imaging, the mass has high signal intensity centrally, indicating cystic necrotic portions. (D) On coronal T1-weighted magnetic resonance imaging, the mass demonstrates well-defined fat signal intensity with a central area of low signal intensity due to cystic change.
|
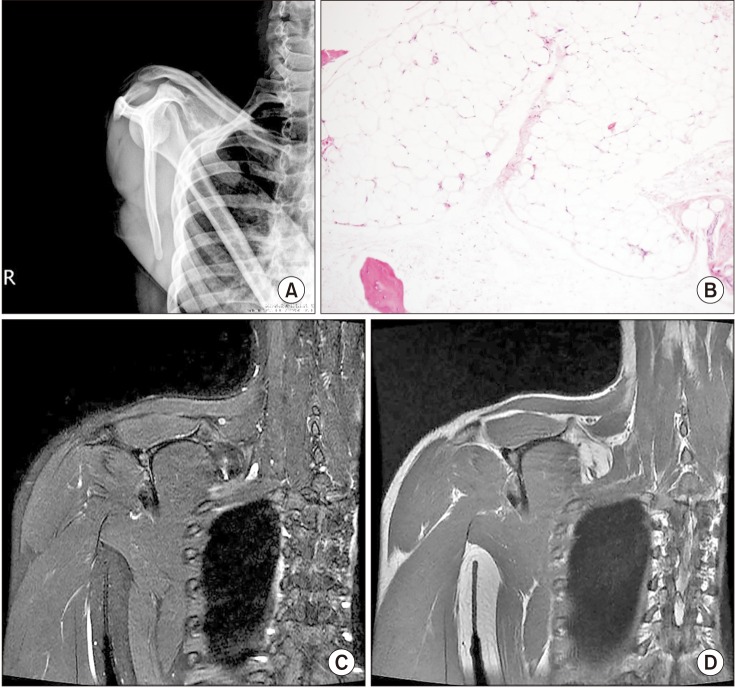 | Fig. 2A 20-year-old man with an intraosseous lipoma (early phase) in the body of scapula. (A) The outlet view shoulder radiograph demonstrates an expansile bone lesion at the body of the right scapula. (B) Photomicrograph of the lesion consisting of mature adipocytes, similar to fatty marrow. However, there is no evidence of bone marrow elements (H&E, ×100). (C) On fat-suppressed coronal T2-weighted magnetic resonance imaging, the mass shows signal dropout with fat suppression. (D) On coronal T1-weighted magnetic resonance imaging, the corresponding lesion is isointense to subcutaneous fat.
|
Table 1
Clinical Characteristics of Intraosseous Lipoma
|
No. |
Sex |
Age (yr) |
Bone |
Site |
Symptom |
Symptom duration (mo) |
Follow-up (mo) |
Milgram stage (histologic) |
Accompanying disease |
|
1 |
Male |
20 |
Scapula |
Body |
Mass, pain |
- |
28 |
I |
|
|
2 |
Male |
65 |
Humerus |
Prox E |
None |
6 |
24 |
I |
|
|
3 |
Male |
54 |
Calcaneus |
Body |
Pain |
3 |
12 |
I |
|
|
4 |
Male |
48 |
Tibia |
Prox E |
Pain |
6 |
12 |
I |
Discoid meniscus |
|
5 |
Male |
34 |
Fibula |
Dist E |
Pain |
4 |
12 |
I |
|
|
6 |
Female |
58 |
Humerus |
Prox E |
Pain |
12 |
12 |
I |
Rotator cuff tear |
|
7 |
Female |
57 |
Humerus |
Prox E |
Pain |
2 |
12 |
I |
|
|
8 |
Male |
63 |
Tibia |
Prox E |
Pain |
6 |
18 |
II |
|
|
9 |
Female |
64 |
Tibia |
D |
Pain |
12 |
12 |
III |
|
|
10 |
Female |
37 |
Femur |
Prox E |
None |
- |
16 |
III |
|
|
11 |
Male |
53 |
Femur |
Prox E |
None |
- |
16 |
III |
|
|
12 |
Male |
50 |
Tibia |
Prox E |
Pain |
6 |
12 |
III |
|
|
13 |
Male |
49 |
Tibia |
Prox E |
Pain |
6 |
12 |
III |
|
|
14 |
Female |
63 |
Femur |
D |
Pain |
4 |
12 |
III |
|
|
15 |
Male |
43 |
Ilium |
- |
None |
- |
18 |
III |
|
|
16 |
Female |
45 |
Femur |
Dist E |
Pain |
2 |
17 |
III |
Discoid meniscus |
|
17 |
Female |
36 |
Humerus |
Prox E |
Pain |
6 |
12 |
III |
|
|
18 |
Male |
67 |
Femur |
Dist E |
Pain |
60 |
24 |
III |
Knee osteoarthritis |
|
19 |
Female |
44 |
Ilium |
- |
None |
- |
24 |
III |
|
|
20 |
Male |
51 |
Femur |
Prox E |
None |
- |
18 |
III |
|
|
21 |
Male |
58 |
Femur |
D |
Pain |
6 |
38 |
III |
|

