Abstract
Background
Cortical suspensory femoral fixation is commonly performed for graft fixation to the femur in anterior cruciate ligament (ACL) reconstruction using hamstring tendons. The purpose of this study was to compare graft healing in the femoral tunnel, implant-related failure, and clinical results between fixed- and adjustable-length loop devices in outside-in ACL reconstruction.
Methods
A total of 109 patients who underwent ACL reconstruction using the outside-in technique from December 2010 to July 2014 were included. For femoral graft fixation, a fixed-length loop device was used in 48 patients (fixed-loop group) and an adjustable-length loop device was used in 61 patients (adjustable-loop group). For evaluation of graft healing in the femoral tunnel, magnetic resonance imaging was performed at postoperative 6 months and the signal-to-noise ratios (SNRs) of the tendon graft and tendon-bone interface in the femoral bone tunnel were evaluated. The presence of synovial fluid was evaluated to determine loop lengthening at the femoral tunnel exit. Clinical results assessed using International Knee Documentation Committee score, Tegner-Lysholm Knee Scoring scale, and knee instability tests were compared between groups.
Results
The SNRs of the tendon graft and tendon-bone interface were not statistically different between groups. The presence of synovial fluid at the femoral exit showed no statistical difference between groups. Clinical results were not significantly different between groups.
Conclusions
The adjustable-length loop device provided comparable graft healing, implant-related failure, and clinical results with the fixed-length loop device, allowing adaptation of the graft to the different tunnel lengths. Therefore, it could be effectively used with an adjustment according to the femoral tunnel length.
Adequate initial strong fixation is essential for treatment success after anterior cruciate ligament (ACL) reconstruction. It provides stability to the graft until biological integration to the native bone.1) All graft fixation techniques have demonstrated positive clinical outcomes; however, a consensus has not been reached on the optimal fixation technique.2)
With the advances in independent drilling techniques for femoral tunnel placement, such as the medial portal and outside-in techniques, cortical suspensory fixation devices have gained popularity for soft tissue graft fixation. 3456) The RetroButton (Arthrex Inc., Naples, FL, USA) is a cortical suspensory fixation device that has a fixed-length loop. It has demonstrated satisfactory biomechanical properties and high failure loads for soft tissue graft fixation.178) However, this device is technically demanding to use and does not allow complete graft fill in the femoral tunnel socket. In addition, a measurement error could result in insufficient graft length.
Adjustable-length fixation devices were designed to allow adaptation of a graft to the different tunnel lengths without leaving excess space inside the tunnel. The TightRope RT (Arthrex Inc.) is an adjustable-length loop suspensory fixation device that is usually used with FlipCutter (Arthrex Inc.). This combination allows proper grafttunnel fit.79) Compared with femoral fixation with use of a fixed-loop device, fixation with use of an adjustable-loop device showed similar clinical outcomes.10) However, some biomechanical studies have expressed concern that adjustable-length loop devices could result in loop lengthening and subsequent graft slippage compared to the fixed-length loop devices.81112) Under such circumstances, resultant excessive graft-tunnel motion at the tendon-bone interface might impair healing and integration of the graft, eventually resulting in knee instability and clinical failure.1)
However, in vitro study findings based on laxity measurements of specimens or isolated mechanical strength measures need to be corroborated with in vivo findings;1213) the relevance of in vitro findings to in vivo results has yet to be determined. The purpose of this study was to compare graft healing in the femoral tunnel, implant-related failure, and clinical results between fixed- and adjustable-length loop devices in outside-in ACL reconstruction. The hypothesis of this study was that there would be no differences between the two kinds of devices in terms of the graft healing in the femoral tunnel, implant-related failure, and clinical results.
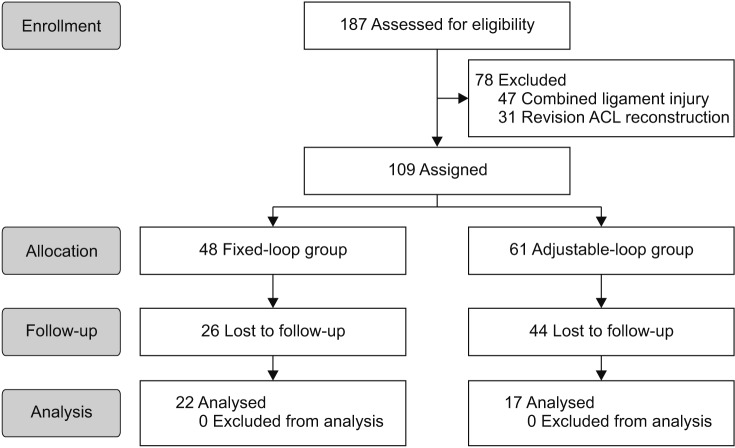
