Abstract
Background
Periprosthetic fractures around a total knee replacement (TKR) can be complex and difficult to manage, requiring the surgical expertise of the trauma and arthroplasty surgeon. There are a number of treatment modalities available, each with their own merits and limitations. As data on tumor prosthesis revision in periprosthetic fractures is sparse, this study aims to evaluate the results of revision using a tumor prosthesis and compare them with those of fixation using a locking plate in periprosthetic fractures after TKR.
Methods
This is a retrospective study of 15 patients who underwent either tumor prosthesis revision (n = 7) or locking plate fixation (n = 8) for supracondylar femoral periprosthetic fractures in our hospital from 2009 and 2014. The mean follow-up time for these patients was 44 months. This study's main outcome measures were pain relief, return to premorbid ambulatory function, and complications.
Results
The revision and fixation groups saw five versus three patients achieve pain relief (71.4% vs. 37.5%, p = 0.315), and two versus four patients return to their premorbid ambulatory function (28.6% vs. 50%, p = 0.608) at the follow-up, respectively. The mean time to weight-bearing in the revision group and fixation group was 2.9 days and 18.9 weeks, respectively (p = 0.001). There were eight complications seen in the revision group with none requiring reoperation; there were five complications seen in the fixation group, and two required reoperation.
The number of total knee replacements (TKRs) will continue to increase as patients live longer and lead more active lives. Hence, we can expect a corresponding rise in the number of TKR complications. Periprosthetic fractures that are associated with TKRs have an incidence of 0.3%–2.5%, which will be a growing challenge for the orthopaedic surgeon to fix or revise.1) They may occur in the distal femur, proximal tibia, patella, or a combination of the three. The most common fracture site is the supracondylar region of the distal femur, which will be the focus of this study.23) Factors that may predispose a TKR patient to this complication are advanced age, female sex, osteoporosis, prolonged steroid use, rheumatoid arthritis and neurological conditions.345)
Supracondylar femoral periprosthetic fractures can be complex and difficult to manage, requiring the surgical expertise of the trauma and arthroplasty surgeon. There are a number of treatment modalities available, ranging from locking plates, intramedullary nailing and revision arthroplasty, each with their own set of merits and limitations.678) Though there are many studies on the various treatment modalities, there are few on tumor prosthesis revision. These studies on tumor prosthesis revision have thus far reported encouraging results, though have cautioned against its use due to their high complication rates, suggesting it as a salvage option.910) Therefore, this study aims to evaluate the results of tumor prosthesis revision for post-TKR periprosthetic fractures, and compare them with fixation using locking plates.
A retrospective study was conducted on patients who underwent either revision with a tumor prosthesis or fixation with locking plates for supracondylar femoral periprosthetic fractures in Tan Tock Seng Hospital from January 2009 through December 2014. Institutional Review Board approval was obtained prior to performing this study (DSRB Reference No. 2015/00586). There was no informed consent obtained from patients.
Patients were identified using our department's electronic patient database. Patient demographics, fracture characteristics, and surgical data were retrieved from their paper notes and electronic records. Their postoperative recovery and complications were recorded as well. This study's main outcome measures were pain relief, return to premorbid ambulatory function, and complications.
