Abstract
Background
The primary objective of this meta-analysis is aimed at determining whether β-lactams prolonged infusion in patients with nosocomial pneumonia (NP) results in higher cure rate and improved mortality compared to intermittent infusion.
Materials and Methods
Relevant studies were identified from searches of MEDLINE, EMBASE, and CENTRAL from inception to September 1st, 2015. All published articles which evaluated the outcome of extended/continuous infusion of antimicrobial therapy versus intermittent infusion therapy in the treatment of NP were reviewed.
Results
A total of ten studies were included in the analysis involving 1,051 cases of NP. Prolonged infusion of β-lactams was associated with higher clinical cure rate (OR 2.45, 95% CI, 1.12, 5.37) compared to intermittent infusion. However, there was no significant difference in mortality (OR 0.85, 95% CI 0.63–1.15) between the two groups. Subgroup analysis for β-lactam subclasses and for severity of illness showed comparable outcomes.
Nosocomial pneumonia (NP) is one of the frequent hospital acquired infections with an incidence ranging from 6 to 52% [12]. It remains associated with increased mortality rates and high health care costs [3]. Despite our better understanding of the mechanisms underlying NP, successful treatment of these patients remains a difficult and complex undertaking as it is influenced by various factors such as lack of a gold standard for definitive diagnosis of NP, difficulty in differentiating colonization from active infection, frequent association with multidrug resistant pathogens, and altered pharmacokinetics in critically ill patients [4].
Successful management of antimicrobial therapy in cases of NP hinges on prescribing appropriate initial empiric therapy, maximizing antimicrobial pharmacokinetics and/or pharmacodynamics (PK/PD) profiles, and administering a short course of treatment. Beta-lactams, when administered at doses commonly used in NP, exhibit time dependent killing. The extent of bacterial death is correlated with the percent of the dosing interval that drug concentrations are maintained above the minimum inhibitory concentration (MIC) of the pathogen. In these instances, pharmacokinetic modeling and dosing simulations showed that pharmacodynamics targets were better achieved by extended or continuous infusion of beta-lactams [567]. Several meta-analyses have examined the comparison between extended or continuous versus short term infusion on clinical outcomes with conflicting results [8910]. Inclusion of crossover studies and trials with small number of participants may have obscured clinical benefits. No prior meta-analysis, to our knowledge, has examined the clinical efficacy of extended infusion in patients with NP. The constant and sustainable antibiotic concentrations provided by extended or continuous infusion are particularly important for pathogens with high MIC values commonly observed in these settings. We performed a systematic review and meta-analysis of published clinical investigations investigating the efficacy of prolonged infusion beta-lactam therapy compared with intermittent infusion beta-lactam therapy with regards to mortality and clinical cure in patients with NP. The primary objective was to determine if prolonged infusion of beta-lactam antibiotics resulted in improved patient survival and clinical cure compared to intermittent dosing of beta-lactam antibiotics.
An internet search was performed using MEDLINE, EMBASE and CINAHL from inception to September 1st, 2015 to identify all published articles which evaluated the outcome of extended/continuous infusion of antimicrobial therapy versus intermittent infusion therapy in the treatment of NP. The electronic search strategy included the terms "infusion", "extended", "prolonged", "continuous", "intermittent", "nosocomial", "ventilator-associated pneumonia", and "outcome". Terms were "exploded" and combined by using Boolean operators where appropriate. We also searched the reference lists of original reports and systematic review of studies involving NP to identify studies not yet included in the computerized databases. In addition, we reviewed the cited lists of eligible trials by Google Scholar to ensure that all appropriate studies were included. Case reports and case series including <10 patients were excluded. No language restrictions were applied.