A total of 109 participants who underwent ACL reconstruction using the retrograde outside-in technique with femoral cortical suspensory fixation devices were recruited for this study from December 2010 to July 2014. The included patients (1) had an ACL injury with no other associated ligamentous injury of the involved knee; (2) underwent primary single-bundle ACL reconstruction using quadruple auto-hamstring tendon grafts, and (3) were available for postoperative magnetic resonance imaging (MRI) at 6 months after surgery. Patients with combined ligament injury and revision reconstruction were excluded. The included patients were divided into two groups according to the femoral cortical suspensory fixation device. The fixed-loop group (48 patients) received a fixed-length loop device using RetroButton (Arthrex Inc.) and the adjustable-loop group (61 patients) received an adjustable-length loop device using TightRope RT (Arthrex Inc.). The preoperative demographic data of the two groups were similar (Table 1). Patients who were available for the last follow-up at more than 2 years after surgery were 22 (45.8%) in the fixed-loop group and 17 (27.9%) in the adjustable-loop group (Table 1). The primary reason for exclusion from the final assessment was loss of follow-up (Fig. 1) of patients who became asymptomatic and felt no need to return to see the surgeon or those who lived relatively far from the hospital. Assignment of patients to either the fixed-loop or the adjustable-loop group was not done by standard randomization but by the time the procedure was performed since the senior surgeon (JHA) changed the fixation device beginning July 2012. The surgery was performed using the fixed-length loop device from December 2010 to June 2012 and using the adjustable-length loop device from July 2012 to July 2014. The study was approved by the Institutional Review Board of Kangbuk Samsung Medical Center (IRB No. 2016-05-049). Informed consent was obtained from all the patient in the article.
With the knee joint distended using an infusion pump, arthroscopic examination was performed through the anterolateral and anteromedial portals. For creation of the tibial tunnel, a guide pin was inserted from the proximal-medial tibial condyle to the center of the ACL tibial insertion using an ACL tibial drill guide (Linvatec, Largo, FL, USA) with a 50°. A cannulated reamer was used to match the diameter of the graft. The ACL tibial drilling guide or Acufex ACL femoral guide (Smith & Nephew, Andover, MA, USA) was introduced through the anterolateral portal. The femoral tunnel was usually adjusted to 7 to 9 mm according to the graft diameter. The guide tip was located at a point which is 4 to 5 mm anterior-distal from the posterior-proximal margin of the ACL femoral footprint. The femoral tunnel was placed within the inner margin of the cartilage and reamed with FlipCutter (Arthrex Inc.). After performing retro-reaming to a depth of 30 mm on the femoral tunnel, the FlipCutter was removed and the ACL graft was passed through the tunnel.5)
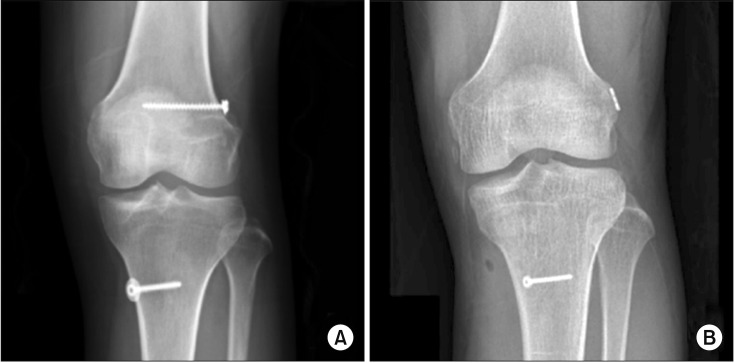
The RetroButton was used for femoral fixation. The graft sutures and button passed through the femoral lateral cortex, 3 cm proximal to the lateral epicondyle. Tension was applied to allow complete graft fill of the femoral tunnel. After the button was removed, the loop was fixed using a 4.5-mm cortical screw with washer to the lateral femoral cortex (Fig. 2).
The TightRope RT (Arthrex Inc.) device was used for femoral fixation. The passing suture and tensioning sutures were passed through the tibia and out of the femur. The button was pulled through the femur to exit the lateral cortex, and the graft was moved forward by tension on the TightRope with the strands shortened. The free suture ends were secured with three half-hitch suture knots tied with an arthroscopic knot pusher (Fig. 2). Then, the tibial side of graft was secured with a bioabsorbable interference screw and post-tied using a 4.5-mm cortical screw.
MRI was performed on a 3.0-T unit Magnetom (Siemens, Munich, Germany) using a standardized protocol for the knee in the neutral position. The grafts were evaluated by MRI 6 to 7 months postoperatively. Coronal T2-weighted fast spin echo images were examined as follows. First, to determine the presence of synovial fluid at the exit of femoral tunnel between the end of the graft and the exit of the femoral bone tunnel, T2 potentiated sequences, most helpful for detection of fluid-sensitive sequence, were used. If an area of higher signal intensity was observed between the graft and the bone tunnel, it was classified as positive for the presence of synovial fluid (Fig. 3).