The fracture patterns were classified according to the Rorabeck and Taylor classification as presented in Table 1.11) Plain radiographs and/or computed tomography scans were used to assess implant loosening and bone loss. The decision for tumor prosthesis revision versus locking plate fixation was made by the managing surgeons. This decision for tumor prosthesis revision was based on the Rorabeck classification (pre-existing symptoms or radiological signs of implant loosening) and/or a lack of adequate bone stock for stable fixation. The prosthesis included in the revision group was the Zimmer Segmental System (Zimmer, Warsaw, IN, USA). The surgical technique for tumor prosthesis revision was performed via the medial parapatellar approach. The distal femur was resected with an oscillating saw and prepared by canal reaming and calcar planning. Next, the tibial component was explanted with a reciprocating saw and stacked osteotomes, prepared by canal reaming and a tibial cut made with an extramedullary jig. The tumor prosthesis was finally implanted with third generation cementing, and the wound was closed in layers. Postoperative surgical drains were used (Fig. 1).
The locking plates included in the fixation group was the Less Invasive Stabilisation System (Synthes, West Chester, PA, USA) as well as the periarticular distal femoral locking plate (Zimmer) and NCB Distal Femur System (Zimmer). The exclusion criteria in our sample were patients who sustained a unilateral Rorabeck type I or bilateral supracondylar femoral periprosthetic fracture. Postoperatively, the revision group was allowed full weight bearing as tolerated. As for the fixation group, patients were kept nonweight bearing for a minimum duration of 6 weeks before being allowed progressive weight-bearing from partial to full weight based on the clinical and radiographic signs of fracture healing (Fig. 2).
Microsoft Excel 2013 (Microsoft, Redmond, WA, USA) was used for generation of descriptive statistics. The continuous data was checked for normality using the Shapiro-Wilk test. Depending on the normality of the data, t-test or Mann-Whitney U-test was used. As for the categorical data, Fisher exact test was used. Statistical significance was defined as a p-value of < 0.05.
There were 15 patients identified for this study: seven tumor prosthesis revisions and eight locking plate fixations. The mean age of the patients was 76.7 years (range, 63 to 86 years) in the revision group and 67.9 years (range, 56 to 78 years) in the fixation group, with a difference that is statistically insignificant (p = 0.055). All patients were female. Their medical comorbidities are presented in Table 2. The mean American Society of Anaesthesiologists physical status grade according to the severity of systemic disease was 2.57 and 2.38, respectively, with a difference also found to be statistically insignificant (p = 0.483). The mechanism of injury for all patients were minor falls, except for one early postoperative fracture from the index operation at 3 weeks in the revision group. The fracture characteristics are presented in Table 2. It was noted that the difference in comminution between the groups was statistically significant (p = 0.04).
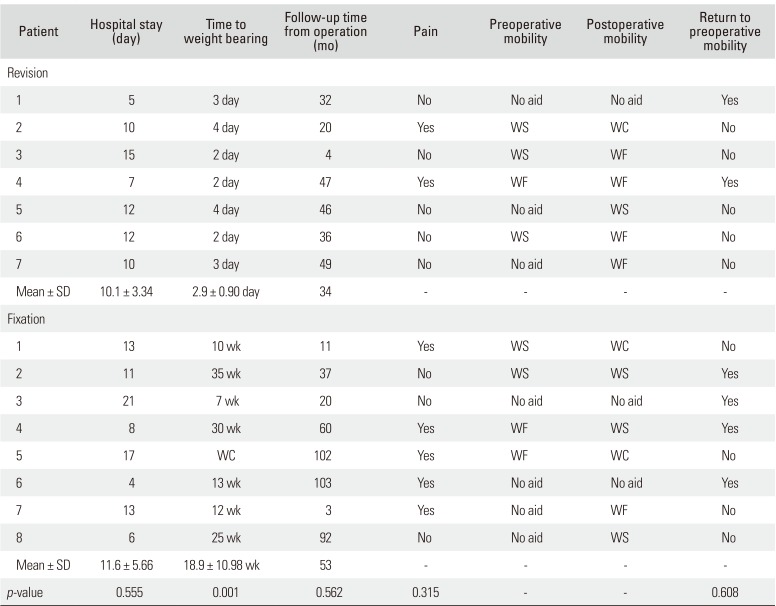
The operative findings are presented in Table 3. The difference in anaesthesia and operative timings were statistically insignificant, with a p-value of 0.342 in the revision group and 0.119 in the fixation group. There were no intraoperative complications, much less as a direct result of tourniquet use. Patient outcomes from the two groups with a mean follow-up period of 44 months are presented in Table 4. In the revision group, five (71.4%) were pain-free and two (28.6%) had returned to their premorbid ambulatory status by a mean follow-up time of 34 months. As for the fixation group, three (37.5%) were pain-free and four (50%) had returned to their premorbid ambulatory status by a mean follow-up time of 53 months. The difference in follow-up time was statistically insignificant (p = 0.562). The mean time to weight-bearing in the revision group and fixation group was 2.9 days to 18.9 weeks, respectively, a difference that is statistically significant (p = 0.001).