Articles were identified in a staged process whereby titles were initially screened for potential eligibility by a single reviewer (PJ). Abstracts and full texts of those potentially eligible were then assessed by two reviewers (HES and AL) independently and were included if the comparative outcomes included patients treated with "extended or continuous" versus "short term or intermittent" infusion. For the purpose of the review, patients were allocated in 2 groups: the "prolonged infusion" group that included patients receiving either extended infusions of a beta-lactam lasting ≥3 hours or a 24-hour continuous infusion, and the "short-term infusion" group comprising patients receiving short-term intermittent drug regimens (ie, 20–60 minutes infusion). In cases where the same population studied was analyzed in more than one publication, the study's results were accounted for only once.
Two reviewers independently extracted the data. In case of disagreement between the two reviewers, a third reviewer extracted the data. Trial authors were contacted for clarification and to complete missing data. We assessed the methodologic quality of observational studies with the Newcastle-Ottawa Scale [11] and that of randomized controlled trials with the Jadad scale [12]. We collected the raw, unadjusted number of deaths among patients given prolonged infusion versus intermittent antibiotic treatment. We collected descriptive data on setting, study years, follow-up duration, patient characteristics, severity of illness, types of pathogens, antimicrobial agents and clinical and microbiological outcomes, emergence of resistance, adverse events and mortality.
The primary outcomes of the review were all-cause mortality and clinical cure at the end of the treatment. When data regarding outcomes were not provided, outcomes at test-of cure visit were used. Clinical cure was defined by the discretion of the authors of the publication because of the heterogeneous nature of the study population, and pathogens involved. If only clinical failure was reported, it was assumed that clinical success was achieved in all those patients who did not fail treatment.
Data were analyzed with the use of the Review Manager (RevMan version 5.3; Cochrane Collaboration, Oxford, UK). Statistical heterogeneity was assessed by employing both the χ2 test and I2 statistic; a χ2 test's P value lower than 0.10 and an I2 value higher than 50% were defined to note statistical significance. When P was higher than 0.10 and I2 was lower than 50% (i.e., statistically non-significant heterogeneity), pooled odds ratios (ORs) and 95% confidence intervals (CIs) for all outcomes were calculated by using both the Mantel-Haenszel fixed effect and the DerSimonian-Laird random effects models. This was done because the possible persistence of the statistical significance of our results even after the implementation of the conservative random effects model (along with the fixed effect model) presumably adds to the robustness of our findings. When χ2 test's P was lower than 0.10 and I2 was higher than 50% (i.e., statistically significant heterogeneity), OR and CI were calculated by using only the random effects model. Subgroup analysis were carried out by type of study design, β-lactam subclasses, and by severity of illness determined by the Acute Physiology and Chronic Health Evaluation (APACHE) II score. Small study effect was detected by the funnel plot method using Egger's test; a P-value lower than 0.05 denotes statistical significance.
We identified 3261 potentially relevant published articles on review of MEDLINE, EMBASE, and CINHAL (Fig. 1). After removing 237 duplicates, 3,024 titles and abstracts were reviewed by two independent study team members. The majority of studies were excluded during initial screening because they were Monte Carlo simulation studies that did not involve patients, or were studies that did not have a comparator group. Thirty-four studies underwent full text review and 10 met criteria for inclusion [13141516171819202122] comprising 1,051 patients treated. Figure 1 shows the selection process of studies included in the meta-analysis.
The characteristics of the eligible studies are presented in Table 1. Four studies were retrospective [16171820], one was prospective, parallel, non-randomized [22] and 5 randomized controlled trials (RCT)s [1315192122]. The selected studies were performed on 4 continents (USA, Europe, Asia, and Australia) and included patients from medical, surgical, and mixed ICUs. All but two of the RCTs and all non RCTs were from a single center. Study sample sizes varied from 20 to 531. A mean/median APACHE II score ≥ 15 was observed in 6 studies (60%). Gram negative organisms were the predominant pathogens in all selected studies.