Then, to analyze graft healing and tendon-bone healing in the femoral tunnel, signal intensity was calculated to measure signal-to-noise ratios (SNRs). The signal intensity was calculated at three zones in the femoral tunnel (superior tendon-bone interface, tendon graft, and inferior tendon-bone interface) and the background (approximately 1 cm medial to the joint line) using a 3.3-mm diameter region of interest (Fig. 4). Region of interest measurements were performed perpendicular to the long axis of the tunnel at three distinct and standardized locations along the femoral tunnels in the coronal plane. The femoral tunnel aperture was calculated 0.5 cm from the joint-tunnel interface, the femoral tunnel midsection was the midline of the longitudinal axis, and the femoral tunnel exit was calculated 0.5 cm from the termination of the tunnel (Fig. 4). As the quantification method for signal intensity, the SNRs at each graft site were estimated by dividing the signal of ACL graft by the background signal. The mean values of SNRs between superior and inferior tendon-bone interfaces were used to determine the SNR of the tendon-bone interface.14) On the graft signal-to-noise quotient value, the intraclass correlation coefficient index for the intraobserver reliability showed satisfactory results.14) All of the measurements were taken by the same investigator (TSK), and repeated measurements were made on two separate days with an interval of at least 1 week.
Clinical evaluation was performed before surgery and ≥ 2 years after surgery using subjective functional examinations (International Knee Documentation Committee [IKDC] score and Tegner-Lysholm Knee Scoring [TLKS] scale) and two knee instability tests (pivot shift test and Lachman test). The subjective functional scores and the results of the instability tests were evaluated at the last follow-up. Both groups were divided into subgroups according to whether the last follow-up clinical assessment was performed.
We hypothesized that the signal intensity at tendon-bone interface of the adjustable-loop group was noninferior to that of the fixed-loop group. On MRI analysis, graft signal was compared between the quadriceps tendon with bone block and hamstring tendon autografts.15) The average SNRs at the middle lesion of the ACL graft was 2.0 ± 0.5 in quadriceps tendon with bone block and 2.4 ± 0.5 in hamstring tendon.16) There was a 20% difference in the SNR values between the two groups. A sample size of 96 patients (48 patients in each group) was determined needed based on the hypothesis that there would be an 18% difference in SNR value at the exit of the femoral tunnel between groups, with a type I (α) error of 0.05 and a type II (β) error of 0.02 (80% power). Fisher exact test was used to compare the fixed-loop group and the adjustable-loop group for categorical variables (sex and the presence/absence of synovial fluid). A two-sample t-test was used to compare the continuous variables (age, follow-up time, SNR value, subjective IKDC score and TLKS scale) between the two groups. Fisher exact test was performed to compare the objective IKDC score, Lachman test, and pivot shift test between groups. Chi-square test was performed to compare the follow-up data obtained at ≥ 2 years after surgery. The Wilcoxon signed-rank test was used to compare pre- and postoperative results of each group. The level of statistical significance was set as p < 0.05.
On comparison of mean SNR values in the femoral bone tunnel, there were no statistically significant difference in graft signal intensity between all patients and patients available at the last follow-up (Table 2). There was a small number of patients in each subgroup, but these subgroups were representative of both groups. There was no significant difference between the fixed-loop group and the adjustable-loop group in SNR values of the tendon grafts (Table 3). SNR values of the tendon-bone interface in the fixed-loop group were consistently lower than those in the adjustable-loop group at the three sites; however, there was no significant difference between the two groups (Table 3). The presence of synovial fluid at the exit of femoral bone tunnel was evident in six patients in each group, which corresponded to 12.5% in the fixed-loop group and 9.8% in the adjustable-loop group, showing no significant differences between groups (p = 0.762). In addition, two patients in the adjustable-loop group had a wide gap between the graft end and the exit of the femoral bone tunnel and one patient in the adjustable-loop group and the fixedloop group each showed a little gap (Fig. 5). A wide gap was defined as a length of more than half the diameter of the graft between the graft end and the exit of the femoral bone.
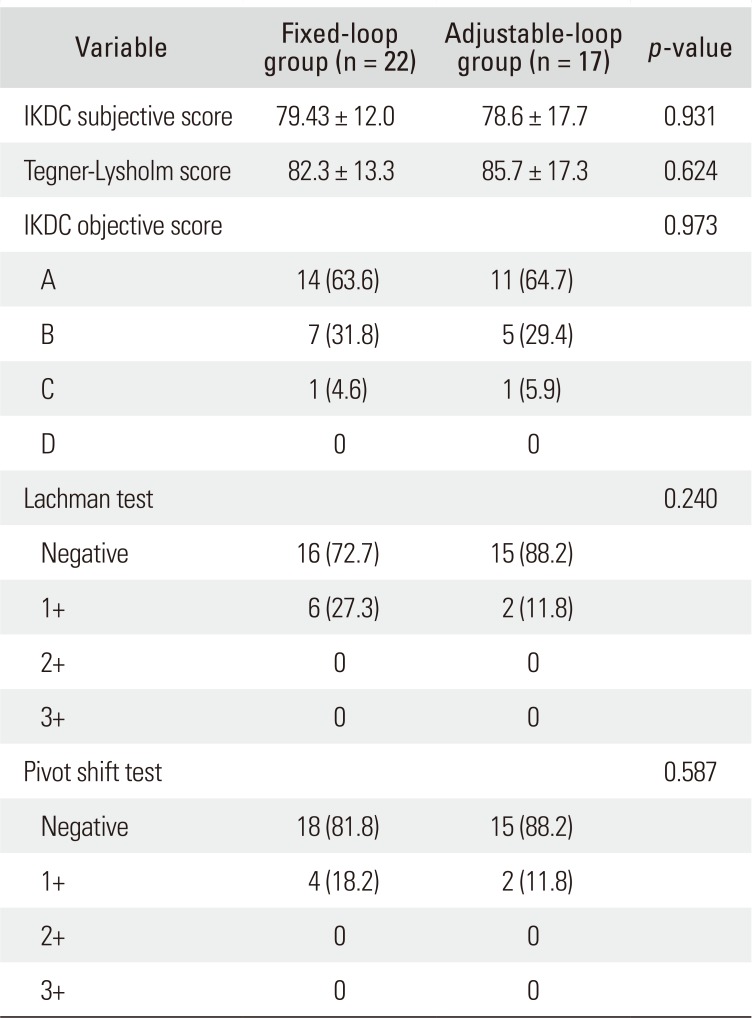
