Abstract
Objective
To evaluate the efficacy of loop electrosurgical excision procedure (LEEP) combined with cold coagulation for treating cervical intraepithelial neoplasia (CIN).
Methods
We reviewed clinic-pathologic data of 498 patients treated with LEEP alone (n=354), and LEEP combined with cold coagulation (n=144) between January 2000 and December 2011. After LEEP, we followed up all patients by using Papanicolaou smear and human papillomavirus (HPV) test, and evaluated abnormal cervical cytology-free interval and high-risk HPV infection-free interval. Moreover, we investigated independent factors affecting abnormal cervical cytology or high-risk HPV infection after LEEP.
Results
Abnormal cervical cytology-free interval was longer in patients treated with LEEP combined with cold coagulation than in those treated with LEEP alone (mean, 92.4 vs. 84.4 months; P=0.01), and patients treated with LEEP combined with cold coagulation also showed longer high-risk HPV infection-free interval than those treated with LEEP alone (mean, 87.6 vs. 59.1 months; P=0.01). Moreover, CIN 3 and cold coagulation were factors affecting abnormal cervical cytology after LEEP (adjusted hazard ratios, 1.90 and 0.61; 95% confidence intervals, 1.27 to 2.84 and 0.39 to 0.96), and CIN 3, positive deep cervical margin and cold coagulation were also factors affecting high-risk HPV infection after LEEP (adjusted hazard ratios, 2.07, 4.11, and 0.64; 95% confidence intervals, 1.38 to 3.08, 1.63 to 10.39, and 0.43 to 0.96). When we performed subgroup analyses for patients with CIN 2 or CIN 3, the result were similar.
Cervical intraepithelial neoplasia (CIN) is a precancerous lesion, which can be treated effectively before the transition to cervical cancer [1]. In particular, excisional procedures including loop electrosurgical excision procedure (LEEP) is well known for the diagnosis and treatment of CIN [12]. Moreover, ablative methods such as laser ablation, cryotherapy and cold coagulation are also known to be effective for treating CIN [3]. Among them, cold coagulation has been used to destroy an abnormal transformation zone, and thereby to treat non-invasive cervical lesions since 1996 [4]. Although cold coagulation has some advantages such as less pain requiring minimal analgesia, short time for treatment and rare complications [5], it is not used widely anymore since the introduction of LEEP providing histologic information.
However, the resection margin status after LEEP is still important because residual dysplastic cells can increase the risk of disease recurrence and progression to invasive cancer [678910]. Thus, repeated conization is considered whenever resection margin of specimen is positive after LEEP for obtaining specimen without residual dysplastic cells [11]. Nevertheless, repeated conization is discouraged for young women who want pregnancy because it increase the risk of preterm birth [1213], and for women who show no residual cervix because repeated conization increases post-procedure complications such as vesicovaginal fistula [14].
Thus, LEEP combined with cold coagulation has been suggested for treating CIN more effectively in previous studies [1516]. In these studies, cold coagulation was expected to eliminate residual dysplastic cells on the resection margin after LEEP if present [17]. In the current study, we also performed a two center cohort study to compare the efficacy between LEEP combined with cold coagulation and LEEP alone for treating CIN and reducing the risk of abnormal cervical cytology or high-risk HPV infection after the treatment.
We collected clinico-pathologic data of patients who underwent LEEP at Seoul National University Hospital and Seoul National University Bundang Hospital between January 2000 and December 2011. The current study was approved by the Institutional Review Board in advance. We included patients as following: those with CIN on punch biopsy or suspicious lesion which cannot be excluded by colposcopy; those who underwent LEEP combined with cold coagulation or LEEP alone. However, we excluded patients who underwent repeated conization or hysterectomy within one year, and those diagnosed with invasive cervical cancer on final pathologic reports.
In the current study, cold coagulation was performed to minimize hemorrhagic complications after LEEP. In detail, we used the cone probe of a Semm Cold Coagulator (Wisap, Sauerlach, Germany). The probe was heated to 120℃, and then applied for about 20 seconds immediately after LEEP. For patients who showed bleeding again within one month, cold coagulation was applied repetitively for controlling bleeding completely. After LEEP combined with cold coagulation or LEEP alone, we followed up all patients by using Papanicolaou smear and human papillomavirus (HPV) test, and evaluated abnormal cervical cytology-free interval and high-risk HPV infection-free interval after the treatment.