Table 2
Radiographic Characteristics of Intraosseous Lipoma
|
Radiographic finding |
No. of patients |
|
Bone destruction pattern |
|
|
Geographic (I) |
21 |
|
Well-defined border with sclerotic rim (Ia) |
13 |
|
Well-defined border without sclerotic rim (Ib) |
4 |
|
Ill-defined border (Ic) |
4 |
|
Moth eaten (II) |
0 |
|
Infiltrative (III) |
0 |
|
Bony expansion |
|
|
Negative |
14 |
|
Positive |
7 |
|
Cortical disruption |
|
|
Negative |
20 |
|
Positive |
1 |
|
Endosteal erosion |
|
|
Negative |
21 |
|
Positive |
0 |

Go to :

DISCUSSION
Intraosseous lipoma is a very rare lesion that constitutes no more than 0.1% of all bone tumors.
1) No sex differences in the incidence have been reported.
28) In our study, 13 patients were males and eight were females. The age range of patients at presentation is wide, from youth to elderly, with high incidence in the fourth, fifth, and sixth decades of life.
289101112) In our study, the mean age of the patients was 50 years (range, 20 to 67 years). The fifth decade was most common, in seven of 21 patients.
The calcaneus and long tubular bones are the common anatomical sites of the lesion.
2610) When located in long bones, the lesion tends to be found in the metaphysis.
2610) But, intraosseous lipomas can be found essentially anywhere in the skeleton. Cases in the spine, pelvic bone, skull, and rib have been reported.
2610) In our study, as in a previous study, long tubular bones were common anatomical locations. The most common anatomical site of the lesion was the femur in seven cases, followed by the tibia in five cases and the humerus in four cases. Flat bones such as the ilium and scapula were the anatomical locations in three cases. Compared with previous studies, there was no notable difference in terms of sex distribution, age, and anatomical locations. However, there were differences among studies
2367) probably due to differences in diagnostic methods (histological/radiological confirmation) and the development of imaging studies which may have resulted in the decrease in histological confirmation.
The pathogenesis of intramedullary lipoma has not been clarified. Several hypotheses have been proposed including secondary bone reaction after trauma, healing reaction of osteonecrosis, and primary benign tumors.
2131415) It has been postulated that a secondary change in the tumor is due to an increase in pressure in the bone caused by proliferation of adipocytes.
213) Milgram proposed a three-stage classification system based on the histological appearance of intraosseous lipomas: stage I, a lesion composed of mature fat cells without calcification; stage II, a predominantly fat lesion with necrosis and focal calcification or ossifications; and stage III, a fat-containing lesion with multiple necroses, wide calcification, and cystic degeneration.
2) The distribution of Milgram stages vary across studies.
237) In our study, stage III was most common, seen in 13 cases, stage II was noted in one case and stage I, in seven cases.
Pain is the leading symptom in most cases, but more than 30% of bone lipomas are found incidentally on imaging studies performed for other reasons. Some authors have reported up to 70% of patients with intraosseous lipomas presented with pain,
616) while other authors described most patients as asymptomatic.
212) In this study, 15 of 21 cases complained of pain. Excluding osteoarthritis, rotator cuff tear, and discoid meniscus as the causes of pain, 11 patients complained of pain related to the lipoma. A palpable mass was present in one case in the scapula body; the lesion had an expansile pattern. No functional limitations were observed in all cases; therefore, it is necessary to distinguish the lesion from other sources of pain when there is functional limitation.
This study was based on the hypothesis that the degree of degenerative changes is related to increased intraosseous pressure. We investigated the relationship between the degree of degeneration and clinical symptoms (pain) with an assumption that severe degenerated changes would manifest with severe clinical symptoms. However, there was no correlation between the degree of degeneration and clinical symptoms (p = 1.000). Considering that stage I cases with no clinical symptoms may be excluded from studies based on surgical histological examinations, more studies on radiologically confirmed cases are needed for better understanding of intraosseous lipoma.
Radiological follow-up with conservative treatment is recommended, except for rare cases with risk of pathological fractures or malignant transformation.
217) Goto et al.
12) suggested surgical indications of intraosseous lipoma as follows: (1) painful tumor, (2) occurrence of pathological fracture, (3) necessity for histological diagnosis, and (4) need to decrease the risk of malignant transformation.
12) We performed curettage and packing with bone chips for surgical treatment in 20 cases. Excision was performed in one case. The indication for surgical treatment was symptomatic tumor (pain, mass) in 16 cases and necessity for histological diagnosis in five cases. Pain was resolved in seven of 11 cases with a complaint of preoperative pain. In cases presenting with clinical symptoms, surgical treatment (curettage, excision) is considered necessary; however, it is important to differentiate it from other pain-inducing disorders.
The limitations of this study include evaluation of only patients from a single institution. In addition, due to the nature of the lesion, the number of cases was not sufficient, and the follow-up period was short.
Intraosseous lipoma undergoes various degenerative changes according to the stage of the lesion. It occurs commonly in long bones of the lower limb and often in flat bones. There was no noticeable correlation between the degree of degeneration and clinical symptoms. Pain was the most common clinical symptom, but it was rarely accompanied by functional limitation. However, it is important to differentiate it from other sources of pain. The incidence of intraosseous lipomas is low, and various imaging findings make clinical diagnosis difficult. Clear understanding of the radiographic findings and symptoms will be useful for diagnosis and differentiation.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download