Clinical evaluation scores and physical examination findings at least 2 years after the operation were compared with preoperative findings. There was no statistically significant difference in demographics and preoperative clinical characteristics between the two groups, except for preoperative the objective IKDC score. Significant improvement was observed in patients in the fixed-loop group compared to those in the adjustable-loop group in the IKDC subjective score (p < 0.001 and p < 0.001, respectively), Tegner-Lysholm score (p < 0.001 and p = 0.002, respectively), IKDC objective score (p < 0.001 and p < 0.001, respectively), Lachman test (p < 0.001 and p < 0.001, respectively), and pivot shift test (p < 0.001 and p < 0.001, respectively). There was no significant difference in the last follow-up clinical score and knee instability test between the two groups (Table 4). There were no complications or adverse events in either group.
The important finding of this study is that the SNR values indicated the adjustable-length loop cortical suspensory fixation device had no inferior graft healing effect in the femoral bone tunnel compared to the fixed-length loop device. In addition, synovial fluid at the exit of femoral tunnel and postoperative clinical results revealed no significant difference between two devices. These findings indicate that the adjustable-length loop does not loosen after ACL reconstruction. This study provides valuable quantitative information regarding the graft healing capacity and loop lengthening of both femoral cortical suspensory devices.
Femoral cortical suspensory fixation devices are currently an accepted standard fixation device for multistranded hamstring tendon grafts in ACL reconstructions. A number of in vitro studies have compared the biomechanical properties between fixed-length loop and adjustable-length loop devices. The studies found that all fixation devices had the necessary biomechanical effects to prevent a failure and displacement and to support loads in early rehabilitation.78) However, recent studies have expressed concern about adjustable-length loop cortical suspensory devices regarding loop lengthening and the potential for failure.81213) In the present study, shortening strands of the femoral cortical suspensory devices were secured with three half-hitch suture knots tied with an arthroscopic knot pusher to reduce loop lengthening. A potential disadvantage of fixed-length loop devices is that it does not allow for complete graft fill of the femoral tunnel socket due to a mismatch between the loop and tunnel length that can result in insufficient graft length. Some authors also expressed concern regarding the bungee-cord (longitudinal graft-tunnel motion) effect and windshield-wiper (sagittal graft-tunnel motion) effect in the bone tunnel.17) In the present study, the loop was fixed using a 4.5-mm cortical screw with washer to the lateral femoral cortex after the button was removed.
This technique could draw in the maximum amount of graft relative to the depth of the femoral tunnel. In a study of Miyata et al.,18) femoral suspensory fixation with screw post showed excellent functional outcomes and biomechanical properties. However, there were disadvantages such as rapid relaxation or low stiffness of the graft, which could cause loop slippage during early postoperative rehabilitation period.
In this study, 3.0-T MRI was used to investigate graft healing and synovial fluid presence between the two groups approximately 6 months after ACL reconstruction. In a number of animal studies, 12 weeks were necessary for tendon to bone healing in the bone tunnel.1619) On quantitative MRI evaluation, Terauchi et al.14) reported the signal intensity within the femoral tunnels decreased with time at 3 and 6 months after single-bundle ACL reconstruction using autogenous hamstring tendons. Another study showed the active tendon graft remodeling occurred from 3 months after surgery and the remodeling process continued after 7 months.20) During the time before incorporation, the graft is dependent on femoral fixation devices to maintain normal ACL graft tension. Therefore, if ACL grafts are not rigidly secured during the initial healing period, migration of the graft during early rehabilitation may occur and lead to persistent laxity, instability, and functional failure. Regarding the tendon graft and tendon-bone interface signal intensity in the femoral tunnel, the SNR values of the tendon grafts were similar in both groups. These findings indicate that the adjustablelength loop devices may have no inferior graft healing effect in the femoral bone tunnel compared to the fixed-length loop devices.