We compared clinico-pathologic characteristics between patients treated with LEEP combined cold coagulation, and those treated with LEEP alone using chi-square or Fisher's exact test. We compared abnormal cervical cytology-free interval and high-risk HPV infection-free interval between the two treatments using Kaplan-Meier analysis with the log-rank test. Moreover, we investigated independent factors affecting abnormal cervical cytology or high-risk HPV infection after LEEP, using Cox's proportional hazard analysis including hazard ratio (HR) and 95% confidence interval (CI). For these analyses, we used IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA), and a P<0.05 was considered statistically significant.
Among a total of 498 patients, 354 underwent LEEP alone while 144 received LEEP combined with cold coagulation. Table 1 shows clinico-pathologic characteristics of all patients. LEEP combined with cold coagulation was performed more frequently in patient with low-grade CIN, compared with those treated with LEEP alone. However, there were no differences in age and resection margin status between the two groups. Abnormal cervical cytology-free interval was longer in patients treated with LEEP combined with cold coagulation than in those treated with LEEP alone (mean, 92.4 vs. 84.4 months; P=0.01), and patients treated with LEEP combined with cold coagulation also showed longer high-risk HPV-free interval than those treated with LEEP alone (mean, 87.6 vs. 59.1 months; P=0.01) (Fig. 1A). When we performed subgroup analyses for patients with CIN 2 or CIN 3, abnormal cervical cytology-free interval was also longer in patients treated with LEEP combined with cold coagulation than in those treated with LEEP alone (mean, 92.3 vs. 76.7 months; P=0.01), and patients treated with LEEP combined with cold coagulation also showed longer high-risk HPV-free interval than those treated with LEEP alone (mean, 87.8 vs. 54.7 months; P<0.01) (Fig. 1B).
When we investigated factors affecting abnormal cervical cytology after LEEP, CIN 3 and cold coagulation were meaningful in the univariate (HRs, 1.56 and 0.75; 95% CIs, 1.08 to 2.26 and 0.49 to 0.85), and the multivariate analyses (adjusted HRs, 1.90 and 0.61; 95% CIs, 1.27 to 2.84 and 0.39 to 0.96) (Table 2). For only patients with CIN 2 or CIN3, cold coagulation were the only factor affecting abnormal cervical cytology after LEEP in the univariate analysis (HR, 0.52; 95% CI, 0.31 to 0.91), whereas CIN 3 and cold coagulation were significant in the multivariate analysis (adjusted HRs, 1.65 and 0.55; 95% CIs, 1.03 to 2.64 and 0.31 to 0.96) (Table 2).
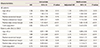
Furthermore, CIN 3, positive deep cervical margin and cold coagulation were factors affecting high-risk HPV infection after LEEP in the univariate (HRs, 1.51, 3.36 and 0.82; 95% CIs, 1.06 to 2.16, 1.37 to 8.24, and 0.56 to 0.79), and the multivariate analyses (adjusted HRs, 2.07, 4.11, and 0.64; 95% CIs, 1.38 to 3.08, 1.63 to 10.39, and 0.43 to 0.96) (Table 3). For patients with CIN 2 or CIN 3, CIN 3 and cold coagulation were significant in the univariate analysis (HRs, 1.89 and 0.75; 95% CIs, 1.24 to 2.89 and 0.46 to 0.92), whereas CIN 3, positive deep cervical margin and cold coagulation were factors affecting high-risk HPV infection after LEEP in the multivariate analysis (adjusted HRs, 2.25, 2.78, and 0.59; 95% CIs, 1.45 to 3.51, 1.15 to 6.71, and 0.56 to 0.990) (Table 3).
In the current study, we found that cold coagulation increased abnormal cervical cytology-free interval and high-risk HPV infection-free interval, and it played a role as a factor reducing abnormal cervical cytology or high-risk HPV infection after LEEP. These results suggest that cold coagulation may contribute to the removal of residual dysplastic cells in patients with CIN who received LEEP. However, there are some limitations as follows in the current study. First, a small number of patients led to few number of histologic recurrence after LEEP, which decreased statistical power for obtaining these results. It is the reason why we used abnormal cervical cytology-free interval and high-risk HPV infection-free interval as a clinical outcome because abnormal cervical cytology or high-risk HPV infection occurred more frequently after LEEP than histologic recurrence. Second, LEEP combined with cold coagulation was used in patients with relatively low-grade CIN, compared with those treated with LEEP alone. In particular, some patients with abnormal cervical cytology or high-risk HPV infection were also included because colposcopic finding could not rule out CIN. This fact can act as a bias in this setting including a small number of patients. Third, we could not evaluated the disadvantage of cold coagulation such as cervical stenosis due to the retrospective design.