Table 2 depicts the β-lactam antibiotic, dose and infusion schedule for each study. β-lactam antibiotics included cephalosporins [13141517], carbapenems [16192021] and piperacillin/tazobactam [1822]. In the experimental arm, these agents were administered via either continuous infusion [131416171821] or extended infusion [15192022]. In five of the six studies utilizing a continuous infusion of β-lactam delivery, a loading dose was administered initially to ensure that the time to maximum concentration of the drug is reached rapidly. Participants received additional non β-lactam antibiotics in 6 studies [141516171923]. The medication in the study arms differed in one trial in which doripenem was compared to imipenem [19]. Because of the similar antimicrobial profile of these agents, this study was included. In several studies, β-lactam dosing was adjusted for renal insufficiency [1419].
The quality of RCTs selected in this study was moderate. Whilst randomization procedure was in place, few studies reported in detail randomization procedures and allocation concealment. Furthermore, none of the investigators were blinded to the mode of delivery. Non RCTs studies were of low to moderate quality. Several studies had a historic control design that compared patients receiving prolonged/continuous infusion with historical cohorts who were administered intermittent boluses per protocol implementation.
Six studies reported mortality as outcome (Fig. 2). Among the 368 patients enrolled in the continuous/extended infusion, there were 57 deaths compared to 69 deaths among the 377 in the intermittent infusion. The difference was not statistically significant with OR of 0.85 (95% CI 0.63–1.15). There was no significant heterogeneity among the identified studies evaluating mortality (I2 = 0). Visual inspection of the funnel plot comparing the effect measure for the primary outcome of mortality for each study with its precision did not suggest asymmetry (Fig. 3). Overall, based on qualitative and quantitative exploration, no conclusive evidence of reporting bias was found.
Pooling the outcomes of the eight studies that reported on clinical success showed that clinical cure was higher among patients who received extended or continuous infusion of a carbapenem, cephalosporin, or piperacillin/tazobactam than those who received intermittent (OR = 2.45 [95% CI, 1.12, 5.37]) (Fig. 4). Proportion of clinical cure ranged from 33% to 100%. There was significant heterogeneity among the selected studies evaluating clinical cure (I2 = 75%, P < 0.001). This is likely due to the varied definitions of clinical success among the studies. In the subgroup analysis (Table 3), no significant differences were noted by study design or β-lactam subclasses. However, clinical cure was higher in pneumonia patients receiving prolonged infusion with APACHE II score ≥ 15 versus intermittent infusion (OR 3.45, 95% CI 1.08–11.01).
Only two studies presented data on microbiologic cure rate [1519]. There was significant overlap in the microbiological isolates seen in both studies. The proportion of patients in the microbiologically evaluable cohorts ranged from 59.3% to 79.9% of the entire sample size. There was no statistical heterogeneity with respect to results (I2 = 0). Although the point estimate for the pooled OR favored extended/continuous infusion over intermittent infusion this difference was not statistically significant (OR for cure, 1.50; 95% CI, 0.89–2.52).
Four studies reported on adverse events during antibiotic administration [14151921]. None were associated with mortality. Three cases of nephrotoxicity were reported in patients receiving ceftazidime (two in the intermittent infusion group and one in the continuous infusion group) [14]. These were attributed to concomitant tobramycin administration. C. difficile were described also in three patients who were treated successfully with oral metronidazole. In one study [19], seizures were more commonly observed in patients receiving imipenem (3.8%) than doripenem infusion (1.1%). Although the majority of these events occurred in patients with underlying brain injury or prior history of epilepsy, all but one did not appear related to study drug therapy. Gastrointestinal manifestations were minor and included nausea, vomiting, diarrhea, and transient elevation in liver enzymes. No significant differences between the study arms were discerned for each of the aforementioned adverse events.
The first publication using continuous infusion as a method to administer β-lactam drugs to endocarditis patients dates back more than 65 years [24]. Since then there is growing evidence on the theoretical advantage of continuous β-lactam application, as a way to optimize the dose regimen and pharmacokinetics without increasing patient's drug exposure [25]. This review showed that there were significant clinical advantages associated with continuous and extended infusion of β-lactam in hospitalized patients with NP. Compared with intermittent boluses, prolonged infusion was associated with a higher clinical cure rate and a trend toward reduction in mortality.