An important new finding was the presence of synovial fluid at the exit of the femoral tunnel. There was more synovial fluid present in the fixed-loop group although there was no significant difference between two groups. It appears that the implant-related failure in the bone tunnel may not only be the problem of the adjustable-length loop devices. There must have been more synovial fluid in the adjustable-loop group in a biomechanical study that showed adjustable-length loop devices experienced more lengthening than the fixed-length loop devices.13) In contrast, our results indicate that fixed-loop cortical suspensory devices may also be susceptible to lengthening. We cannot explain the reason for the higher number of positive cases in the fixed-length loop group considering the presence of synovial fluid. We surmise that technical mistakes, such as incomplete femoral tunnel filling, may have been responsible for loop lengthening. For example, there were two cases with a large gap at the graft end in the femoral bone tunnel that seemed to have resulted from an obvious technical mistake: when the button was pulled through the femur, insufficient tension may have been applied.
There was no significant difference in clinical scores and physical examination results for at least 2 years after the operation between the two femoral cortical suspension fixation devices. These clinical results are supported by several studies that showed no clinical differences among the femoral fixation devices. Some studies reported no significant difference in anteroposterior stability and clinical scores among femoral fixation devices, such as cortical suspensory fixation, aperture interference screws, and trans-femoral fixation devices.2122) Boyle et al.23) recently reported their clinical results comparing fixed- and adjustable-length loop devices; no differences in postoperative laxity or graft failure rates were evident at the 2-year follow-up. During early postoperative rehabilitation period, graft relaxation and graft slippage could occur by lengthening of the fixation device.1) It negatively affects functional outcomes and graft healing as the graft becomes lax.124) Although some synovial fluid was evident in several cases, clinical results at the 2-year follow-up showed significant improvement in both groups.
By the laboratory-based studies of ACL reconstruction, any associated findings in biomechanical studies were validated.11) In our MRI evaluations and clinical assessments, the difference in displacement between fixedand adjustable-length loop devices observed in previous laboratory studies either did not occur in vivo or was clinically insignificant.91213) Therefore, it was our interest to determine whether there is any difference in graft healing in the femoral tunnel, implant-related failure, and clinical results between fixed- and adjustable-length loop devices after ACL reconstruction. This study provides valuable quantitative information regarding graft healing in the femoral tunnel, implant-related failure, and clinical results of both femoral cortical suspensory fixation devices.
This study has some limitations. The main limitation was the lack of direct comparison of the strength of the button plate in both devices because we removed the button plate of the fixed-loop device. Prior biomechanical results of various femoral cortical suspensory fixation devices indicated no significant difference in ultimate failure strength with respect to the button plate. Since we presumed that synovial fluid between the graft and the bone tunnel may interfere with graft healing, we chose to focus our analysis on reducing the gap at exit of bone tunnel. Another limitation of this study is that two patients in the adjustable-loop group had a wide gap between the graft end and the exit of the femoral bone tunnel and we did not measure the gap accurately; however, we believed this would enable the best comparison of graft healing in the femoral tunnel between two femoral cortical suspensory devices. Third, the length of MRI follow-up was relatively short to analyze graft healing in the bone tunnel. Previous studies have demonstrated that graft incorporation occurs in the early 8- to 12-week postoperative period925) with tissue healing response occrring within the bone tunnel in the 6 months postoperative period.26) Based on such studies, 6-month postoeprative MRI may have been too early to determine graft healing. Fourth, the study did not use objective parameters, such as arthrometer testing, using only subjective tests on instability. Lastly, this was a retrospective study with a low final follow-up rate. In spite of such limitations, the significance of this study is that we found the adjustable-length loop device showed comparable graft healing, implant-related failure, and clinical results. Therefore, we believe it could be effectively used with an adjustment to the femoral tunnel length in ACL reconstruction.
References
1. Kousa P, Jarvinen TL, Vihavainen M, Kannus P, Jarvinen M. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part II: tibial site. Am J Sports Med. 2003; 31(2):182–188. PMID: 12642250.