However, the finding that CIN 3 was a factor affecting abnormal cervical cytology or high-risk HPV infection after LEEP is meaningful in the current study. The similar result was reported in previous studies [1618]. It means that patients with high-grade CIN may have more chance of high-risk HPV infection, and subsequent cellular dysplasia. Moreover, positive resection margin increased the risk of high-risk HPV infection after LEEP, whereas it was not related with the increased risk of abnormal cervical cytology. In spite of few evidences supporting this finding, we could explain it as follows.
In the current study, we applied cold coagulation for controlling bleeding after LEEP like a previous study [16]. The reason is that the incidence of complicated bleeding may be 1% in patients treated with LEEP combined with cold coagulation, whereas it occurs 2% to 2.6% after LEEP alone [31619]. Thus, it is possible that the application time of the probe heated to 120℃ was not enough to kill cells infected with high-risk HPV, although most of residual dysplastic cells were removed during cold coagulation after LEEP. Thus, positive resection margin has more chance to include hidden cells infected with high-risk HPV after cold coagulation, and this hypothesis can be indirectly supported by a previous study where post-treatment HPV test was more useful during the follow-up after cervical conization than a Pap smear [20].
In literature review, cold coagulation after LEEP has been also reported to decrease the risk of abnormal cervical cytology, supporting the results from the current study. Previous studies showed that the risk of abnormal cervical cytology was about 1% and 4.2% to 16.7% at 6 and 12 months after LEEP combined with cold coagulation. Nevertheless, it increased 2.6% to 7.6% and 9.3% to 10.3% at 6 and 12 months after LEEP alone [161721]. These findings emphasize that cold coagulation may decrease the risk of abnormal cervical cytology effectively after LEEP.
In conclusion, the current study suggests that cold coagulation after LEEP may be effective to decrease abnormal cervical cytology and high-risk HPV infection in comparison with LEEP alone. Moreover, cold coagulation can give an additional advantage that it is efficient to control bleeding after LEEP easily. However, the effect of cold coagulation for reducing the risk of histologic recurrence should be further investigated in large-scale prospective cohort studies in the future.
Figures and Tables
 | Fig. 1Comparison of abnormal cervical cytology-free interval and high-risk human papillomavirus infection-free interval between loop electrosurgical excision procedure (LEEP) combined with cold coagulation and LEEP alone in (A) all patients and (B) patient with cervical intraepithelial neoplasia 2 or 3. |
Table 1
Clinico-pathologic characteristics
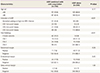
Table 2
Cox's proportional hazard analysis for factors affecting abnormal cervical cytology after loop electrosurgical excision procedure
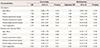
Table 3
Cox's proportional hazard analysis for factors affecting high-risk human papillomavirus infection after loop electrosurgical excision procedure
Acknowledgments
This research was supported by grants (no. 04-2012-0890, 03-2012-0170, 23-2015-0180, and 23-2015-0140) from the Seoul National University Hospital research fund and the Korean Health Technology R&D Project, Ministry of Health and Welfare (HI14C2404).
References
1. Lindeque BG. Management of cervical premalignant lesions. Best Pract Res Clin Obstet Gynaecol. 2005; 19:545–561.
2. Ahlgren M, Ingemarsson I, Lindberg LG, Nordqvist RB. Conization as treatment of carcinoma in situ of the uterine cervix. Obstet Gynecol. 1975; 46:135–139.
3. Wright TC Jr, Gagnon S, Richart RM, Ferenczy A. Treatment of cervical intraepithelial neoplasia using the loop electrosurgical excision procedure. Obstet Gynecol. 1992; 79:173–178.
4. Loobuyck HA, Duncan ID. Destruction of CIN 1 and 2 with the Semm cold coagulator: 13 years' experience with a see-and-treat policy. Br J Obstet Gynaecol. 1993; 100:465–468.
