Abstract
Unsintered hydroxyapatite (u-HA) and poly-L-lactide (PLLA) composites (u-HA/PLLA) are osteoconductive and biodegradable. Screw (Super-Fixsorb MX30) and plate (Super-Fixsorb MX40 Mesh) systems made of u-HA/PLLA are typically used in small bones in maxillofacial surgeries. After the resection of bone tumors in larger bones, reconstructions with β-tricalcium phosphate (β-TCP) implants of strong compression resistance have been reported. After a resection, when the cavity is hemispheric- or concave-shaped, stabilization of the implanted β-TCP block is necessary. In the current series, u-HA/PLLA were used to stabilize the mechanically strong implanted low-porous β-TCP blocks in six bone tumor cases, including three giant cell tumors of bone, and one case each of chondroblastoma, chondrosarcoma, and parosteal osteosarcoma. The mean age of patients at the time of surgery was 31.3 years (range, 19 to 48 years). The bones involved were two ilia (posterior), a femur (diaphysis to distal metaphysis), and three tibias (proximal epiphysis, proximal metaphysis to epiphysis, and distal metaphysis to epiphysis). Neither displacement of the implanted β-TCP block nor any u-HA/PLLA-related complications were observed. The radiolucent character of the u-HA/PLLA did not hinder radiological examinations for potential signs of tumor recurrence. The method of using u-HA/PLLA components for the stabilization of β-TCP blocks makes the procedure easy to perform and reliable. It can extend the application of β-TCP blocks in reconstruction surgery.
After curettage of benign bone tumors including giant cell tumor of bone, the bone cavity is often filled with bone autograft, polymethylmethacrylate bone cement,1) or synthetic bone materials, including β-tricalcium phosphate (β-TCP).2) Osteosynthetic materials to promote bone incorporation after curettage are ideal.2) With an allograft, it is difficult to maintain mechanical strength postimplantation until bone incorporation. One reported method used to overcome this lack of mechanical strength is a cortical allograft.3) However, a cortical allograft may not be available even in those institutes in which allografts are available.
β-TCP is a highly porous ceramic bone substitute that promotes osteogenesis.4) A hard-type β-TCP has a porosity of less than 71% but greater than 65%, whereas ordinary β-TCP has a porosity of less than 80% but greater than 71%. The compressive strength of the hardtype β-TCP (15 MPa) is more than ten times greater than the strength of the standard β-TCP (1.5 MPa, Superpore; PENTAX New Ceramics Division, HOYA Corp., Tokyo, Japan). Therefore, the hard-type β-TCP is stronger initially than normal cancellous bone.5)
Reconstruction after bone resection with a hardtype β-TCP block for giant cell tumor of bone around the knee has been reported.2) When the cavity in the host bone after bone tumor resection is hemispheric- or concave-shaped, stabilization of the implanted β-TCP block is necessary. For stabilization of the implanted β-TCP blocks, the use of bulky metal implants to treat fractured bone requires larger skin incisions, whereas more delicate implants would be sufficient to stabilize the β-TCP block implantation.
The unsintered hydroxyapatite and poly-L-lactide composites (u-HA/PLLA) are biodegradable, osteoconductive, and osteosynthetic materials that promote the replacement of bone.6) The u-HA/PLLA screw (Super-Fixsorb MX30; Johnson & Johnson, Tokyo, Japan) and plate (Super-Fixsorb MX40 Mesh; Takiron Co., Osaka, Japan) systems have applications in maxillofacial surgeries.789) In the current series, plates and screws made from u-HA/PLLA are used for the stabilization of implanted β-TCP blocks after curettage or resection of bone tumors.
Six cases with bone tumors that had been reconstructed with implanted β-TCP blocks stabilized by u-HA/PLLA are reported. Among the six cases, four patients were male and two patients were female. Their mean age at the time of surgery was 31.3 years (range, 19 to 48 years). A preoperative biopsy was used to diagnose each case. Computed tomography (CT) and magnetic resonance imaging (MRI) were performed in all cases. The diagnoses and the locations included giant cell tumors of bone in the posterior ilium, in the proximal tibia from the metaphysis to the epiphysis, and in the distal tibia from the metaphysis to the epiphysis (one case each); a chondroblastoma in the proximal tibia at the epiphysis (one case); a conventional chondrosarcoma in the posterior ilium (one case); and a parosteal osteosarcoma in the distal femur extending from the posterior side of the diaphysis to the epiphysis (one case). Curettage was performed for the cases with giant cell tumors of bone and the chondroblastoma case, whereas en-bloc resection was performed for the cases with chondrosarcoma and parosteal osteosarcoma. After surgery, the mean defect length was 4.9 ± 2.2 cm (range, 2.2 to 18 cm).