2. Brown CH Jr, Wilson DR, Hecker AT, Ferragamo M. Graft-bone motion and tensile properties of hamstring and patellar tendon anterior cruciate ligament femoral graft fixation under cyclic loading. Arthroscopy. 2004; 20(9):922–935. PMID: 15525925.

3. Lee YS, Ko TS, Ahn JH, et al. Comparison of tibial tunnel techniques in posterior cruciate ligament reconstruction: C-arm versus anatomic fovea landmark. Arthroscopy. 2016; 32(3):487–492. PMID: 26597550.

4. Lee YS, Lee BK, Oh WS, Cho YK. Comparison of femoral tunnel widening between outside-in and trans-tibial double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014; 22(9):2033–2039. PMID: 23851922.

5. Ahn JH, Lee YS, Lee SH. Creation of an anatomic femoral tunnel with minimal damage to the remnant bundle in remnant-preserving anterior cruciate ligament reconstruction using an outside-in technique. Arthrosc Tech. 2014; 3(1):e175–e179. PMID: 24749041.

6. Lee YS, Lee BK, Chun DI. Flipping method of a RetroButton during ACL reconstruction with outside-in femoral drilling using a FlipCutter. Orthopedics. 2012; 35(10):861–864. PMID: 23027473.

7. Kamelger FS, Onder U, Schmoelz W, Tecklenburg K, Arora R, Fink C. Suspensory fixation of grafts in anterior cruciate ligament reconstruction: a biomechanical comparison of 3 implants. Arthroscopy. 2009; 25(7):767–776. PMID: 19560641.

8. Petre BM, Smith SD, Jansson KS, et al. Femoral cortical suspension devices for soft tissue anterior cruciate ligament reconstruction: a comparative biomechanical study. Am J Sports Med. 2013; 41(2):416–422. PMID: 23263298.
9. Conner CS, Perez BA, Morris RP, Buckner JW, Buford WL Jr, Ivey FM. Three femoral fixation devices for anterior cruciate ligament reconstruction: comparison of fixation on the lateral cortex versus the anterior cortex. Arthroscopy. 2010; 26(6):796–807. PMID: 20511038.

10. Choi NH, Yang BS, Victoroff BN. Clinical and radiological outcomes after hamstring anterior cruciate ligament reconstructions: comparison between fixed-loop and adjustable-loop cortical suspension devices. Am J Sports Med. 2017; 45(4):826–831. PMID: 27881383.

11. DeBerardino TM, Smith PA, Cook JL. Femoral suspension devices for anterior cruciate ligament reconstruction: letter to the editor. Am J Sports Med. 2014; 42(2):NP15–NP16. PMID: 24489006.

