Abstract
Background and Objectives
The aim of the study is to evaluate the long-term results after a surgical repair of Ebstein's anomaly.
Subjects and Methods
Forty-eight patients with Ebstein's anomaly who underwent open heart surgery between 1982 and 2013 were included. Median age at operation was 5.6 years (1 day-42.1 years). Forty-five patients (93.7%) demonstrated tricuspid valve (TV) regurgitation of less than moderate degree. When the patients were divided according to Carpentier's classification, types A, B, C, and D were 11, 21, 12, and 4 patients, respectively. Regarding the type of surgical treatment, bi-ventricular repair (n=38), one-and-a half ventricular repair (n=5), and single ventricle palliation (n=5) were performed. Of 38 patients who underwent a bi-ventricular repair, TV repairs were performed by Danielson's technique (n=20), Carpentier's technique (n=11), Cone repair (n=4), and TV annuloplasty (n=1). Two patients underwent TV replacement. Surgical treatment strategies were different according to Carpentier's types (p<0.001) and patient's age (p=0.022).
Results
There were 2 in-hospital mortalities (4.2%; 1 neonate and 1 infant) and 2 late mortalities during follow-up. Freedom from recurrent TV regurgitation rates at 5, 10, and 15 years were 88.6%, 66.3%, 52.7%, respectively. TV regurgitation recurrence did not differ according to surgical method (p=0.800). Survival rates at 5, 10, and 20 years were 95.8%, 95.8%, and 85.6%, respectively, and freedom from reoperation rates at 5, 10, and 15 years were 85.9%, 68.0%, and 55.8%, respectively.
Ebstein's anomaly is a rare disorder accounting for approximately 1% of all congenital heart diseases.1) The morphologic defect of Ebstein's anomaly involves the failure of delamination of the tricuspid valve (TV) leaflets, resulting in a wide variety of abnormalities; adherence of the leaflets to the underlying myocardium, apical and posterior displacement of the dilated TV annulus, dilation of the "atrialized" portion of the right ventricle, fenestrations, redundancy, and tethering of the anterior leaflet.2) In addition, associated cardiac malformations are common. An interatrial communication was reported in 80 to 94% of patients, and other additional associated anomalies included bicuspid or atretic aortic valves, pulmonary atresia or hypoplastic pulmonary artery, subaortic stenosis, coarctation, mitral valve prolapse, accessory mitral valve tissue or muscle bands of the left ventricle, ventricular septal defects, and pulmonary stenosis.3) Patients with Ebstein's anomaly also frequently show arrhythmias. Right bundle branch block is one of the common electrocardiographic features.4) There is also an increased incidence of accessory conduction pathways, and these contribute to the development of supraventricular and ventricular tachyarrhythmias.5)6) Clinical symptoms of patients with Ebstein's anomaly are mainly related to cyanosis, right-sided heart failure, and arrhythmias.7) A wide spectrum of symptoms has been described due to the complexity of abnormalities in the anomaly. In 1988, Carpentier and associates classified Ebstein's anomaly according to the degree of leaflet tethering, degree of apical displacement and degree of dilatation of the atrialized right ventricle.8) A variety of surgical methods were introduced in treatment of Ebstein's anomaly. Those treatments included a TV repair or replacement for the principle element in the treatment of Ebstein's anomaly and additional concomitant procedures for the correction of comorbid anomalies (such as ablation of accessory conduction pathways, resection or plication of the atrialized right ventricle, application of bidirectional cavo-pulmonary shunt, and single-ventricle repair for advanced right ventricular dysfunction).9)
The aim of the study was to evaluate the long-term results after a surgical repair of Ebstein's anomaly during the past 30 years.
The study protocol was reviewed by the Institutional Review Board and approved as a minimal risk retrospective study (Approval Number: H-1510-032-710) that did not require individual consent based on the institutional guidelines for waiving consent.
Of 8045 patients who underwent open heart surgery between 1982 and 2013 at Seoul National University Children's Hospital, 48 patients had been diagnosed with Ebstein's anomaly (48/8045, 0.6 %).