After curettage or resection of the lesion, a hard-type β-TCP block was used to fill the cavity. A screw and plate made from u-HA/PLLA was used to stabilize the hard-type β-TCP block. The shaped u-HA/PLLA plate was laid over the hard-type β-TCP block and was fixed to either the adjacent bone or underlying bone through the β-TCP block using 4.5 mm u-HA/PLLA screws (Fig. 1). When there was still space between the β-TCP block and the host bone, standard β-TCP particles were added. The β-TCP were 10 mm thick rectangular blocks with sizes of 10 × 15 mm, 20 × 20 mm or 30 × 30 mm. The cavity was filled with a combination of these different-sized β-TCP blocks. The average number of β-TCP blocks used was 2.6 ± 1.2, ranging from 1 to 4. The mean number of screws used was 3.1 ± 2.0, ranging from 1 to 5. Plain radiographs were taken to evaluate the implants every month after the operation for the first 4 months and every 2 months for the following 4 months. Following that, the interval for radiographic evaluation depended on the individual case according to the bone incorporation and the neoplastic nature of the lesion. The mean follow-up time was 14 months (range, 7 to 22 months). No dislocation of the implanted β-TCP block was visible during the follow-up period. No complications associated with the u-HA/PLLA were observed in any of the cases.
The patient with chondrosarcoma in the ilium was a 41-year-old male. The osteolytic lesion with calcification was located posteriorly, adjacent to the sacroiliac joint. After en-bloc resection, the defect was extended to 4.0 cm long and filled with two β-TCP blocks, and a β-TCP plate and five u-HA/PLLA screws were attached (Fig. 2). A second case in the ilium involved a giant cell tumor of bone in a 29-year-old female. The osteolytic lesion had thinned the cortex and was located posteriorly adjacent to the sacroiliac joint. Curettage was performed to create a defect with a 4 cm maximum length. The defect was filled with four β-TCP blocks, and a β-TCP plate and five u-HA/PLLA screws were attached. In both cases, full weight bearing was allowed after the operation. Use of a crutch was recommended for 3 months because of slight pain after the operation. In both cases, approximately 3 months after surgery, the periphery of the implanted β-TCP block became misshapen, and the absence of a clear demarcation between the implant and bone was more pronounced 6 months after surgery.
The diaphysis case presented as a well-differentiated parosteal osteosarcoma of the posterior femoral diaphysis extending 6.5 cm to the metaphysis in a 19-year-old female. Ossified bony protuberances from the posterior surface of the femur were seen. En-bloc resection was performed, and the 8 cm defect was filled with three β-TCP blocks, followed by stabilization with two β-TCP plates and five u-HA/PLLA screws (Fig. 3). Weight bearing was allowed after the operation. Because of the large incision of the posterior distal thigh extending to the knee, the patient experienced difficulty in knee extension of about −10°. A crutch was used until full extension of the knee joint was recovered 3 months after surgery, when normal gait was regained. Bone incorporation of the implanted β-TCP at the periphery was recognized adjacent to the normal bone tissue 3 months after surgery.
Both cases that involved the metaphysis were giant cell tumors of bone. Plain radiographs and CT showed an osteolytic and expansile lesion. The reconstruction method has been reported.2) After curettage of the lesion, block-shaped hard-type β-TCP for the cavity, and standard β-TCP particles to fill in additional space were used. In both cases, to increase the potential for success of the β-TCP reconstruction method, u-HA/PLLA plates and screws were used to stabilize the implanted β-TCP block (Fig. 4). In a 36-year-old male with a 4 cm-giant cell tumor of bone in the proximal tibia, three β-TCP blocks, a β-TCP plate and two u-HA/PLLA screws were used. In a 48-year-old male with a 3.5 cm giant cell tumor in the distal tibia, three β-TCP blocks, a β-TCP plate and a u-HA/PLLA screw were used. Rehabilitation was the same as that reported elsewhere,2) in which the patient used two crutches to avoid a weight bearing load greater than 5 kg. Weight bearing was allowed about 3 weeks after surgery when bone incorporation was recognized by vagueness of the β-TCP particles and new bone was apparent on the plain radiographs. Full range of motion of the knee and ankle in each case was achieved, and normal gait ability was regained in both cases by 6 months after the operation.
A 2 cm chondroblastoma case was identified in the proximal tibial epiphysis of a 16-year-old male. After curettage of the lesion, a 2.2 cm defect was filled with a β-TCP block, and a β-TCP plate and u-HA/PLLA screws were applied (Fig. 5). Full weight bearing was allowed after the operation because the lesion was posteriorly located, avoiding the weight bearing axis. Full range of knee was regained. The periphery adjacent to the normal bone tissue became obscure, suggesting bone incorporation at around 3 months after the operation.
Several different bioceramic materials of β-TCP, calcium sulfate and hydroxyapatite have been used in orthopedic surgery as bone substitutes.10) Hydroxyapatite is less readily resorbed and blocks new bone formation and remodeling, resulting in poor local stability or a permanent stress concentration.11) Among the bone substitutes, β-TCP is relatively balanced between scaffold absorption and bone formation, and therefore β-TCP composite is widely used for filling bone defects. However, the “standard” β-TCP, like an autograft, is not strong mechanically before its incorporation into bone.4) Weight bearing should begin after complete bone incorporation of “standard” β-TCP or autograft into the whole lesion, but sometimes it is difficult to determine when bone has been incorporated into the center of the lesion.2)
