Abstract
Purpose
Peripheral arterial disease (PAD) has been a major public health issue in the elderly. Advances in endovascular surgery have led to a substantial shift in the management of PAD. Although the nationwide trend of PAD treatment in the Western countries was reported, limited data have been available on this in Korea. This study examined the national trend in the treatment of PAD in Korea over the past decade.
Methods
Health Insurance Review and Assessment Service data were used. We sought to analyze trends in the open and endovascular surgery for the treatment of PAD in Medicare beneficiaries between 2004 and 2013. We also analyzed trends in each types of surgery in the lower extremity. A linear-by-linear association was performed to determine the changes of PAD treatment for this period.
Results
The rate of open surgery per 100,000 Medicare beneficiaries decreased significantly from 8 procedures in 2004 to 6 in 2013. At the same time, endovascular surgery increased from 23 procedures in 2004 to 59 in 2013. Endovascular surgery in the lower extremity increased more than twofold, while the open surgery decreased by 39%. The rate of balloon angioplasty among endovascular surgery was increased by almost threefold, while the bypass surgery using artificial graft decreased by half.
Peripheral arterial disease (PAD), a common vascular problem, carries an increased risk of cardiovascular morbidity and mortality [1]. It can lead to a decreased quality of life and possible major limb loss [2]. Patients with PAD are at up to 6-fold greater risk of death from coronary heart disease and 3-fold greater risk of all-cause mortality than patients without evidence of the disease [3]. Generally, at one year of PAD, 30% of patients are expected to undergo amputation, with only 45% remaining alive with both limbs [1].
Although open surgery for PAD has been the standard of care, endovascular surgery is an increasingly accepted means of treatment for PAD [1]. Recent advances in technology and technique have allowed endovascular surgery to be applied to an ever-increasing number of patients. In western country, analysis of trends in lower extremity endovascular interventions and bypass surgery in Medicare beneficiaries between 1996 and 2006 has shown that the use of endovascular interventions grow substantially at 330%, while bypass surgery has decreased by 42% [4]. Another study on the lower extremity revascularization using National Inpatient Sample data from the United States (US) has revealed that open revascularizations have decreased from 111 to 68 per 100,000 populations, while endovascular revascularizations have almost doubled (from 45 to 94) in the period between 1998 and 2007 [5].
Despite these well designed studies for national trends of lower extremity endovascular and open surgery in Western countries, there has been very little analysis of changes on national volume of lower extremity revascularization in Asian countries. Therefore, the objective of this study was to evaluate the national trends of treatment modality for PAD in Korea.
Data of Health Insurance Review and Assessment Service (HIRA) were used as source for evaluating the trend of treatment for PAD in Korea. South Korea has a universal health coverage system. The National Health Insurance covers approximately 98% of the overall Korean population. Claims data of HIRA is collected when healthcare service providers in South Korea seek reimbursements for healthcare services that the National Health Insurance Corporation agrees to cover. The annual number of Korean patients that have submitted health insurance claims is approximately 46 million. The claims data of HIRA is a national data compiled from healthcare providers across the country corresponding to the number of claims submitted by patients [6].
Electronic data interchange (EDI) database of HIRA has the operation and management codes. Terms of treatment for PAD were collected from EDI codes from HIRA. The EDI codes for open surgery are listed in Table 1. We collected all EDI codes related to PAD. Codes for commonly performed procedures on the lower extremity PAD include O0163 to O0170 for terms of femoropopliteal, femorotibial/popliteotibial, and femoroperoneal/popliteoperoneal bypass. Each bypass surgery has two separate codes with the conduit of autologous vein and artificial graft. The codes of O1645 and 1646 are related to bypass surgery such as pedal or plantar bypass. The codes for the treatment of aorta, iliac artery and upper extremity artery are O0161 and O0162. Endarterectomy with or without patch closure of abdominal aorta, iliac, and other arteries is allocated with the codes of O2016-O2068.