12. Eguchi A, Ochi M, Adachi N, Deie M, Nakamae A, Usman MA. Mechanical properties of suspensory fixation devices for anterior cruciate ligament reconstruction: comparison of the fixed-length loop device versus the adjustable-length loop device. Knee. 2014; 21(3):743–748. PMID: 24613584.

13. Barrow AE, Pilia M, Guda T, Kadrmas WR, Burns TC. Femoral suspension devices for anterior cruciate ligament reconstruction: do adjustable loops lengthen? Am J Sports Med. 2014; 42(2):343–349. PMID: 24158183.
14. Terauchi R, Arai Y, Hara K, et al. Magnetic resonance angiography evaluation of the bone tunnel and graft following ACL reconstruction with a hamstring tendon autograft. Knee Surg Sports Traumatol Arthrosc. 2016; 24(1):169–175. PMID: 25288337.

15. Ma Y, Murawski CD, Rahnemai-Azar AA, Maldjian C, Lynch AD, Fu FH. Graft maturity of the reconstructed anterior cruciate ligament 6 months postoperatively: a magnetic resonance imaging evaluation of quadriceps tendon with bone block and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2015; 23(3):661–668. PMID: 25223969.
16. Hunt P, Rehm O, Weiler A. Soft tissue graft interference fit fixation: observations on graft insertion site healing and tunnel remodeling 2 years after ACL reconstruction in sheep. Knee Surg Sports Traumatol Arthrosc. 2006; 14(12):1245–1251. PMID: 16710731.
17. Rork PE. “Bungee cord” effect in hamstring tendon ACL reconstruction. Orthopedics. 2000; 23(3):184. PMID: 10741360.

18. Miyata K, Yasuda K, Kondo E, Nakano H, Kimura S, Hara N. Biomechanical comparisons of anterior cruciate ligament: reconstruction procedures with flexor tendon graft. J Orthop Sci. 2000; 5(6):585–592. PMID: 11180923.
19. Chen CH. Graft healing in anterior cruciate ligament reconstruction. Sports Med Arthrosc Rehabil Ther Technol. 2009; 1(1):21. PMID: 19772670.

20. Kanamura H, Arai Y, Hara K, et al. Quantitative evaluation of revascularization at bone tunnels and grafts with contrast-enhanced magnetic resonance angiography after anterior cruciate ligament reconstruction. Int Orthop. 2016; 40(7):1531–1536. PMID: 26744163.

21. Aydin D, Ozcan M. Evaluation and comparison of clinical results of femoral fixation devices in arthroscopic anterior cruciate ligament reconstruction. Knee. 2016; 23(2):227–232. PMID: 25937093.

22. Lubowitz JH, Schwartzberg R, Smith P. Cortical suspensory button versus aperture interference screw fixation for knee anterior cruciate ligament soft-tissue allograft: a prospective, randomized controlled trial. Arthroscopy. 2015; 31(9):1733–1739. PMID: 25911394.
23. Boyle MJ, Vovos TJ, Walker CG, Stabile KJ, Roth JM, Garrett WE Jr. Does adjustable-loop femoral cortical suspension loosen after anterior cruciate ligament reconstruction? A retrospective comparative study? Knee. 2015; 22(4):304–308. PMID: 25999126.

24. Rodeo SA, Kawamura S, Kim HJ, Dynybil C, Ying L. Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: an effect of graft-tunnel motion? Am J Sports Med. 2006; 34(11):1790–1800. PMID: 16861579.
25. Kawakami H, Shino K, Hamada M, et al. Graft healing in a bone tunnel: bone-attached graft with screw fixation versus bone-free graft with extra-articular suture fixation. Knee Surg Sports Traumatol Arthrosc. 2004; 12(5):384–390. PMID: 15042286.

26. Rodeo SA, Arnoczky SP, Torzilli PA, Hidaka C, Warren RF. Tendon-healing in a bone tunnel: a biomechanical and histological study in the dog. J Bone Joint Surg Am. 1993; 75(12):1795–1803. PMID: 8258550.

Fig. 3
Coronal oblique T2-weighted magnetic resonance imaging. (A) Presence of synovial fluid case. (B) Absence of fluid case. Arrow: presence of synovial fluid at the exit of femoral tunnel.