From the revision group of seven patients, there were eight complications seen in six patients: six (85.7%) developed postoperative anaemia that required two or more blood transfusions; two (28.6%) developed fast atrial fibrillation as a result of postoperative pain, which was managed with rate-controlling beta-blockade and analgesia optimisation. The mean hospital stay for the revision group was 10.1 days (range, 5 to 15 days). There were no complications that required reoperation. For the fixation group of eight, there were five complications seen in three patients: one (12.5%) developed postoperative anaemia that required two or more blood transfusions; two (25%) developed uncomplicated urinary tract infection as a result of immobility, which was treated with a short course of antibiotics. The mean hospital stay for the fixation group was 11.6 days (range, 4 to 21 days).
However, there were two complications seen in two patients in the fixation group that required reoperation. One patient (12.5%) was readmitted within a month of discharge for deep wound infection. Tissue cultures grew methicillin-resistant Staphylococcus aureus, which was treated with culture-directed antibiotics, and multiple wound debridement and subsequent plate removal. The TKR prosthesis was left in situ. The inpatient stay was 59 days. The fracture later healed in malunion and the patient mobilized in a wheelchair. The other patient (12.5%) was found to have septic nonunion at 13 months from the fixation operation. Tissue cultures grew S. aureus and group B streptococcus, which was treated with culture-directed antibiotics. The patient underwent two-staged knee fusion and subsequently mobilized in a wheelchair.
There were two patients, one from each group, with less than 1-year follow-up. The patient from the revision group was followed up for 4 months and was pain-free, mobilising with a walking frame, from a walking stick premorbidly. The patient died from end stage renal failure at 18 months postoperatively. As for the patient from the fixation group, the patient was followed up for 3 months, and was pain-free and mobilising with a walking frame, from no need for aids premorbidly. This patient died from urosepsis at 46 months postoperatively. There was another unrelated death in the revision group at 16 months postoperatively.
We have presented 15 patients who received either a tumor prosthesis revision or a locking plate fixation in our hospital for a supracondylar femoral periprosthetic fracture between 2009 and 2014. The proportion of patients who were pain-free was 71.4% in the revision group and 37.5% in the fixation group, and the proportion of those who had returned to their premorbid ambulatory status was 28.6% and 50%, respectively. There were complications seen in six revisions and three fixation patients, of which two fixation patients required reoperation.
The indications for tumor prosthesis revision versus locking plate fixation were based on the Rorabeck classification (pre-existing symptoms or radiological signs of implant loosening) and/or the adequacy of bone stock available for stable fixation. Tumor prosthesis revision was indicated for type 3 fractures, and type 2 fractures with severe comminution or bone loss that precluded fixation. As for locking plate fixation, it was indicated for type 2 fractures with adequate bone stock to allow for stable fixation.