After implantation, β-TCP strength increases linearly with bone incorporation.4) Initial compression strength is important after implantation. Unlike ordinary β-TCP, the hard-type β-TCP has greater initial mechanical strength than normal cancellous bone.5) In the current series with hemispheric- or concave-shaped bone defects, full weight bearing was allowed after the operation for the cases in the posterior pelvis, the distal femur with a cortical diaphyseal defect extending to the epiphysis, and for the case involving the proximal tibial epiphysis along the non-weight bearing axis. For cases that involve the tibial metaphysis to the epiphysis extending into the subarticular space, full weight bearing starts around 3 months after surgery when bone incorporation in the subarticular area is seen, but before complete bone incorporation of the lesion.2) Even in cases extending to the subarticular space, this reconstructive procedure with hard-type β-TCP provides not only excellent knee function but also an opportunity for early weight bearing.2)
In the current series, rectangular hard-type β-TCP blocks 10 mm thick and 10, 20 or 30 mm wide were used. It is easy to shape the hard-type β-TCP block to fit the bone cavity.21213) In order to stabilize the implanted β-TCP block, the overlying u-HA/PLLA composite plate was fixed to the adjacent bone or to the underlying bone through the β-TCP block using a u-HA/PLLA screw for stability. In our experience, the hard-type β-TCP can be used with Kirschner wires for fixation without breaking.12) Fixation of the hard-type β-TCP using u-HA/PLLA screws that penetrate the block also was possible in the current series. The u-HA/PLLA matrix shows optimal degradative and bioresorptive behavior. The u-HA/PLLA composite has been reported to retain its mechanical strength during the bone healing period.6) There is no need for a second operation to remove the implant. It has been reported that the PLLA matrix of u-HA/PLLA degrades completely after approximately 4.0 to 5.0 years, and almost all of the u-HA particles are replaced by bone tissue after 5.5 years.14) Resorbable materials, such as HA and PLLA, can cause an allergic response or inflammatory reactions in surrounding tissue.151617) In the current series, local symptoms indicative of inflammation were not reported in any cases. However, the slow degradation of the u-HA/PLLA would be unlikely to cause an inflammatory reaction.
For stabilization of implanted β-TCP blocks, the use of bulky metal implants to treat fractured bone requires larger skin incisions, when more delicate implants would be sufficient to stabilize the β-TCP block implantation. In a comparison of the mechanical properties between u-HA/PLLA plates and titanium plates, the bending strength, bending stiffness and torsional strength of one-third or semi-tubular u-HA/PLLA plate constructs has been reported to be comparable with those of titanium plates for 1.5- or 2.0-mm screws. The clinical results in this small series of patients with metacarpal fractures were similar for the u-HA/PLLA plates and titanium plates.18) In addition, the u-HA/PLLA composite of plate and screws appears as stable as titanium mini-plates. The combination of u-HA/PLLA plate and screws can be used in a similar way to titanium mini-plates in orthognathic surgery.19) However, u-HA/PLLA plate and screw fixation is insufficient for a complete defect of the diaphysis in the weight-bearing femur.
In summary, plates and screws made of u-HA/PLLA can be used to stabilize hard-type β-TCP blocks in the reconstruction of bone tumor resections. The u-HA/PLLA is radiolucent; therefore, its presence does not hinder plain radiograph examinations for possible signs of tumor recurrence. Moreover, a CT or MRI examination can resolve u-HA/PLLA materials without artifacts, preserving the ability to assess the lesion, whereas a metal plate and screws would make complete assessment of the lesion difficult because of the artifacts on plain radiographs, CT and/or MRI scans. The u-HA/PLLA materials do not cause artifacts that can interfere with an examination of the lesion at follow-up. The utility of u-HA/PLLA components for reconstructive surgery to treat a bone tumor can extend the application of β-TCP blocks.
Figures and Tables
Fig. 1
Unsintered hydroxyapatite and poly-L-lactide composite (u-HA/PLLA) components for use in bone reconstruction after tumor curettage or resection. (A) Mesh plate and screws. (B) The β-tricalcium phosphate block is stabilized by u-HA/PLLA components.
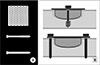
Fig. 2
Chondrosarcoma in the ilium of a 41-year-old male. (A) After en -bloc resection of the lesion, hard-type β-tricalcium phosphate (β-TCP) blocks were implanted and stabilized with the unsintered hydroxyapatite and poly-L-lactide composite plates and screws. Plain radiographs were taken at various times: preoperatively, postoperatively (B), and 16 months after the surgery (C). (D) A computed tomography (CT) scan taken preoperatively shows an irregular calcified lesion at the left posterior ilium. (E, F) At 4 months after surgery, the CT scans show no evidence of dislocation of the implanted β-TCP blocks.