There are five EDI codes of the endovascular surgery for PAD (Table 2). Endovascular treatments of aorta with balloon angioplasty and stent placement were given the codes of M6595 and M6603, respectively. Endovascular procedures with balloon angioplasty and stent placement in other arteries except aorta were given the codes of M6597 and M6605, respectively. The code of M6620 included any types of percutaneous atherectomy such as directional, rotational, or ablative atherectomy.
For the evaluation of trend of PAD treatment for the recent 10 years, EDI database from 2004 to 2013 of HIRA was used. We calculated the total number of open surgery and endovascular surgery for the treatment of PAD for this period. From these dataset, we analyzed the trend for revascularization on lower extremity, the codes of O0163-O0170, O1645, O1646 for open surgery, and the codes of M6597 and M6605 for endovascular surgery. We analyzed the utilization of autologous vein, artificial graft, and endarterectomy for open surgery. The rates of balloon angioplasty, stent placement, and percutaneous atherectomy were analyzed for this period. The present study was approved by the Hospital Institutional Review Board (IRB). And the IRB authority did waive the requirement to obtain informed consent because HIRA data did not include the personal information.
For statistical analysis, a linear-by-linear association was performed to determine the trend of PAD treatment for this period. Altman method was used to evaluate the trend of population-adjusted frequencies. A P-value less than 0.05 (two sided) was considered statistically significant. Data were analyzed using IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA).
A total of 233,408 patients received open or endovascular procedures for PAD, including 37,464 open surgeries and 195,944 endovascular surgeries. Detail numbers of the patients each year are summarized in Table 3. The proportion of open surgery decreased from 26.0% in 2004 to 8.9% in 2013 (risk ratio [RR], 0.73; 95% confidence interval [CI], 0.69-0.77). At the same period, the number of endovascular surgery increased from 74.0% in 2004 to 91.1% in 2013 (RR, 2.62; 95% CI, 2.56-2.68). These trends were all statistically significant (P < 0.0001). Age distribution of patients is shown in Fig. 1. The revascularization was most frequently performed in the patients in 60's followed by 70's and 50's.
The rate of patients undergoing open and endovascular procedures for PAD during the study period are displayed in Fig. 2. The number of total revascularization increased significantly (P < 0.0001) from 14,522 in 2004 to 32,353 in 2013 (RR, 2.13; 95% CI, 2.09-2.17). During the study period, the use of endovascular surgery grew significantly (P < 0.0001) from 10,748 in 2004 to 29,469 in 2013 (RR, 2.62; 95% CI, 2.56-2.68), while open revascularization decreased from 3,774 in 2004 to 2,884 in 2013 (RR, 0.73; 95% CI, 0.69-0.77) (Fig. 2A). Population-adjusted frequencies per 100,000 of total, open, and endovascular surgery over 10 years are shown in Fig. 2B. The rate of total revascularization per 100,000 Medicare beneficiaries substantially increased during the study period from 31 procedures in 2004 to 65 in 2013 (RR, 2.10; 95% CI, 1.37-3.22). At the same time, endovascular surgery increased with the similar pattern from 23 procedures in 2004 to 59 in 2013 (RR, 2.57; 95% CI, 1.58-4.15). These trends were all statistically significant (P < 0.0001). However, open surgery per 100,000 Medicare beneficiaries decreased from 8 procedures in 2004 to 6 in 2013 (RR, 0.75; 95% CI, 0.26-2.16).
The trends of lower extremity revascularization are shown in Fig. 3. The number of total revascularization was increased from 12,244 in 2004 to 25,819 in 2013 (RR, 2.01; 95% CI, 1.97-2.06) with statistical significance (P < 0.0001). The pattern of endovascular surgery on the lower extremity was similar to that of the total revascularization. During the study period, the rate of endovascular surgery increased from 9,047 in 2004 to 23,791 in 2013 (RR, 2.51; 95% CI, 2.45-2.57). The rate of open surgery on the lower extremity decreased from 3,197 to 2,028 (RR, 0.61; 95% CI, 0.57-0.64).