There have been studies on the broader application of tumor prosthesis in nontumor cases, with positive outcomes in both pain reduction and function restoration.12) Of the few that looked specifically at tumor prosthesis for periprosthetic fractures, Jassim et al.9) reviewed 11 patients (mean age, 81 years) who underwent tumor prosthesis revision using one prosthesis model for periprosthetic fracture around the distal femoral component and reported acceptable clinical and functional outcomes at 33 months. Mortazavi et al.10) reviewed 20 patients (mean age, 69.5 years) who underwent revision with distal femoral arthroplasty replacement using three different prosthesis, reporting promising clinical and functional outcomes at 58.6 months. In keeping with these findings, our study's revision group has shown encouraging outcomes. Our study's revision and fixation groups saw five versus three patients achieve pain relief (71.4% vs. 37.5%, p = 0.315), and two versus four patients return to their premorbid ambulatory function (28.6% vs. 50%, p = 0.608) at follow-up, respectively. However, these differences were statistically insignificant.
Despite the positive outcomes from tumor prosthesis revision, studies have cautioned against its use because of the reportedly high complication rates. Springer et al.13) reported complications in eight out of the 25 patients reviewed, of which deep infection was the commonest. Pour et al.14) reported a high complication rate, with treatment failures as a result of aseptic loosening, periprosthetic infection and periprosthetic fracture. Though there have also been studies that reported low and even no complications from the distal femoral replacement for supracondylar periprosthetic fractures, their follow-up period was short at 6 months.1516)
Studies that looked specifically at tumor prosthesis for periprosthetic fractures reported high complication rates. Mortazavi et al.10) reported complications in 11 out of 20 patients, with five requiring additional surgery. Jassim et al.9) reported complications in six out of 11 patients, though with none requiring further operation. This was similarly seen in our study's revision group: complications in six out of seven patients with none requiring reoperation. According to Clavien-Dindo classification of surgical complications, all of the revision group's complications were grade II, which is relatively minor.17) Although the fixation group had a lower complication rate of three out of eight patients, there were two grade IIIB complications of deep wound infection and septic nonunion requiring reoperation.
The significance of revision over fixation is the mean time to weight-bearing. Cannon15) had seen all 27 patients mobilise rapidly after endoprosthetic replacement with positive clinical and functional outcomes and low complications rates at 6 months. Though five out of seven of our study's revision group required additional assistance beyond their premorbid ambulatory function at follow-up, their immediate postoperative full weight-bearing status may have afforded them an improvement in quality of life and a reduction of the risks of immobility.18) It has been seen in our study's fixation group that two patients have developed urinary tract infections, as a likely result of immobility. These concerns are especially shared with the older patients, who are less likely to be able to tolerate weight-bearing restrictions and immobility.
This is a retrospective study comparing outcomes of two different surgical modalities. The sample size in this study was small and both groups of patients were not well matched. Due to the small sample size, data from two patients with less than 1-year follow-up were included in the analysis.
The management of supracondylar femoral periprosthetic fractures continues to be a challenge for the surgeon and the patient. The results of revision TKR using a tumor prosthesis were comparable to those of fixation using a locking plate in periprosthetic fractures after TKR. Though tumor prosthesis revision had higher complication rates, they were minor and did not require reoperation. Tumor prosthesis revision may be considered as a viable alternative to locking plate fixation when indicated.
References
1. Rorabeck CH, Taylor JW. Periprosthetic fractures of the femur complicating total knee arthroplasty. Orthop Clin North Am. 1999; 30(2):265–277. PMID: 10196428.