Fig. 3
Parosteal osteosarcoma in the distal femur of a 19-year-old female. (A) Plain radiographs. (B) Computed tomography scans show ossified bony protuberances from the posterior surface of the femur. (C) En-bloc resection was performed and the reconstruction method involved the use of hard-type β-tricalcium phosphate (β-TCP) blocks and the unsintered hydroxyapatite and poly-L-lactide composites. (D) No displacement of the β-TCP blocks was observed and the β-TCP blocks were incorporated into the host bone 21 months after the surgery.
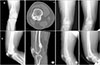
Fig. 4
Giant-cell tumor of bone in the proximal tibia of a 36-year-old male. (A) Plain radiographs. (B) Computed tomography scans show an osteolytic and expansile lesion. (C) Immediate postoperative plain radiographs show reconstruction with a hard-type β-tricalcium phosphate (β-TCP) block. (D) Bone incorporation at the periphery of the β-TCP block is seen 3 months after the operation.

Fig. 5
Chondroblastoma in the proximal tibia of a 16-year-old male. (A) Plain radiographs. (B) Computed tomography scans show an osteolytic lesion with calcification. (C) After curettage, reconstruction was performed with a β-tricalcium phosphate block and unsintered hydroxyapatite and poly-L-lactide composites.

References
1. O'Donnell RJ, Springfield DS, Motwani HK, Ready JE, Gebhardt MC, Mankin HJ. Recurrence of giant-cell tumors of the long bones after curettage and packing with cement. J Bone Joint Surg Am. 1994; 76(12):1827–1833.
2. Sakamoto A. Reconstruction with β-tricalcium phosphate for giant cell tumor of bone around the knee. J Knee Surg. 2017; 30(1):75–77.