The diagnosis of Ebstein's anomaly was based on echocardiography in all patients. Those patients with pulmonary atresia with intact ventricular septum, complex conotruncal abnormalities, and atrioventricular discordance with ventriculoarterial discordance ("corrected transposition") were excluded from the study.
Of 48 patients, 28 patients (58.3%) were female and had a median age of 5.6 years (1 day-42.1 years) at the time the operation was performed; 2 patients were neonates (4.2%), 8 were infants (16.7%), 33 were children (68.8%), and 5 were adults (10.4%). Major preoperative symptoms of the patients were exertional dyspnea (n=24, 50%) and cyanosis (n=24, 50%). Most common associated cardiac anomalies was atrial septal defect (n=40, 83.3%). Arrhythmias were presented in 25 patients (52.1%) preoperatively, and right bundle branch block (n=15, 31.3%) was the most common. Forty-five patients (93.7%) demonstrated tricuspid regurgitation (TR) of greater than moderate degree. When the patients were divided according to Carpentier's classification, types A, B, C, and D were 11 (22.9%), 21 (43.8%), 12 (25.0%), and 4 (8.3%) patients, respectively (Table 1).
The type of surgical treatment was determined by the patient's TV morphology, surgeon's preferences, and allotted time. TV replacement was done in the earliest period. TV repair with Danielson's technique was performed before 2000, Carpentier's technique was performed after 2000, and Cone repair was performed after 2013.
Bi-ventricular repair (n=38), one-and-a half ventricular repair (n=5), and single ventricle palliation (n=5) were performed for surgical treatment of Ebstein's anomaly. Of 38 patients who underwent a bi-ventricular repair, TV repairs were performed by Danielson's technique (n=20), Carpentier's technique (n=11), Cone repair (n=4), and tricuspid annuloplasty (Kay-type annuloplasty) (n=1). Two patients underwent TV replacement. Of 5 patients who underwent a one-and-a-half ventricular repair, TV repairs were performed by Danielson's technique (n=4) and Carpentier's technique (n=1) (Table 2).
Surgical treatment strategies were different according to Carpentier's type (p<0.001); single ventricle repair was more frequently performed in patients with more progressed Carpentier's types such as types C and D. When the patients were divided according to age at operation (≤1 year or >1 year), type of surgical treatment was significantly different (p=0.022); single ventricle repair was completed only in infants (Table 2).
All patients underwent postoperative follow-up examinations before discharge, and also underwent follow-up examinations including a chest X-ray through the outpatient clinic shortly after discharge, and every 6 to 12 months postoperatively thereafter. Postoperative echocardiographic examinations were performed before discharge, and also performed at the outpatient clinic. The latest follow-up echocardiography was performed at median of 9.7 years (1 day to 33.1 years). The patients were interviewed by telephone for confirmation of their condition if the last clinic visit had not been conducted at the scheduled point. Follow-up was completed in 89.6% (43 of 48) of the patients, with a median follow-up duration of 9.6 years (1 day-33.5 years). All clinical follow-ups were completed by March 31, 2015.
Demographic and other patient-related data were obtained from medical records. Follow-up information was obtained from outpatient clinic visits. Data are expressed as median or number of patients (percentage). A p-value of <0.05 was considered statistically significant. Differences in surgical methods according to Carpentier's type or age were analyzed using a linear by linear association method. Difference in the severity of TR before discharge compared to preoperative TR was analyzed using the Wilcoxon signed rank test. Freedom from recurrent TR, survival and freedom from reoperations were estimated by using the Kaplan-Meier method. Differences in TR recurrence according to surgical strategies were analyzed by the log-rank test. Risk factors of death and reoperation were analyzed using Cox's proportional hazard model. Variables including sex, weight, body surface area, age at operation, symptoms, preoperative TR, Carpentier's type, presence of arrhythmias, type of surgery performed, cardiopulmonary bypass time, aortic cross clamp time, and TR before discharge were included in the analyses.