2. Cordeiro EN, Costa RC, Carazzato JG, Silva Jdos S. Periprosthetic fractures in patients with total knee arthroplasties. Clin Orthop Relat Res. 1990; (252):182–189. PMID: 2302883.

3. Dennis DA. Periprosthetic fractures following total knee arthroplasty. J Bone Joint Surg Am. 2001; 83(1):119–130.

4. Culp RW, Schmidt RG, Hanks G, Mak A, Esterhai JL Jr, Heppenstall RB. Supracondylar fracture of the femur following prosthetic knee arthroplasty. Clin Orthop Relat Res. 1987; (222):212–222.

5. Chen F, Mont MA, Bachner RS. Management of ipsilateral supracondylar femur fractures following total knee arthroplasty. J Arthroplasty. 1994; 9(5):521–526. PMID: 7807110.

6. Healy WL, Siliski JM, Incavo SJ. Operative treatment of distal femoral fractures proximal to total knee replacements. J Bone Joint Surg Am. 1993; 75(1):27–34. PMID: 8419387.

7. Ritter MA, Keating EM, Faris PM, Meding JB. Rush rod fixation of supracondylar fractures above total knee arthroplasties. J Arthroplasty. 1995; 10(2):213–216. PMID: 7798104.

8. Johnston AT, Tsiridis E, Eyres KS, Toms AD. Periprosthetic fractures in the distal femur following total knee replacement: a review and guide to management. Knee. 2012; 19(3):156–162. PMID: 21741844.

9. Jassim SS, McNamara I, Hopgood P. Distal femoral replacement in periprosthetic fracture around total knee arthroplasty. Injury. 2014; 45(3):550–553. PMID: 24268192.

10. Mortazavi SM, Kurd MF, Bender B, Post Z, Parvizi J, Purtill JJ. Distal femoral arthroplasty for the treatment of periprosthetic fractures after total knee arthroplasty. J Arthroplasty. 2010; 25(5):775–780. PMID: 20171053.

11. Rorabeck CH, Taylor JW. Classification of periprosthetic fractures complicating total knee arthroplasty. Orthop Clin North Am. 1999; 30(2):209–214. PMID: 10196422.

12. Berend KR, Lombardi AV Jr. Distal femoral replacement in nontumor cases with severe bone loss and instability. Clin Orthop Relat Res. 2009; 467(2):485–492. PMID: 18523831.

13. Springer BD, Sim FH, Hanssen AD, Lewallen DG. The modular segmental kinematic rotating hinge for nonneoplastic limb salvage. Clin Orthop Relat Res. 2004; (421):181–187.

14. Pour AE, Parvizi J, Slenker N, Purtill JJ, Sharkey PF. Rotating hinged total knee replacement: use with caution. J Bone Joint Surg Am. 2007; 89(8):1735–1741. PMID: 17671012.
15. Cannon SR. The use of megaprosthesis in the treatment of periprosthetic knee fractures. Int Orthop. 2015; 39(10):1945–1950. PMID: 26311510.

16. Saidi K, Ben-Lulu O, Tsuji M, Safir O, Gross AE, Backstein D. Supracondylar periprosthetic fractures of the knee in the elderly patients: a comparison of treatment using allograft-implant composites, standard revision components, distal femoral replacement prosthesis. J Arthroplasty. 2014; 29(1):110–114. PMID: 23680503.

17. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240(2):205–213. PMID: 15273542.
18. Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995; 77(10):1551–1556. PMID: 7593064.