Several meta-analyses have been conducted on this topic [8926272829] with inconsistent results. These studies have included heterogeneous populations with different indications for antibiotic use, different study designs, and multitude of antimicrobial combinations that display dissimilar PK/PD properties. This review is the first to examine the role of prolonged versus intermittent infusion in nosocomial pneumonia. Despite the methodological differences of selected studies, patients who received prolonged over intermittent infusion rate displayed higher clinic cure rates than intermittent antibiotic infusion. In vitro and animal studies have demonstrated that the amount of time in which the free or non-protein bound drug concentration exceeds the MIC (fT > MIC) of the organism is the best predictor of clinical and microbiologic response for β-lactams [303132]. Because critically ill patients are at high risk of acquiring pathogens with high MICs, it can be quite challenging to achieve adequate PK/PD targets with classical intermittent dosing regimens. The increased volume of distribution in this population leads frequently to a lower steady state concentration/MIC with subsequent risk of therapeutic failure or emergence of drug resistant pathogens [33]. This is well illustrated in a study by Chytra and colleagues [34] who demonstrated that administration of meropenem by continuous infusion was associated with higher eradication rate and lower bacterial persistence in comparison with higher intermittent dosage without difference in the rate of resistance, colonization, or superinfection. Similarly, two other studies documented an improved bacteriologic efficacy of continuous infusion of β-lactam over bolus dosing [3536]. In 2009, a meta-analysis was published of all RCT from 1950 through November 2007 comparing the clinical benefits of continuous infusion regimens of β-lactam antibiotics with intermittent regimens [8]. No difference was found for mortality or clinical cure between the two groups. Yet, all but one of the included studies used a higher drug dose in the bolus group than in the continuous infusion group.
It is noteworthy that although clinical cure rate was significantly higher in patients who received extended or continuous infusions, the difference in mortality rate between the two groups did not reach statistical significance. The sample size of our meta-analysis may not have permitted detection of modest differences. To detect a significant difference in outcome, a 4-fold difference in mortality from baseline would have been necessary, or using the observed mortality between groups, more than 2,400 patients would have been required in each treatment group to achieve a power of 80% at a significance level of 0.05. In addition, the attributable mortality from nosocomial pneumonia (including ventilator associated pneumonia) has been reported to vary between 1.5% and 50% [37] depending on host characteristics, offending pathogens, and severity of illness. Due to the heterogeneity of the study population, the expected mortality of the selected studies was not uniform. The inclusion of low-risk patients could have resulted in a skewed mortality impact, and thus any mortality difference would have been extremely difficult to demonstrate. This explanation is further supported by the fact that infusion of β-lactams appears to be more effective in patients who have a higher acuity of illness [38]. This is illustrated in this study by the higher cure rate and improved survival of patients with APACHE >15. It is noteworthy to indicate that the subgroup analysis of RCTs did not reveal significant difference in clinical cure rate because the sample size of the RCTs is not powered for statistical significance. What is reassuring is that the mortality trend favors also the extended infusion. This analysis had only few retrospective studies.
Since the success of treatment depends upon antibiotic levels at the site of infection, prolonged infusion has been shown to include better penetration of β-lactam antibiotics into the lungs [3539]. In patients with ventilator associated pneumonia, alveolar concentration exceeding the susceptibility breakpoint for Gram negative bacteria can be attained more reliably with prolonged infusion. This approach can be achieved with minimal side effects. Overall we have seen no differences in adverse events between the two administration groups in those studies that reported these complications.
Nonetheless, it has been suggested that continuous exposure to antimicrobial concentrations slightly in excess of the reported MIC could select subpopulations of resistant organisms that typically are not detected by MIC testing and usually are eliminated or inhibited by higher peak antimicrobial concentrations. However, in vitro studies could not corroborate this hypothesis. Using a hollow fiber infection model with Pseudomonas aeruginosa, Felton and coworkers [40] demonstrated that extended infusion resulted in comparable antibacterial activities and rates of emergence of antimicrobial resistance as by bolus infusion.