There were 2 in-hospital mortalities (4.2%); one 1-year old female with moderate to severe TR, Carpentier's type B anomaly and atrial septal defect (ASD), which required a TV repair with Carpentier's technique and ASD patch closure, died of low cardiac output postoperatively during the 1st postoperative day. Another 1-day old female with moderate to severe TR, Carpentier's type D anomaly and Rastelli type A atrioventricular septal defect (AVSD) requiring an atrioventricular valvuloplasty, atrial septectomy and pulmonary artery banding at the 1st day of her life, died of low cardiac output syndrome at the 15th postoperative day. Two late mortalities developed during the follow-up; one died of sepsis at 193 months postoperation, and the other died of upper gastrointestinal bleeding at 121 months postoperation. There were a total of 4 postoperative complications due to a complete AV block (n=3) and chylothorax (n=1).
Of the 5 patients who experienced atrial fibrillation or a flutter, a right-sided Maze procedure (n=3) and isthmus cryoablation (n=1) were performed. Of the 4 patients with paroxysmal supraventricular tachycardia, a radiofrequency catheter ablation (RFCA) was done preoperatively in 1 patient (Table 3). All patients revealed a normal sinus rhythm at the last follow-up regardless of antiarrythmic medications.
The degree of preoperative TV regurgitation decreased significantly before discharge in most patients (p<0.001). When the degree of TV regurgitation was compared according to Carpentier's type, TV regurgitation decreased significantly in patients with Carpentier's type A, B, and C (p=0.012, <0.001, and 0.004, respectively) (Fig. 1).
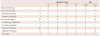
The severity of TV regurgitation tended to progress at the latest follow-up echocardiographic examinations of median 9.71 years. Freedom from recurrent TR rates at 5, 10, and 15 years were 88.6%, 66.3%, and 52.7%, respectively. When the patients were divided according to surgical strategies (Danielson repair, Carpentier repair, and cone repair), no significant difference in recurrent TR was found (Fig. 2).
Thirteen patients underwent reoperations during the follow-up, including 11 reoperations (11/44, 25%) for progressed tricuspid regurgitation or prosthetic TV failure, when single ventricle palliation procedures were excluded from reoperations. Two patients who had a TV replacement (TVR) underwent redo-TVR due to prosthetic valve failure. Among the 4 patients who underwent a one-and-a-half ventricle repair and TV repair with Danielson's technique, 1 patient underwent TVR, and 2 patients underwent redo-tricuspid valve repair with Carpentier's technique. Among the 20 patients who underwent TV repair with Danielson's technique, 2 patients had TVR, 2 patients had TVR with one-and-a-half ventricle repair, and 1 patient had redo-TV repair with Carpentier's technique. One patient who underwent a TV repair with Carpentier's technique had a Cone repair during follow-up. There were 2 patients who required redo-open heart surgery that was not directly related to any previous anomaly; one patient underwent subaortic membrane resection due to left ventricular outlet obstruction caused by subaortic membrane, and the other patient underwent mitral valvuloplasty due to mitral valve regurgitation during follow-up (Table 4).
Six patients underwent 2nd reoperations during the follow-up; 2nd redo-TVR due to prosthetic valve failure in 4 patients, single ventricle palliation with Fontan operation in one patient with TVR and one-and-a-half ventricle repair, and subaortic membrane resection due to recurred subaortic membrane in 1 patient who previously underwent subaortic membrane resection.
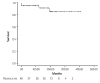
Survival rates for 5, 10, and 20 years were 95.8%, 95.8%, and 85.6%, respectively (Fig. 3). Freedom from reoperation rates for 5, 10, and 15 years were 85.9%, 68.0%, and 55.8%, respectively (Fig. 4). When the risk factors were analyzed using Cox proportional hazard model, we did not find any statistically significant risk factor of death and reoperation, neither by univariate nor multivariable analyses.
The present study revealed 3 main findings. First, Ebstein's anomaly is a rare surgical disorder accounting for approximately 0.6% of all congenital open heart surgery patients at Seoul National University Children's Hospital. Second, surgical treatment strategies in Ebstein's anomaly are decided according to Carpentier's types. Third, survival and freedom from reoperation rates at 10 years were 95.8% and 68.0%, respectively, and approximately 25% patients needed a eredo operation for tricuspid valve during the follow-up.