Fig. 1
(A) Radiographs of a left supracondylar femoral periprosthetic fracture (Rorabeck type 3) requiring revision in the anteroposterior view (left) and lateral view (right). (B) Radiographs of a left supracondylar femoral periprosthetic fracture treated with tumor prosthesis revision 1 month postoperatively in the anteroposterior view (left) and lateral view (right).
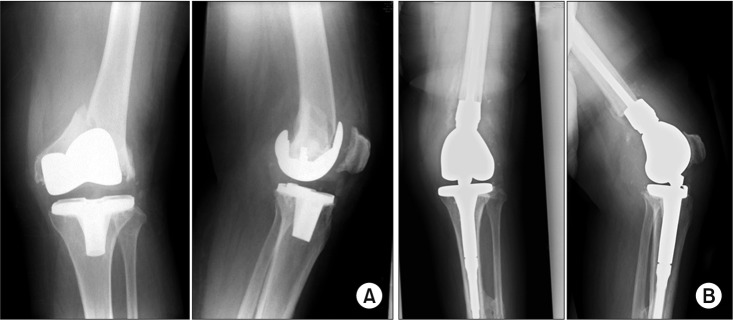
Fig. 2
(A) Radiographs of a left comminuted supracondylar femoral periprosthetic fracture (Rorabeck type 2) with good bone stock amenable to fixation in the anteroposterior view (left) and lateral view (right). (B) Radiographs of the left comminuted supracondylar femoral periprosthetic fracture treated with locking plate fixation on postoperative day 1 in the anteroposterior view (left) and lateral view (right). (C) Bony union on 21-month postoperative anteroposterior (left) and lateral (right) radiographs.
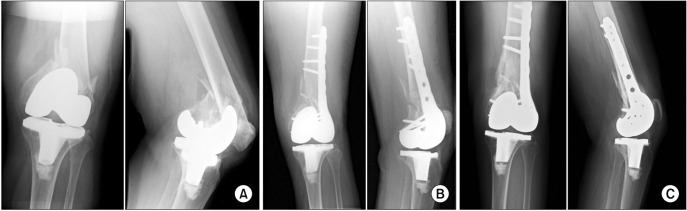
Table 1
Rorabeck and Taylor Classification11)
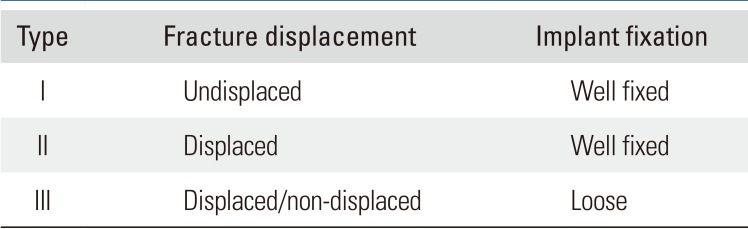
| Type | Fracture displacement | Implant fixation |
|---|---|---|
| I | Undisplaced | Well fixed |
| II | Displaced | Well fixed |
| III | Displaced/non-displaced | Loose |
Table 2
Patient Demographic Details and Fracture Characteristics
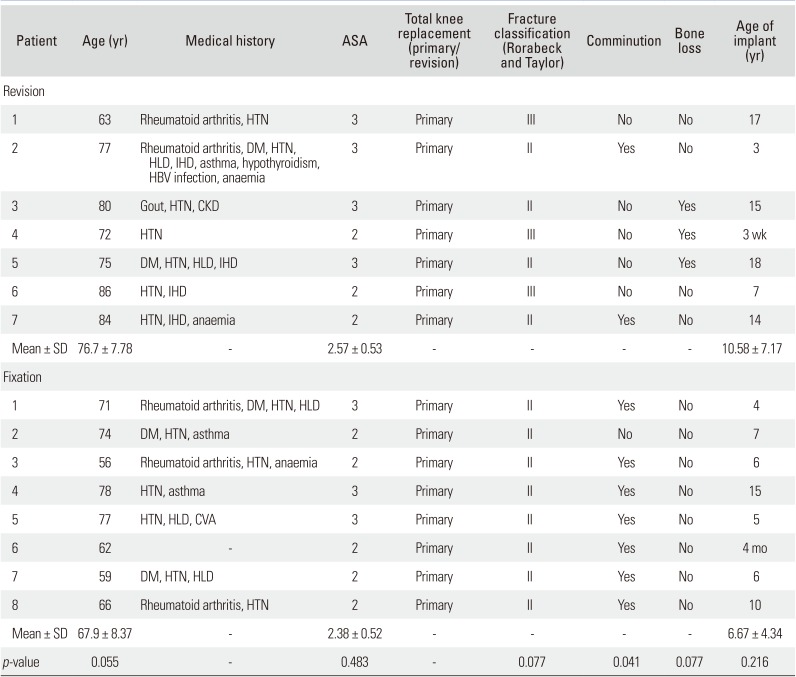
Table 3
Surgical Data
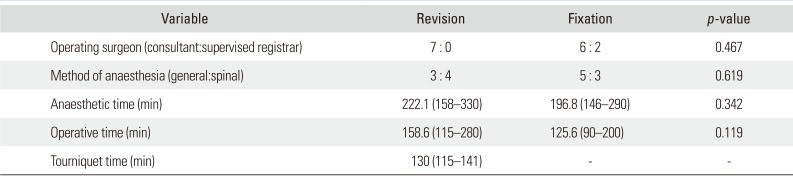
Table 4
Patient's Outcomes




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download