The frequency of specific procedure using open surgery is shown in Fig. 4A. The overall decline of lower extremity open surgery was due to the decreasing frequency of bypass surgery. During the study period, we observed a 49% and 44% decline of bypass with artificial graft and autologous vein, respectively in 2013, compared to 10 years ago. However, substantial change was observed in patients with endarterectomy. Endarterectomy increased by almost 337% from 2004 to 2013. The overall frequency of endovascular surgery was markedly increased. The specific types of endovascular surgery including balloon angioplasty, stent placement, and percutaneous atherectomy are shown in Fig. 4B. Although there was a stable increment of stent placement (RR, 1.96; 95% CI, 1.88-2.04), the rate of balloon angioplasty was dramatically increased from 5,665 in 2004 to 16,747 in 2013 (RR, 2.82; 95% CI, 2.74-2.91). The rate of percutaneous atherectomy was markedly increased from 4 in 2004 to 107 in 2013 (RR, 25.5; 95% CI, 9.41-69.31).
Endovascular approach is thought as an acceptable option for management of PAD patients. Therefore, its frequency was rapidly increased in the last decade. In the US, the endovascular interventions grew 3.3 times, while bypass surgery decreased by 42% [4]. In a Canadian study, age-adjusted and sex-adjusted rate of arterial bypass surgery decreased significantly (from 77 to 61 per 100,000 populations), whereas the rate for percutaneous transluminal angioplasty (PTA) increased significantly (from 59 to 75 per 100,000 population) [7]. Chang et al. [8] analyzed nationwide inpatient databases in Taiwan from 2000 to 2011. Although the incidence of bypass surgery for PAD estimated at 8.4 per 100,000 was reduced to 6.4 per 100,000, the number of PTA procedures remarkably increased by 15 times (from 600/yr to 9,100/yr) from 2000 to 2011. Our study showed similar trend. Total revascularization was expanded 213% due to dramatic increase of endovascular procedure.
There are several explanations on the expansion of the endovascular revascularization of PAD. First, the risk factors for PAD have been increased. Age is one of the main risk factors in PAD. In South Korea, proportion of the population over 65 increased from 8.3% in 2004 to 12.2% in 2013 [9]. Aging process in South Korea population might affect the incidence of PAD and subsequent increment of the endovascular revascularization frequency. Diabetes and chronic kidney disease on hemodialysis are independent risk factors for the development of PAD [1011]. From 1970 to 2000, the prevalence of diabetes in Korea increased about threefold [12]. Epidemiologic study after this period showed that the incidence of diabetes of aged 70-79 years was increased from 2009 to 2011 [13]. Registry data for end stage renal disease in Korea revealed that the number of patients with ESRD was increased very rapidly [14]. The increasing rate of prevalence per year was about 12% during 2000-2009. Second, the endovascular surgery has a less invasive nature. Therefore, a decrease in the threshold for endovascular approach in PAD likely represents one major contribution to the increase of this procedure [4]. Third, endovascular procedures are less durable than open surgery [15]. Therefore, repeated interventions might be needed to maintain reasonable clinical outcomes.
Population-based trends of revascularization showed similar with Western countries. However, the actual numbers of revascularization per 100,000 Medicare beneficiaries were quite different from the US study. Although US study showed 138 to 455 of endovascular treatment and 126 to 219 of bypass surgeries per 100,000 Medicare beneficiaries [4], our study revealed almost one-tenth of revascularization performed in Korea compared to the data of US Medicare beneficiaries. The actual frequency of revascularization in Korea was similar to the study of Taiwan, in which the frequency was reported to be doubled from 3.73 per 10,000 in 2000 to 7.48 per 10,000 in 2011 [8]. Deployment of medical resources for vascular surgeries in Korea needs to be further evaluated by health policy authority.