3. Sakellariou VI, Mavrogenis AF, Mazis GA, Papagelopoulos PJ. Osteosarcoma of navicular bone: en bloc excision and salvage of the foot. Foot Ankle Surg. 2012; 18(3):e29–e33.

4. Sakamoto M, Matsumoto T. Development and evaluation of superporous ceramics bone tissue scaffold materials with triple pore structure a) hydroxyapatite, b) beta-tricalcium phosphate. In : Tal H, editor. Bone regeneration. London: InTech;2012. p. 301–320.
5. Stone JL, Beaupre GS, Hayes WC. Multiaxial strength characteristics of trabecular bone. J Biomech. 1983; 16(9):743–752.

6. Shikinami Y, Matsusue Y, Nakamura T. The complete process of bioresorption and bone replacement using devices made of forged composites of raw hydroxyapatite particles/poly l-lactide (F-u-HA/PLLA). Biomaterials. 2005; 26(27):5542–5551.

7. Ueki K, Okabe K, Marukawa K, et al. Skeletal stability after mandibular setback surgery: comparison between the hybrid technique for fixation and the conventional plate fixation using an absorbable plate and screws. J Craniomaxillofac Surg. 2014; 42(4):351–355.

8. Yasunaga T, Matsusue Y, Furukawa T, Shikinami Y, Okuno M, Nakamura T. Bonding behavior of ultrahigh strength unsintered hydroxyapatite particles/poly(L-lactide) composites to surface of tibial cortex in rabbits. J Biomed Mater Res. 1999; 47(3):412–419.

9. Furukawa T, Matsusue Y, Yasunaga T, et al. Histomorphometric study on high-strength hydroxyapatite/poly(L-lactide) composite rods for internal fixation of bone fractures. J Biomed Mater Res. 2000; 50(3):410–419.

10. Ng AM, Tan KK, Phang MY, et al. Differential osteogenic activity of osteoprogenitor cells on HA and TCP/HA scaffold of tissue engineered bone. J Biomed Mater Res A. 2008; 85(2):301–312.

11. Liu B, Lun DX. Current application of β-tricalcium phosphate composites in orthopaedics. Orthop Surg. 2012; 4(3):139–144.

12. Sakamoto A. Joint preserved reconstruction after curettage in giant cell tumor of bone arising in the distal radius: case report. Int J Surg Case Rep. 2015; 16:181–183.

13. Sakamoto A. Reconstruction with β-tricalcium phosphate after navicular tumor resection. J Foot Ankle Surg. 2017; 56(1):98–102.

14. Hayashi M, Muramatsu H, Sato M, Tomizuka Y, Inoue M, Yoshimoto S. Surgical treatment of facial fracture by using unsintered hydroxyapatite particles/poly l-lactide composite device (OSTEOTRANS MX(®)): a clinical study on 17 cases. J Craniomaxillofac Surg. 2013; 41(8):783–788.

15. Eppley BL, Morales L, Wood R, et al. Resorbable PLLA-PGA plate and screw fixation in pediatric craniofacial surgery: clinical experience in 1883 patients. Plast Reconstr Surg. 2004; 114(4):850–856.

16. Shikinami Y, Okuno M. Bioresorbable devices made of forged composites of hydroxyapatite (HA) particles and poly-L-lactide (PLLA). Part I: basic characteristics. Biomaterials. 1999; 20(9):859–877.

17. Shikinami Y, Okuno M. Bioresorbable devices made of forged composites of hydroxyapatite (HA) particles and poly L-lactide (PLLA). Part II: practical properties of miniscrews and miniplates. Biomaterials. 2001; 22(23):3197–3211.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download