Several limitations of this analysis should be noted. First, the numbers of patients enrolled in the selected studies were relatively small and most of the RCT were single centered, unblinded, with only a minority reporting on quality indicators, such as allocation concealment, intention-to-treat analysis, and losses to follow-up after randomization. Second, the microbiology of these infectious events was not consistently provided and although the majority of these cases were related to Gram negative pathogens, the susceptibility profiles were not reported. Given the fact that inappropriate antibiotic regimens are linked to increased mortality, the presence of highly resistant organisms may have altered the mortality rates in few of these studies. Third, concomitant antibiotic therapy reduces the validity of conclusions about the impact of prolonged infusion on clinical outcomes particularly when the agents used possess different antimicrobial spectrum. Therefore, it is not possible to determine accurately how clinical cure and mortality relate to antibiotic exposure. Fourth, the clinical trial end point definitions are not homogeneously and consistently established across the ten selected studies, but represent reasonable options that are based on available data. Further attempts to evaluate clinical trials through combination of retrospective and prospective studies should be undertaken with caution and for the generation of hypotheses only.
In conclusion, the current evidence suggests that prolonged infusion of beta-lactams results in higher clinical cure rate. However, well-designed RCTs are warranted to validate these findings before such strategy can be widely applied in clinical practice.
Figures and Tables
Figure 1
Flow diagram of the selection process of the identified studies.
CAP, community acquired pneumonia; HCAP, Health care associated pneumonia.

Figure 2
Forest plot comparing mortality rates in patients with nosocomial pneumonia receiving prolonged infusion and intermittent boluses.
CI, continuous infusion.

Figure 3
Funnel plot illustrating meta-analysis of mortality rate.
SE, standard error; RR, relative risk.

Figure 4
Forest plot comparing clinical cure rates in patients with nosocomial pneumonia receiving prolonged infusion and intermittent boluses.
CI, continuous infusion.

Table 1
Characteristics of selected studies for meta-analysis
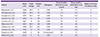
| Author | Study year | Study design | Sample size | Pathogens | Mean/median APACHE II score (CI, EI) | Mean/median APACHE II score (II) | Jadad or Newcastle Ottawa scale |
|---|---|---|---|---|---|---|---|
| Hanes et al., [13] | 2000 | RCT | 31 | GNB | 14 | 11 | 2 |
| McNabb et al., [14] | 2001 | RCT | 35 | GNB | 13.9 | 15.5 | 3 |
| Georges et al., [15] | 2005 | RCT | 50 | GNB | N/S | N/S | 2 |
| Lorente et al., [16] | 2006 | R | 89 | GNB | 15 | 15 | 7 |
| Lorente et al., [17] | 2007 | R | 121 | GNB | 16 | 16 | 8 |
| Sakka et al., [21] | 2007 | RCT | 20 | GNB | 26 | 28 | 2 |
| Chastre et al., [19] | 2008 | RCT | 531 | GNB | N/S | N/S | 2 |
| Lorente et al., [18] | 2009 | R | 83 | GNB | 16.1 | 16.2 | 8 |
| Wang et al., [20] | 2009 | R | 30 | A. baumannii | 20 | 17 | 7 |
| Fahimi et al., [22] | 2012 | P | 61 | GNB | 19 | 20 | 7 |
Table 2
Antibiotic dosage regimens and concomitant antibiotics

| Author | Study antibiotic | Extended infusion/continuous infusion | Intermittent infusion | Concomitant antibiotic |
|---|---|---|---|---|
| Hanes et al., [13] | Ceftazidime | LD, 2 g (0.5-h infusion), then 60 mg/kg/day as Cl | 2 g q8 h (0.5-h infusion) | N/S |
| McNabb et al., [14] | Ceftazidime | 3 g/d as CI | 2 g/d q8 h | Tobramycin |
| