Abstract
Background
Although distal radius fractures (DRF) are common fractures, intra-articular comminuted DRF with volar free fragments are uncommon. There is considerable difficulty in the fixation of free fragments beyond the watershed line using the existing volar locking plate. We aimed to examine the efficacy and potential complications associated with the use of juxta-articular volar plates in intra-articular DRF accompanied by free fragments beyond the watershed line.
Methods
The patients were enrolled in a consecutive manner between 2007 and 2016. In cases of DRF with free fragments beyond the watershed line, we employed a 2.4-mm small fragment juxta-articular volar locking compression plate using a volar Henry approach. A total of 32 patients were included in this study. There were 15 males and 17 females with a mean age of 52.3 years (range, 33 to 69 years). The mean follow-up period was 14.5 months (range, 10 to 24 months). Preoperative radiographs and three-dimensional computed tomography images were used to analyze fracture patterns and assess the free fragments beyond the watershed line. The mean number of free fracture fragments beyond the watershed line was 2.33. Plain radiographs of immediate postoperative and last follow-up were used to confirm fracture union, incongruence, radial height, volar tilt, radial inclination, and arthritic changes. For functional assessment, we measured grip strength, range of motion (ROM), modified Mayo wrist score (MMWS) and determined Disabilities of Arm, Shoulder and Hand (DASH) scores at the last follow-up. Postoperative complications were monitored during the follow-up period.
Results
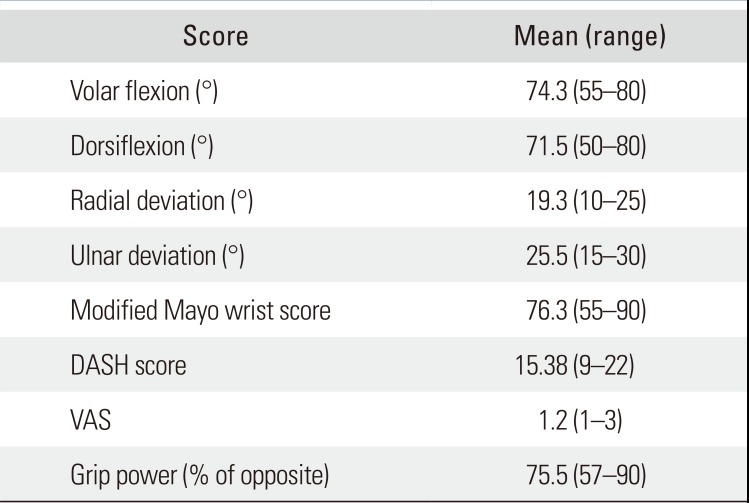
All patients obtained sound union without significant complications. At the last follow-up, 16 cases presented with an articular step-off of more than 1 mm (mean, 1.10 mm). The mean MMWS was 76.3 (range, 55 to 90), mean DASH score was 15.38 (range, 9 to 22), mean visual analogue scale score for pain was 1.2 and mean grip strength was 75.5% of the opposite side. The mean ROM was 74.3° for volar flexion and 71.5° for dorsiflexion.
Distal radius fractures (DRF) are common fractures that represent 17% of all fractures in adults.1) DRF accompanied by a dorsal or volar rim fracture are uncommon, with the incidence ranging from 1% to 11% of all kinds of DRF.2) In particular, DRF with accompanying volar free fracture fragments beyond the watershed line present less common incidences and are more challenging to achieve fixation with the conventional volar locking plate. This kind of fracture has characteristics of articular fractures where volar translation of fragments and even subluxation of the carpus may occur unless properly stabilized. Until now, there has been no consensus on the definition, injury mechanism, and gold standard for the treatment of this type of fracture.34567) Percutaneous pin fixation is the only method used in simple articular fractures despite there was an attempt to correct articular step-off with following K-wire fixation.8) External fixation can restore the radius length but does not adequately correct displaced or impacted fragments.910)
Robert Medoff developed a simplified articular fracture classification of five components and devised a hybrid technique using percutaneous wire and plate fixation designed to fix individual fracture fragment through several small incisions, so called fragment-specific fixation technique.1011) As an alternative to volar wire fixation, a volar hook plate was introduced by Bakker and Shin12) to rigidly fix the volar marginal rim fragments as in fragment-specific fixation. Regardless of the specific fixation method, the basic principles of surgical treatment are anatomic reduction and secure fixation with use of a low-profile device that does not disrupt the normal anatomy.
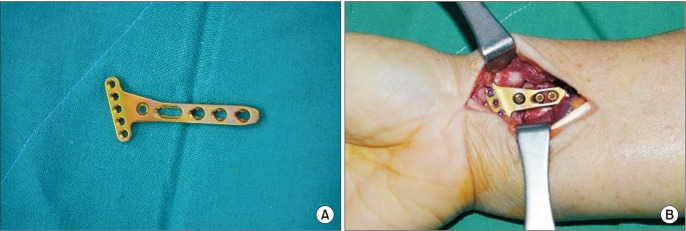
Here, we report a series of cases in which we performed open reduction and internal fixation for this type of fracture in active, healthy patients, using a 2.4-mm juxta-articular volar locking compression plate (LCP) Distal Radius System (DePuy Synthes, Solothurn, Switzerland). This plate of particular design can be placed more distally and allows for direct fixation of far distal volar fragments. We aimed to examine the efficacy and potential complications associated with the use of this particular plate in intra-articular DRF accompanied by volar free fragments beyond the watershed line.
This retrospective study was carried out between 2007 and 2016 under approval of Institutional Review Board of CHA Medical Center (IRB No. CHAMC 2017-04-040). Written informed consents were obtained from all patients. In cases of DRF with volar free fragments beyond the watershed line, we employed a 2.4-mm small fragment juxta-articular volar LCP instead of the conventional volar locking plate (Fig. 1). Patients were enrolled consecutively during the study period. Due to compromised medical condition, low demand for functional recovery, and refusal of operative treatment, conservative management was the treatment of choice in some patients with displaced intraarticular fragments. In total, 43 patients with comminuted intra-articular DRF with volar free fragments beyond the watershed line were recruited from a single university hospital for surgical treatment using the juxta-articular volar plate. All surgical procedures were performed by a single experienced hand surgeon (SHH).
After excluding patients with any form of ipsilateral arm fracture or a history of hand and wrist fractures, 32 patients were ultimately included in this study. There were 15 males and 17 females, with a mean age of 52.3 years (range, 33 to 69 years). Medical charts of each patient were reviewed to investigate patient characteristics, medical history and history of smoking. The mean time from injury to surgery was 3.6 days (range, 0 to 10 days), and the mean follow-up period was 14.5 months (range, 10 to 24 months) (Table 1).
Open reduction was performed using the volar Henry approach. With exposure of the distal radius, a Freer elevator was inserted through the volar fractured site and was positioned under the subchondral bone of the radiocarpal joint. The joint surface was elevated and restored using the leverage technique. Adequate reduction was confirmed with C-arm guidance, which was followed by preliminary K-wire fixation. With the plate appropriately positioned, a cortical screw was inserted into the elongated proximal combi-hole in order to tightly attach the plate over the distal radius metaphysis. The remaining proximal locking holes were inserted with locking screws. Finally, 2.4-mm locking screws were inserted into the distal locking holes of the plate (Fig. 2). Penetration of the distal screws into the distal radiocarpal joint was assessed with fluoroscopy on a 10° to 20° radial-tilted view and passive joint motion of the compressed radiocarpal joint was examined. The wrist was immobilized with a short-arm splint. Patients were allowed to start gradual and gentle wrist motion from postoperative week 2.
Preoperative radiographs and three-dimensional computed tomography (CT) images were used to analyze fracture patterns and assess the volar free fragments beyond the watershed line. The mean number of volar free fracture fragments beyond the watershed line was 2.33 (range, 1 to 4). The amount of displacement of the fragment was measured using a millimeter ruler on anteroposterior and lateral-magnified radiographs taken immediately after surgery. At the last follow-up, plain radiographs were used to confirm fracture union, incongruence, radial height, volar tilt, radial inclination and arthritic changes. Radiological measurements were performed independently by two orthopedic surgeons (YSS and THK) and one radiologist (HJ).
Functional assessment was performed at the last follow-up with regard to grip strength, range of motion (ROM) in the wrist, modified Mayo wrist score (MMWS) and Disabilities of Arm, Shoulder and Hand (DASH) score. Grip strength was measured using a Jamar dynamometer (Hydraulic Hand Dynamometer, 5030J1; Jamar, USA) and compared with the contralateral side. ROM in the wrist and forearm (dorsiflexion, volar flexion, radial deviation, and ulnar deviation) were measured using a goniometer. Pain visual analogue scale (VAS) score was also assessed.
We monitored possible complications after DRF including wound infection, nonunion, malunion, tendon rupture, traumatic osteoarthritis, ROM limitation, persistent neuropathy and even complex regional pain syndrome during the follow-up period. Given the particular DRF pattern and the use of a juxta-articular plate, we especially tried to detect the occurrence of plate-induced tendon rupture, joint perforation of inserted screw, and posttraumatic arthritis until the final follow-up.
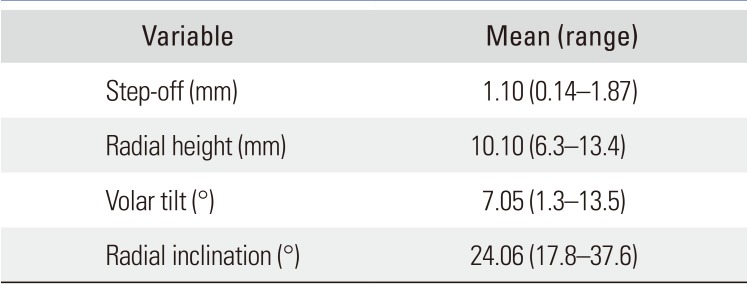