Fig. 4
Signal intensity of anterior cruciate ligament graft using the signal-to-noise quotient. (A) Tunnel aperture. (B) Tunnel midsection. (C) Tunnel exit. Arrow: tendon-bone interface, arrowhead: tendon graft.
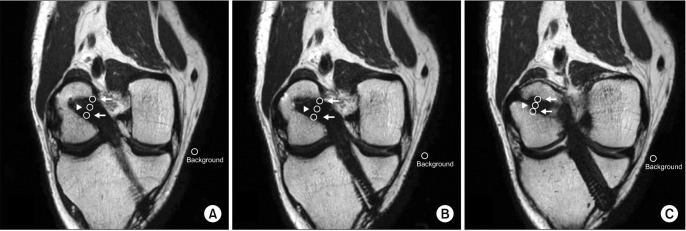
Fig. 5
A wide gap between the graft end and the exit of the femoral bone tunnel. Arrow: length of wide gap.

Table 1
Demographic and Clinical Characteristics of the Patients
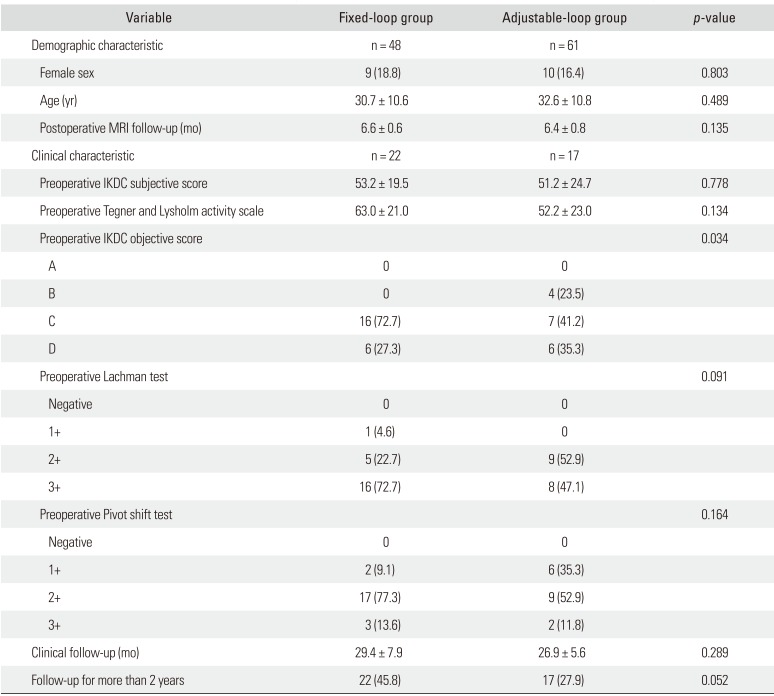
Table 2
Comparison of Mean SNR Values in the Femoral Bone Tunnel between Total Patients and Patients Available for Last Clinical Follow-up in Each Group
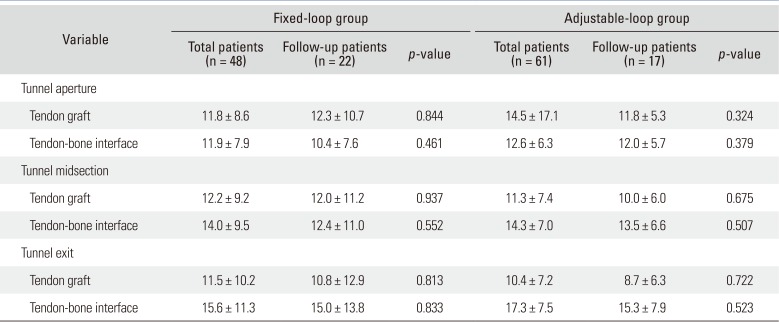
Table 3
Comparison of Mean SNR Values in the Femoral Bone Tunnel between the Fixed-Loop Group and the Adjustable-Loop Group
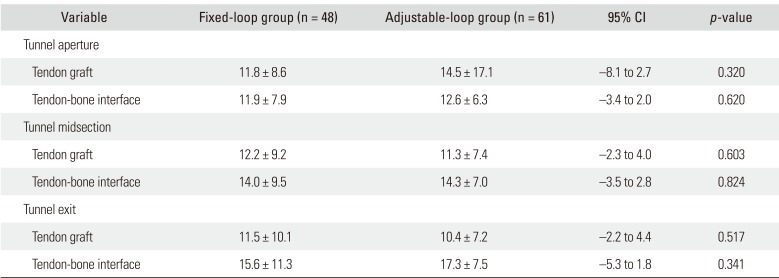
Table 4
Clinical Results at Last Follow-up between the Fixed-Loop Group and the Adjustable-Loop Group




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download