Although there was an overall decreasing trend of open surgery in the current study, a subset of endarterectomy was increased by more than threefold. The increment of common femoral endarterectomy likely represents a major contribution to the increase of this procedure. Furthermore, many of the femoral endarterectomy (FEA) might have been performed as an adjunct procedure of hybrid surgery in patient with complex involvement of atherosclerosis. Joh et al. [16] reported that FEA was the most common open surgery in hybrid revascularization for PAD.
In the analysis of endovascular surgery, the rate of balloon angioplasty was increased by 282%. The rate of percutaneous atherectomy was markedly increased from 4 in 2004 to 107 in 2013 (RR, 25.5; 95% CI, 9.41-69.31). The increment of infrapopliteal intervention likely represents a major contribution to the rapid increase of balloon angioplasty. With the high prevalence of diabetes and ESRD in Korea [1214], the most common endovascular procedure was done for lesions of popliteal or tibial arteries. Although the placement of stent in this region showed reasonable results in some studies [1718], balloon angioplasty is accepted as the primary treatment because of there is insufficient evidence to support the superiority of primary stenting [19]. The dramatic increase of the rate of atherectomy might be due to introduction of directional atherectomy devices and their marketing [2021].
Several limitations of this study should be acknowledged. This is a retrospective study based on an administrative database, so there is an intrinsic limit to the number of variables that can be measured. And with the current HIRA code, it is difficult to distinguish the open surgery of acute thrombotic or embolic occlusion of the peripheral artery. Also the HIRA code, M6597, includes PTA of PAD as well as arteriovenous access for hemodialysis. Therefore, this count can be overestimated. There is another limitation to evaluate the trends of lower extremity revascularization. While the code of M6597 and M6605 include the PTA and/or stenting for iliac lesions, the O0161 and O0162 for the bypass surgery for iliac lesion such as femorofemoral bypass was not included. In our study, the code of O0161 and O0162 was not included because these codes include the bypass surgery of upper extremity such as axillo-axillary or subclavio-subclavian arterial bypass. Follow-up data and longterm outcomes are unavailable. In addition, further evaluation is needed after more detailed data are collected, such as the prevalence of comorbidities, the lengths of hospital stays, the amputation rate, and the mortality rate according to treatment modality.
In conclusion, endovascular surgery in the lower extremity increased more than twofold, while the open surgery on the lower extremity decreased by 39%. Balloon angioplasty in endovascular surgery increased by almost threefold. At the same time, the bypass surgery using artificial graft decreased by about 50%. Further study is needed to identify the change of amputation rate and direct causative link between surgery for PAD and limb salvage.
Figures and Tables
Fig. 2
(A) Trends in total revascularization, endovascular and open surgery for peripheral arterial disease, 2004-2013. (B) Trends in total revascularization, endovascular and open surgery for peripheral arterial disease per 100,000 Medicare beneficiaries, 2004-2013. RR, risk ratio; CI, confidence interval.

Fig. 3
Trends in total revascularization, endovascular and open surgery for lower extremity arterial disease, 2004-2013. LE, lower extremity; RR, risk ratio; CI, confidence interval.
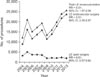
Fig. 4
(A) Trends in bypass with artificial graft or autologous vein and endarterectomy for the treatment of peripheral arterial disease, 2004-2013. (B) Trends in balloon angioplasty, stenting, and percutaneous for the treatment of peripheral arterial disease, 2004-2013. RR, risk ratio; CI, confidence interval.

ACKNOWLEDGEMENTS
This work was supported by a grant from the Kyung Hee University in 2010 (KHU-20101886).
References
1. Davies MG. Criticial limb ischemia: epidemiology. Methodist Debakey Cardiovasc J. 2012; 8:10–14.
2. Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001; 286:1317–1324.
3. Aronow H. Peripheral arterial disease in the elderly: recognition and management. Am J Cardiovasc Drugs. 2008; 8:353–364.