Postoperatively, authors did not encounter wound problem and all patients achieved bony union during the outpatient follow-up. There was no case of persistent neuropathy or fixation failure inducing fragment migration. At the last follow-up, 16 cases presented with an articular step-off of more than 1 mm (mean, 1.10 mm). The mean radial height was 10.1 mm (range, 6.3 to 13.4 mm), mean volar tilt was 7.05° (range, 1.3° to 13.5°), and mean radial inclination was 24.06° (range, 17.8° to 37.6°). There was no evidence of posttraumatic arthritis on follow-up radiographs despite the mean 1.10 mm of articular step-off (Table 2). The intraclass correlation coefficient ranged from 0.916 to 0.988 for each item and was statistically significant (Table 3).
At the last follow-up, the mean MMWS was 76.3 (range, 55 to 90; excellent in 1, good in 13, fair in 17, and poor in 1), mean DASH score was 15.38 (range, 9 to 22), mean pain VAS score was 1.2, and mean grip strength was 75.5% of the opposite side. The mean ROM was 74.3° for volar flexion, 71.5° for dorsiflexion, 19.3° for radial deviation, and 25.5° for ulnar deviation (Table 4 and Fig. 3).
There was no case of tendon rupture (extensor or flexor tendon) until the final follow-up. However, we carried out plate removal in 11 of the 32 patients due to the patient's request.
The distal radius articular surface is composed of the lunate facet and the scaphoid facet that face carpal bones of the lunate and scaphoid, respectively.10) Anterior aspect of the articular facet, the name of the anterior rim or volar facet, is the keystone of radiocarpal joints affecting stability of anterior carpal translation. However, the scaphoid and lunate facets have different features and the anatomic differences make it difficult to achieve anatomic reduction and rigid fixation. Although the anterior rim of the lunate and scaphoid facets project anterior to the relatively flat surface of the distal radius volar aspect, the lunate facet is more prominent and creates a setup for a triangular fragment. In our patients, the fracture line started from distal to the watershed line and extended through the joint surface making a free fragment. Some patients had a coronal split fracture featuring a volar rim free fragment and others had a more horizontal fracture line even extending into the dorsal articular rim. Moreover, there were cases of free fragments derived from the scaphoid facet only or even from both scaphoid and lunate facet as well as only lunate facet involvement.
Even though volar locking plate fixation has become a well-established technique for DRF management, conventional volar locking plates are designed to be positioned proximal to the watershed line.1314) Therefore, there is considerable difficulty in the fixation of intra-articular fragments, especially free fragments beyond the watershed line. Harness et al.15) reported a series of loss of fixation of the lunate facet leading to volar carpal subluxation after standard volar plating in volar shear fractures. Earp et al.16) analyzed the surgical results of 77 AO/OTA C3 type fractures using a volar locking plate and reported reduction loss in 10.4% of patients. In order to overcome this difficulty, there have been several trials using additional fixation screws, wire loop techniques,17) a hook plate,12) and a specialized plate for those fracture.67)
More recently, a 2.4-mm LCP plate has been developed, which features a low-profile plate and a proximal angle of 5° relative to the distal locking screws. This plate was designed to be placed over the watershed line and treat small-sized articular fragments. Considering the anatomy of the distal radius, the distal radius volar concave surface, in which the implant is placed, exhibits a limited transverse ridge, commonly referred to as the watershed line. Implants placed over, or projecting above, the watershed line can potentially irritate and even lead to a rupture of the flexor tendons.18) In 11 of the 32 patients treated in the present study, the inserted implants needed to be removed due to the patient's request although there were no other reported problems. Furthermore, we did not encounter any cases involving a rupture of the flexor tendon.
A fracture fragment beyond the watershed line itself is an intra-articular fracture, and the majority of our cases had other intra-articular fragments other than the volar marginal fragments which numbered 2.33 on average. In cases of DRF, more than 2-mm articular step-off should not be neglected and should be considered as an indication of operative management in an active, healthy patient.19) Radiocarpal articular incongruity remains the most clinically significant radiographic parameter in younger patients with regards to both functional outcome and future degenerative change. Karnezis et al.20) reported that residual articular incongruity is correlated with persisting loss of wrist dorsiflexion and that wrist dysfunction contradicts the view that loss of articular congruity is associated with delayed development of articular degeneration but not with early wrist dysfunction.