Ebstein's anomaly is a complex congenital disorder, which encompasses a large spectrum of diseases involving tricuspid valves as well as right ventricular function, and has a prevalence of approximately 1% of all congenital heart diseases.1) One recent study on the Society of Thoracic Surgeons Congenital Heart Surgery Database (STS-CHSD)10) demonstrated low average annual institutional case volumes (median, 1 per year) and high in-hospital mortality in neonatal patients in comparison with infants, children, and adults. In the present study, the incidence of Ebstein's anomaly was similar to a previous report, with 0.6% of all congenital open heart diseases operated at our institution. The goals of surgical treatment of Ebstein's anomaly includes correction of tricuspid valve regurgitation, restoration of right ventricular dysfunction, and treatment of other comorbid cardiac conditions such as arrhythmias. The surgical treatment of Ebstein's anomaly has continually evolved since the initial report of repositioning of the septal and posterior leaflets by Hunter and Lillehei in 1958.11) Hardy and colleagues introduced a technique of plication of an atrialized ventricle.12) Danielson and colleagues modified Hardy's method, which became one of the most frequently used methods in the treatment of Ebstein's anomaly.13) Danielson's technique included transverse plication of the atrialized right ventricle, resulting in a tricuspid valve formed by a single leaflet coapted to the interventricular septum. In 1988, Carpentier et al. reported a new technique with longitudinal plication of the right ventricle and mobilization and repositioning of the tricuspid valve.8) In 1989, da Silva and colleagues developed a new surgical technique called cone reconstruction of the tricuspid valve, aiming at the reconstruction of a valve similar to a normal one.14) Although tricuspid valve repair is preferable to replacement, tricuspid valve replacement is considered when repair is not feasible. In addition, bidirectional cavopulmonary shunt or "one-and-a-half ventricle repair" is performed when the functional capacity of the right ventricle is insufficient to unload right ventricle.15)16) In the present study, a bidirectional cavopulmonary shunt was performed if the patient's right atrial pressure was higher than 15 mmHg after cardiopulmonary bypass weaning.
If patients had severe right ventricular dysfunction, single ventricle repair or Fontan procedures may be the treatment of choice.17) The variety of surgical techniques in treating Ebstein's anomaly represents the enormous anatomic variability that exists. In this study, tricuspid valve replacement rather than repair was performed at the earliest period. Thereafter, tricuspid valve repair using Danielson's technique had been performed. Since 2000, tricuspid valve repair using Carpentier's technique was performed, and since 2013 the Cone repair has been performed. Survival or freedom from reoperation was not statistically related to the types of repair such as bi-ventricular repair versus one-and-a half ventricular repair versus single ventricle palliation. The types of repair were significantly related with Carpentier's type and the patient's age at operation. Single ventricle repair was done in patients with a more progressed disease such as Carpentier's types C and D, or in neonatal patients. Patients who had a more progressed disease or who required surgical correction during the neonatal period probably had a more severe form RV dysfunction; a single ventricle palliation or one-and-a-half ventricular repair was preferred to biventricular repair.
After surgical treatment of Ebstein's anomaly, the severity of TR was significantly decreased in all patients. It tended to progress thereafter, however, and freedom from recurrent TR rates at 5, 10, and 15 years were 88.6%, 66.3%, and 52.7%, respectively. There was no significant difference in the recurrence rate of TR according to surgical strategies although the follow-up duration after cone repair was relatively short and patients who underwent cone repair were relatively small in number. Hence, further follow-up is warranted in order to evaluate differences according to surgical strategies; those who underwent follow-up examinations including chest X-rays and echocardiograms. Because progressive dilatation of the right ventricle and recurrent TR were major concerns for long-term follow up care of patients, a better assessment of TR severity could help with the appropriate selection of patients who would benefit from a subsequent TV repair or replacement.18) Advances in evaluation technologies such as tissue Doppler imaging, speckle tracking echocardiography, and cardiac magnetic resonance imaging were proposed for a better assessment of RV function.19)
One previous study demonstrated that greater severity of Ebstein's anomaly, cardiothoracic ratio of >60%, RVOT obstruction, and presentation as a fetus were associated with poorer survival.20) Another study demonstrated that early age at presentation, hepatomegaly, need for mechanical ventilation and medication, and associated cardiac abnormalities were strongly associated with death.21) However, those results were obtained by analyzing patients who had not been operated on. In the previous study analyzing patients who underwent surgical correction for Ebstein's anomaly, no risk factors were identified for late mortality after surgery.22) In the present study, no statistically significant risk factors of death and reoperation were found. These findings, however, might be related to the small number of patients enrolled in the study.