4. Goodney PP, Beck AW, Nagle J, Welch HG, Zwolak RM. National trends in lower extremity bypass surgery, endovascular interventions, and major amputations. J Vasc Surg. 2009; 50:54–60.
5. Egorova NN, Guillerme S, Gelijns A, Morrissey N, Dayal R, McKinsey JF, et al. An analysis of the outcomes of a decade of experience with lower extremity revascularization including limb salvage, lengths of stay, and safety. J Vasc Surg. 2010; 51:878–885. 885.e1
6. Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health. 2014; 36:e2014008.
7. Al-Omran M, Tu JV, Johnston KW, Mamdani MM, Kucey DS. Use of interventional procedures for peripheral arterial occlusive disease in Ontario between 1991 and 1998: a population-based study. J Vasc Surg. 2003; 38:289–295.
8. Chang NT, Chan CL, Lu YT, Hsu JC, Hsu YN, Chu D, et al. Invasively-treated incidence of lower extremity peripheral arterial disease and associated factors in Taiwan: 2000-2011 nationwide hospitalized data analysis. BMC Public Health. 2013; 13:1107.
9. Statistics Korea. Aging trend in Korea [Internet]. Daejeon: Statistics Korea;2015. cited 2015 Jun 7. Available from: http://sgis.kostat.go.kr.
10. Garimella PS, Hart PD, O'Hare A, DeLoach S, Herzog CA, Hirsch AT. Peripheral artery disease and CKD: a focus on peripheral artery disease as a critical component of CKD care. Am J Kidney Dis. 2012; 60:641–654.
11. Conte MS. Diabetic revascularization: endovascular versus open bypass--do we have the answer? Semin Vasc Surg. 2012; 25:108–114.
12. Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011; 35:303–308.
13. Koo BK, Lee CH, Yang BR, Hwang SS, Choi NK. The incidence and prevalence of diabetes mellitus and related atherosclerotic complications in Korea: a National Health Insurance Database Study. PLoS One. 2014; 9:e110650.
14. Jin DC. Current status of dialysis therapy in Korea. Korean J Intern Med. 2011; 26:123–131.
15. Rana MA, Gloviczki P. Endovascular interventions for infrapopliteal arterial disease: an update. Semin Vasc Surg. 2012; 25:29–34.
16. Joh JH, Joo SH, Park HC. Simultaneous hybrid revascularization for symptomatic lower extremity arterial occlusive disease. Exp Ther Med. 2014; 7:804–810.
17. Rand T, Basile A, Cejna M, Fleischmann D, Funovics M, Gschwendtner M, et al. PTA versus carbofilm-coated stents in infrapopliteal arteries: pilot study. Cardiovasc Intervent Radiol. 2006; 29:29–38.
18. Randon C, Jacobs B, De Ryck F, Vermassen F. Angioplasty or primary stenting for infrapopliteal lesions: results of a prospective randomized trial. Cardiovasc Intervent Radiol. 2010; 33:260–269.
19. Wu R, Yao C, Wang S, Xu X, Wang M, Li Z, et al. Percutaneous transluminal angioplasty versus primary stenting in infrapopliteal arterial disease: a metaanalysis of randomized trials. J Vasc Surg. 2014; 59:1711–1720.
20. McKinsey JF, Zeller T, Rocha-Singh KJ, Jaff MR, Garcia LA. DEFINITIVE LE Investigators. Lower extremity revascularization using directional atherectomy: 12-month prospective results of the DEFINITIVE LE study. JACC Cardiovasc Interv. 2014; 7:923–933.
21. Roberts D, Niazi K, Miller W, Krishnan P, Gammon R, Schreiber T, et al. Effective endovascular treatment of calcified femoropopliteal disease with directional atherectomy and distal embolic protection: final results of the DEFINITIVE Ca++ trial. Catheter Cardiovasc Interv. 2014; 84:236–244.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download