The rafting technique has also been introduced and is commonly used for cases involving tibial plateau fractures. A locking plate is situated near the joint line and proximal fixed-angle locking screws are inserted to hold the subchondral bone of the tibial plateau.21) The raft screws inserted into the subchondral bone are known to be resistant to joint collapse.22) Since the AO juxta-articular plate is laid down over the watershed line, distal screws are inserted into the subchondral bone of the distal radius articular surface. In this setting, subchondral bone fixation can support the articular surface in a more robust manner than conventional locking plates in which distal screws are inserted through the metaphyseal cancellous bone. Furthermore, distal locking screws inserted from a position just proximal to the articular surface are able to hold volar free fracture fragments beyond the watershed line.
Another possible concern related to this type of plate is screw penetration into the joint space owing to the screws being inserted too distally. The AO juxta-articular plate has fixed-angle distal screws and is an anatomically precontoured plate; in our experience, it was rarely necessary to bend the plates along the distal radius volar surface. Rather, our experience indicated that if the plate is appropriately positioned, the distal screws do not penetrate the joint surface. Furthermore, in order to confirm whether or not screws penetrated the joint space, we used 10° to 20° radial-tilting lateral views both intra- and postoperatively. After final fixation, it is also helpful to assess the passive radiocarpal ROM, with passive compression, in order to confirm that the joint glides smoothly without mechanical crepitus.
Compared with more common osteoporotic DRF, fractures in this study occurred in younger patients (mean age, 52.3 years) with high-energy intra-articular comminution. Despite the high energy injury, it is noteworthy that there were no wound complications associated with soft tissue injury in this study. This problem was prevented with immediate open reduction and internal fixation.
Konstantinidis et al.23) used the same plate used in our present study and reported sufficient fixation to prevent clinically significant loss or articular reduction and acceptable patient outcome. However, the study included only complex articular fractures, not particular articular fractures with far volar fracture fragments. In our present study, even with a severe comminuted fracture with a volar free fragment distal to the watershed line, good results were obtained when volar fixation was performed with an appropriate plate.
This study had some limitations. Because the surgical approach was determined by the configuration of the fracture and the surgeon's preference, this study represents the experiences of a single surgeon. In addition, since we were only focusing on a particular type of DRF, in which there were volar free fragments beyond the watershed line, our patient group was relatively small and there was no comparable control group. Though postoperative ruptures have been reported as late as 10 years following surgery, the mean time to flexor tendon rupture is approximately 9 months after surgery.10) Considering the mean follow-up period was 14.5 months (range, 10 to 24 months), we might not have sufficiently evaluated tendon problems caused by the juxta-articular plate and delayed onset of traumatic osteoarthritic changes derived from articular incongruence.
In cases of intra-articular comminuted DRF with volar free fragments beyond the watershed line, a volar approach with use of a juxta-articular plate provided favorable outcomes without significant complications.
ACKNOWLEDGEMENTS
We thank Hyunkyung Jang, Department of Radiology, CHA Bundang Medical Center, CHA University School of Medicine, for the participation in radiological measurement.
References
1. Jakob M, Rikli DA, Regazzoni P. Fractures of the distal radius treated by internal fixation and early function: a prospective study of 73 consecutive patients. J Bone Joint Surg Br. 2000; 82(3):340–344. PMID: 10813166.
2. Pattee GA, Thompson GH. Anterior and posterior marginal fracture-dislocations of the distal radius: an analysis of the results of treatment. Clin Orthop Relat Res. 1988; (231):183–195.
3. Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986; 68(5):647–659. PMID: 3722221.