One of the major comorbidities of Ebstein's anomaly is arrhythmia. One previous study showed that arrhythmia associated with Ebstein's anomaly substantially improved after conservative surgical intervention.23) On the contrary, another study demonstrated that concomitant antiarrhythmic procedures resulted in excellent freedom from recurrence of arrhythmias.24) In the present study, all the patients revealed normal sinus rhythm at the last follow-up, suggesting that the result of resolution of arrhythmia was excellent after surgical repair of Ebstein's anomaly, with or without concomitant anti-arrhythmic procedures. Therefore, further studies are warranted in order to reveal the efficacy of concomitant antiarrythmic procedures.
The present study showed that survival rates at 5, 10, and 20 years after surgery for Ebstein's anomaly were 95.8%, 95.8%, and 85.6%, respectively, and freedom from reoperation rates for 5, 10, and 15 years were 85.9%, 68.0%, and 55.8%, respectively. These results were similar to previous studies demonstrating the survival and freedom from reoperation rates.22)25)
There are limitations of the study that must be recognized. First, the study was a retrospective study. Second, relatively small patients were included in the study, although we collected data of more than 30 years. Third, patients included in the study had heterogenous characteristics and various surgical strategies in the treatment of Ebstein's anomaly.
In conclusion, surgical treatment of Ebstein's anomaly showed favorable long-term results despite anatomic and clinical complexities. Further follow-up is warranted in order to evaluate differences according to surgical strategy.
Figures and Tables
 | Fig. 1Comparison of severity of TR. Number of patients according to the severity of TR before and after the repair is shown in graph. The severity of TR was also compared according to the Carpentier's type. TR: tricuspid regurgitation. |
 | Fig. 2Kaplan-Meier estimated overall freedom from recurrent TR (A). Freedom from recurrent TR rates at 5, 10, and 15 years were 88.6%, 66.3%, and 52.7%, respectively. Kaplan-Meier estimated freedom from recurrent TR according to surgical strategies (B). Log-rank test showed no significant difference in recurrent TR rates between surgical strategies (Danielson repair, Carpentier repair, and cone repair). TR: tricuspid regurgitation. |
 | Fig. 4Kaplan-Meier estimated freedom from reoperations after initial surgical repair of Ebstein's anomaly. |
Table 1
Preoperative characteristics

Table 2
Surgical treatment of patients with Ebstein's anomaly
References
1. Attenhofer Jost CH, Connolly HM, Edwards WD, Hayes D, Warnes CA, Danielson GK. Ebstein's anomaly - review of a multifaceted congenital cardiac condition. Swiss Med Wkly. 2005; 135:269–281.
2. Krieger EV, Valente AM. Diagnosis and management of ebstein anomaly of the tricuspid valve. Curr Treat Options Cardiovasc Med. 2012; 14:594–607.
3. Attenhofer Jost CH, Connolly HM, Dearani JA, Edwards WD, Danielson GK. Ebstein's anomaly. Circulation. 2007; 115:277–285.
4. Huang CJ, Chiu IS, Lin FY, et al. Role of electrophysiological studies and arrhythmia intervention in repairing Ebstein's anomaly. Thorac Cardiovasc Surg. 2000; 48:347–350.
5. Iturralde P, Nava S, Sálica G, Medeiros A, et al. Electrocardiographic characteristics of patients with Ebstein's anomaly before and after ablation of an accessory atrioventricular pathway. J Cardiovasc Electrophysiol. 2006; 17:1332–1336.