5. Kang WD, Ju UC, Kim SM. A human papillomavirus (HPV)-16 or HPV-18 genotype is a reliable predictor of residual disease in a subsequent hysterectomy following a loop electrosurgical excision procedure for cervical intraepithelial neoplasia 3. J Gynecol Oncol. 2016; 27:e2.
6. Roman LD, Felix JC, Muderspach LI, Agahjanian A, Qian D, Morrow CP. Risk of residual invasive disease in women with microinvasive squamous cancer in a conization specimen. Obstet Gynecol. 1997; 90:759–764.
7. Gonzalez DI Jr, Zahn CM, Retzloff MG, Moore WF, Kost ER, Snyder RR. Recurrence of dysplasia after loop electrosurgical excision procedures with long-term follow-up. Am J Obstet Gynecol. 2001; 184:315–321.
8. Murdoch JB, Morgan PR, Lopes A, Monaghan JM. Histological incomplete excision of CIN after large loop excision of the transformation zone (LLETZ) merits careful follow up, not retreatment. Br J Obstet Gynaecol. 1992; 99:990–993.
9. Shafi MI, Dunn JA, Buxton EJ, Finn CB, Jordan JA, Luesley DM. Abnormal cervical cytology following large loop excision of the transformation zone: a case controlled study. Br J Obstet Gynaecol. 1993; 100:145–148.
10. Gardeil F, Barry-Walsh C, Prendiville W, Clinch J, Turner MJ. Persistent intraepithelial neoplasia after excision for cervical intraepithelial neoplasia grade III. Obstet Gynecol. 1997; 89:419–422.
11. Mota F. Microinvasive squamous carcinoma of the cervix: treatment modalities. Acta Obstet Gynecol Scand. 2003; 82:505–509.
12. Mathevet P, Dargent D, Roy M, Beau G. A randomized prospective study comparing three techniques of conization: cold knife, laser, and LEEP. Gynecol Oncol. 1994; 54:175–179.
13. Andersen ES, Nielsen K, Larsen G. Laser conization: follow-up in patients with cervical intraepithelial neoplasia in the cone margin. Gynecol Oncol. 1990; 39:328–331.
14. Park KE, Ku SY, Kim HS, Kwak C, Kim SH, Choi YM, et al. Vesicovaginal fistula following large-loop excision of the transformation zone in a chronic systemic glucocorticoid user. J Obstet Gynaecol Res. 2011; 37:1459–1462.
15. Bar-Am A, Daniel Y, Ron IG, Niv J, Kupferminc MJ, Bornstein J, et al. Combined colposcopy, loop conization, and laser vaporization reduces recurrent abnormal cytology and residual disease in cervical dysplasia. Gynecol Oncol. 2000; 78:47–51.
16. Allam M, Paterson A, Thomson A, Ray B, Rajagopalan C, Sarkar G. Large loop excision and cold coagulation for management of cervical intraepithelial neoplasia. Int J Gynaecol Obstet. 2005; 88:38–43.
17. Baggish MS, Dorsey JH. Carbon dioxide laser for combination excisional-vaporization conization. Am J Obstet Gynecol. 1985; 151:23–27.
18. Paraskevaidis E, Kalantaridou SN, Paschopoulos M, Zikopoulos K, Diakomanolis E, Dalkalitsis N, et al. Factors affecting outcome after incomplete excision of cervical intraepithelial neoplasia. Eur J Gynaecol Oncol. 2003; 24:541–543.
19. Herzog TJ, Williams S, Adler LM, Rader JS, Kubiniec RT, Camel HM, et al. Potential of cervical electrosurgical excision procedure for diagnosis and treatment of cervical intraepithelial neoplasia. Gynecol Oncol. 1995; 57:286–293.
20. Houfflin Debarge V, Collinet P, Vinatier D, Ego A, Dewilde A, Boman F, et al. Value of human papillomavirus testing after conization by loop electrosurgical excision for high-grade squamous intraepithelial lesions. Gynecol Oncol. 2003; 90:587–592.
21. Yi KH, Jeon YS, Kim BT, Kim JH, Kim BG, Park SY, et al. The efficacy of combination of cold-knife conization and cold-coagulation for diagnosis and treatment of the cervical intraepithelial neoplasia. Korean J Obstet Gynecol. 1997; 40:1990–1998.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download