4. Harley BJ, Scharfenberger A, Beaupre LA, Jomha N, Weber DW. Augmented external fixation versus percutaneous pinning and casting for unstable fractures of the distal radius: a prospective randomized trial. J Hand Surg Am. 2004; 29(5):815–824. PMID: 15465230.
5. Chang HC, Poh SY, Seah SC, Chua DT, Cha BK, Low CO. Fragment-specific fracture fixation and double-column plating of unstable distal radial fractures using AO mini-fragment implants and Kirschner wires. Injury. 2007; 38(11):1259–1267. PMID: 17631882.

6. Goorens CK, Geeurickx S, Wernaers P, Staelens B, Scheerlinck T, Goubau J. Midterm follow-up of treating volar marginal rim fractures with variable angle Lcp volar rim distal radius plates. J Hand Surg Asian Pac Vol. 2017; 22(2):184–187. PMID: 28506180.

7. Kachooei AR, Tarabochia M, Jupiter JB. Distal radius volar rim fracture fixation using DePuy-Synthes volar rim plate. J Wrist Surg. 2016; 5(1):2–8. PMID: 26855829.

8. Johnson NA, Dias JJ, Wildin CJ, Cutler L, Bhowal B, Ullah AS. Comparison of distal radius fracture intra-articular step reduction with volar locking plates and K wires: a retrospective review of quality and maintenance of fracture reduction. J Hand Surg Eur Vol. 2017; 42(2):144–150. PMID: 27697898.

9. Melone CP Jr. Open treatment for displaced articular fractures of the distal radius. Clin Orthop Relat Res. 1986; (202):103–111.

10. Wolfe SW. Distal radius fractures. In : Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, Cohen MS, editors. Green's operative hand surgery. 7th ed. Philadelphia, PA: Elsevier;2017. p. 516–587.
11. Leslie BM, Medoff RJ. Fracture specific fixation of distal radius fractures. Tech Orthop. 2000; 15(4):336–352.

12. Bakker AJ, Shin AY. Fragment-specific volar hook plate for volar marginal rim fractures. Tech Hand Up Extrem Surg. 2014; 18(1):56–60. PMID: 24521761.

13. Orbay JL, Touhami A. Current concepts in volar fixed-angle fixation of unstable distal radius fractures. Clin Orthop Relat Res. 2006; 445:58–67. PMID: 16505728.

14. Orbay JL. The treatment of unstable distal radius fractures with volar fixation. Hand Surg. 2000; 5(2):103–112. PMID: 11301503.

15. Harness NG, Jupiter JB, Orbay JL, Raskin KB, Fernandez DL. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Joint Surg Am. 2004; 86(9):1900–1908. PMID: 15342751.

16. Earp BE, Foster B, Blazar PE. The use of a single volar locking plate for AO C3-type distal radius fractures. Hand (N Y). 2015; 10(4):649–653. PMID: 26568717.

17. Chin KR, Jupiter JB. Wire-loop fixation of volar displaced osteochondral fractures of the distal radius. J Hand Surg Am. 1999; 24(3):525–533. PMID: 10357531.

18. Omokawa S, Abe Y, Imatani J, Moritomo H, Suzuki D, Onishi T. Treatment of intra-articular distal radius fractures. Hand Clin. 2017; 33(3):529–543. PMID: 28673629.

19. Ruch DS, McQeen MM. Distal radius and ulna fractures. In : Court-Brown CM, Heckman JD, McQueen MM, Ricci WM, Tornetta P, McKee MD, editors. Rockwood and Green's fractures in adults. 7th ed. Philadelphia, PA: Wolters Kluwer;2010. p. 829–880.
20. Karnezis IA, Panagiotopoulos E, Tyllianakis M, Megas P, Lambiris E. Correlation between radiological parameters and patient-rated wrist dysfunction following fractures of the distal radius. Injury. 2005; 36(12):1435–1439. PMID: 16256994.

21. Hake ME, Goulet JA. Open reduction and internal fixation of the tibial plateau through the anterolateral approach. J Orthop Trauma. 2016; 30(Suppl 2):S28–S29. PMID: 27441932.

22. Yoon YC, Oh JK, Oh CW, Sahu D, Hwang JH, Cho JW. Inside out rafting K-wire technique for tibial plateau fractures. Arch Orthop Trauma Surg. 2012; 132(2):233–237. PMID: 22015645.