6. Khositseth A, Danielson GK, Dearani JA, Munger TM, Porter CJ. Supraventricular tachyarrhythmias in Ebstein anomaly: management and outcome. J Thorac Cardiovasc Surg. 2004; 128:826–833.
7. Paranon S, Acar P. Ebstein's anomaly of the tricuspid valve: From fetus to adult. Heart. 2008; 94:237–243.
8. Carpentier A, Chauvaud S, Macé L, et al. A new reconstructive operation for ebstein's anomaly of the tricuspid valve. J Thorac Cardiovasc Surg. 1988; 96:92–101.
9. Stulak JM, Dearani JA, Danielson GK. Surgical management of ebstein's anomaly. Semin Thorac Cardiovasc Surg Pediatr Card Surg Ann. 2007; 10:105–111.
10. Davies RR, Pasquali SK, Jacobs ML, Jacobs JJ, Wallace AS, Pizarro C. Current spectrum of surgical procedures performed for Ebstein's malformation : An analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. Ann Thorac Surg. 2013; 96:1703–1710.
11. Hunter SW, Lillehei CW. Ebstein's malformation of the tricuspid valve: Study of a case together with suggestion of a new form of surgical therapy. Dis Chest. 1958; 33:297–304.
12. Hardy K, May IA, Webster CA, Kimball KG. Ebstein's anomaly: A functional concept and successful definitive repair. J Thorac Cardiovasc Surg. 1964; 48:927–940.
13. Danielson GK, Driscoll DJ, Mair DD, Warnes CA, Oliver WC Jr. Operative treatment of ebstein's anomaly. J Thorac Cardiovasc Surg. 1992; 104:1195–1202.
14. Silva JP, Baumgratz JF, Fonseca Ld, et al. Ebstein's anomaly: Results of the conic reconstruction of the tricuspid valve. Arq Bras Cardiol. 2004; 82:212–216.
15. Oxenius A, Attenhofer Jost CH, Prêtre R, et al. Management and outcome of Ebstein's anomaly in children. Cardiol Young. 2013; 23:27–34.
16. Raju V, Dearani JA, Burkhart HM, et al. Right ventricular unloading for heart failure related to Ebstein malformation. Ann Thorac Surg. 2014; 98:167–174. discussion 173-4.
17. Jaquiss RD, Imamura M. Management of Ebstein's anomaly and pure tricuspid insufficiency in the neonate. Semin Thorac Cardiovasc Surg. 2007; 19:258–263.
18. Muraru D, Surkova E, Badano LP. Current trends in the diagnosis and management of functional tricuspid regurgitation. Korean Circ J. 2016; 46:e101.
19. Cheung YF. Functional assessment for congenital heart disease. Korean Circ J. 2014; 44:59–73.
20. Celermajer DS, Bull C, Till JA, et al. Ebstein's anomaly: Presentation and outcome from fetus to adult. J Am Coll Cardiol. 1994; 23:170–176.
21. Kapusta L, Eveleigh RM, Poulino SE, et al. Ebstein's anomaly: factors associated with death in childhood and adolescence: a multi-centre, long-term study. Eur Heart J. 2007; 28:2661–2666.
22. Boston US, Dearani JA, O'Leary PW, Driscoll DJ, Danielson GK. Tricuspid valve repair for Ebstein's anomaly in young children: a 30-year experience. Ann Thorac Surg. 2006; 81:690–696. discussion 695-6.
23. Chauvaud SM, Brancaccio G, Carpentier AF. Cardiac arrhythmia in patients undergoing surgical repair of ebstein's anomaly. Ann Thorac Surg. 2001; 71:1547–1552.
24. Khositseth A, Danielson GK, Dearani JA, Munger TM, Porter CJ. Supraventricular tachyarrhythmias in Ebstein anomaly: management and outcome. J Thorac Cardiovasc Surg. 2004; 128:826–833.
25. Brown ML, Dearani JA, Danielson GK, et al. The outcomes of operations for 539 patients with ebstein anomaly. J Thorac Cardiovasc Surg. 2008; 135:1120–1136.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download