Abstract
Purpose
Pneumomediastinum is rare in children and adolescents, and its causes have not yet been clearly determined. We aimed to identify the causes, clinical manifestations and prognosis of noniatrogenic pneumomediastinum in children.
Methods
From February 2007 to June 2014, we retrospectively investigated 121 patients with pneumomediastinum under 18 years of age in 2 hospitals. Eighteen patients with pneumomediastinum after thoracotomy and 35 patients with iatrogenic pneumomediastinum were excluded.
Results
Sixty-eight patients were divided into 4 age groups: those under 1 year of age (n=9, 13.2%), those 1 to 5 years of age (n=9, 13.2%), those 6 to 10 years of age (n=17, 25.0%) and those over 11 years of age (n=33, 48.5%). Chest pain (n=43, 63.2%) was the most common initial complaint and subcutaneous emphysema was identified in 18 patients (26.5%). Chest x-ray was diagnostic in all except 9 patients (13.2%). Predisposing causes of pneumomediastinum were idiopathic (n=26, 38.2%), respiratory tract infection (n=23, 33.8%), asthma exacerbation (n=4, 5.9%), trauma (n=4, 5.9%), endobronchial foreign body (n=2, 2.9%), interstitial lung disease (n=5, 7.4%), and neonatal respiratory disease (n=4, 5.9%). Chest pain (P<0.001) and idiopathic cause (P=0.001) were shown to linearly increase with age. On the contrary, tachypnea (P<0.001), dyspnea (P=0.016), and interstitial lung disease (P=0.008) were shown to have a decreasing linear association with age. The length of hospital stay was significantly increased in patients with interstitial lung disease (P=0.042), those with pneumothorax (P=0.044), and those without chest pain (P=0.013).
Conclusion
According to age groups, there were significant differences in causes and clinical manifestations. In particular, pneumomediastinum that developed in younger patients with interstitial lung disease showed unfavorable outcomes, such as dyspnea, pneumothorax, and increased length of hospital stay. Therefore, precise evaluation of predisposing causes and careful management are needed for children with pneumomediastinum.
Figures and Tables
 | Fig. 1Selection of the patients and classification by predisposing causes. ILD, interstitial lung disease. *ILD included humidifier disinfectant-associated children's interstitial lung disease (n=4) and idiopathic pulmonary fibrosis (n=1). |
Table 1
General characteristics of the patients (n=68)

Table 2
Predisposing causes of pneumomediastinum
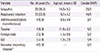
Table 3
Clinical differences of patients according to age

Table 4
Comparisons of length of hospital stay by sex, predisposing causes, symptoms/signs, and complication

References
1. Okada M, Adachi H, Shibuya Y, Ishikawa S, Hamabe Y. Diagnosis and treatment of patients with spontaneous pneumomediastinum. Respir Investig. 2014; 52:36–40.

2. Banki F, Estrera AL, Harrison RG, Miller CC 3rd, Leake SS, Mitchell KG, et al. Pneumomediastinum: etiology and a guide to diagnosis and treatment. Am J Surg. 2013; 206:1001–1006.

5. Mumford AD, Ashkan K, Elborn S. Clinically significant pulmonary barotrauma after inflation of party balloons. BMJ. 1996; 313:1619.

6. Grossman A, Romem A, Azaria B, Goldstein L, Barenboim E. Pneumomediastinum in student aviators: 10 cases with return to flying duty. Aviat Space Environ Med. 2005; 76:63–65.
7. Karakaya Z, Demir S, Sagay SS, Karakaya O, Ozdinc S. Bilateral spontaneous pneumothorax, pneumomediastinum, and subcutaneous emphysema: rare and fatal complications of asthma. Case Rep Emerg Med. 2012; 2012:242579.

8. Jeng MJ, Lee YS, Tsao PC, Soong WJ. Neonatal air leak syndrome and the role of high-frequency ventilation in its prevention. J Chin Med Assoc. 2012; 75:551–559.

9. Lim EJ, Park YB, Kim CH, Park DS, Kim MG, Kim CH, et al. A recurrent spontaneous pneumomediastinum. Tuberc Respir Dis. 2005; 59:696–699.

10. Jung AY, Yang I, Go HS, Shin SM, Yoon HK, Woo JY, et al. Imaging neonatal spontaneous pneumomediastinum using ultrasound. J Med Ultrason (2001). 2014; 41:45–49.

11. Sahni S, Verma S, Grullon J, Esquire A, Patel P, Talwar A. Spontaneous pneumomediastinum: time for consensus. N Am J Med Sci. 2013; 5:460–464.

12. Chalumeau M, Le Clainche L, Sayeg N, Sannier N, Michel JL, Marianowski R, et al. Spontaneous pneumomediastinum in children. Pediatr Pulmonol. 2001; 31:67–75.

13. Kim HY, Kim KM, Kim SH, Son SK, Park HJ. Clinical manifestations of respiratory viruses in hospitalized children with acute viral lower respiratory tract infections from 2010 to 2011 in Busan and Gyeongsangnam-do, Korea. Pediatr Allergy Respir Dis. 2012; 22:265–272.

14. Hatamabadi HR, Esmailnejad SS, Khazayi AR, Masjoudi B. A diagnostic challenge of an unusual presentation of pneumomediastinum. Chin J Traumatol. 2014; 17:44–47.
15. Chiu CY, Wong KS, Yao TC, Huang JL. Asthmatic versus non-asthmatic spontaneous pneumomediastinum in children. Asian Pac J Allergy Immunol. 2005; 23:19–22.
16. McSweeney WJ, Stempel DA. Non-iatrogenic pneumomediastinum in infancy and childhood. Pediatr Radiol. 1973; 1:139–144.

17. Kim KW, Ahn K, Yang HJ, Lee S, Park JD, Kim WK, et al. Humidifier disinfectant-associated children's interstitial lung disease. Am J Respir Crit Care Med. 2014; 189:48–56.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download