23. Konstantinidis L, Helwig P, Strohm PC, Hirschmuller A, Kron P, Sudkamp NP. Clinical and radiological outcomes after stabilisation of complex intra-articular fractures of the distal radius with the volar 2.4 mm LCP. Arch Orthop Trauma Surg. 2010; 130(6):751–757. PMID: 19894054.
Fig. 2
Operative procedures. (A) With a Freer elevator inserted through the volar fracture site and positioned under the subchondral bone of the radiocarpal joint, the joint surface was elevated and restored using the leverage technique. (B) After temporary K-wire fixation at adequate reduction, proximal cortical screw fixation for compression was followed by proximal locking screw fixation with the plate appropriately positioned. Anteroposterior (C) and lateral (D) C-arm images after final fixation: 2.4-mm locking screws were inserted into the distal fixed locking holes of the plate.
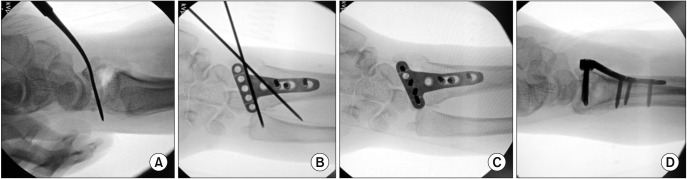
Fig. 3
A 53-year-old female fell from a height, resulting in a left comminuted distal radius fracture with volar free fragments beyond the watershed line. (A, B) Initial anteroposterior and lateral plain radiographs. (C, D) In computed tomographic assessment, we observed a transverse fracture located beyond the watershed line, extending into the joint space with dorsal displacement, and dorsal cortex comminution. (E) Freer leverage reduction and temporary fixation were conducted after fracture exposure. (F, G) Ten months after surgery, at the final follow-up, plain radiographs showed complete bony union on plain anteroposterior and lateral radiographs. (H) The patient achieved volar flexion of 70° and dorsal flexion of 80°. The Disabilities of Arm, Shoulder and Hand scores was 12.0. The pain visual analogue scale score was 1. The modified Mayo wrist score was 85.
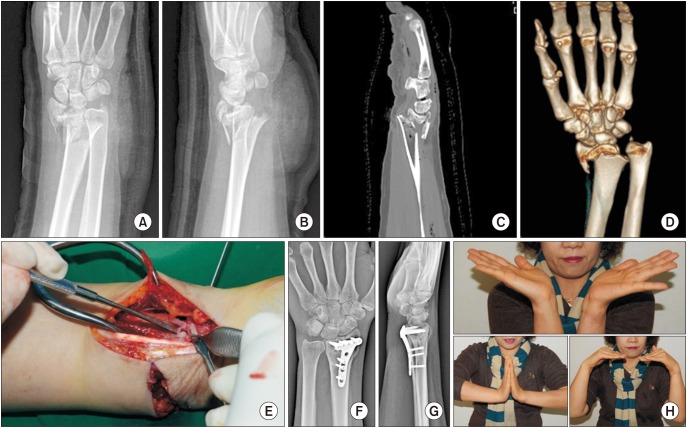
Table 1
Demographic and Clinical Characteristics of Patients
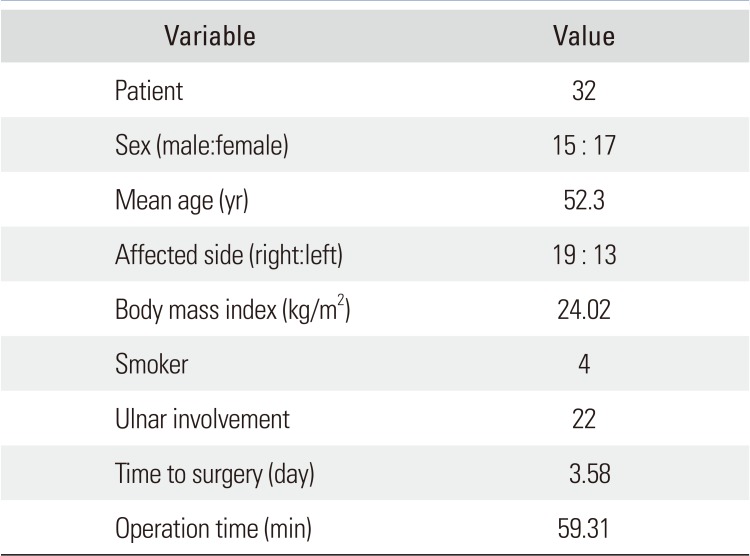
Table 2
Radiological Outcome after Radius Surgery
| Variable | Mean (range) |
|---|---|
| Step-off (mm) | 1.10 (0.14–1.87) |
| Radial height (mm) | 10.10 (6.3–13.4) |
| Volar tilt (°) | 7.05 (1.3–13.5) |
| Radial inclination (°) | 24.06 (17.8–37.6) |
Table 3
ICC of Variables
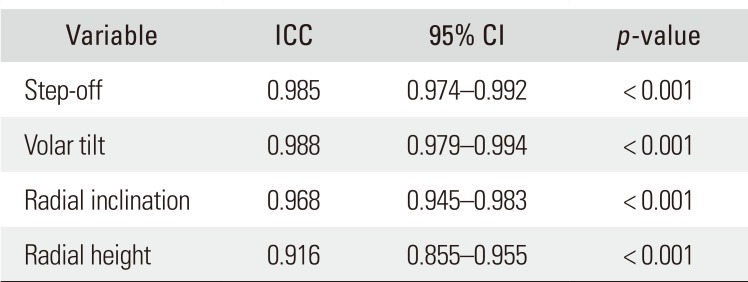
| Variable | ICC | 95% CI | p-value |
|---|---|---|---|
| Step-off | 0.985 | 0.974–0.992 | < 0.001 |
| Volar tilt | 0.988 | 0.979–0.994 | < 0.001 |
| Radial inclination | 0.968 | 0.945–0.983 | < 0.001 |
| Radial height | 0.916 | 0.855–0.955 | < 0.001 |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download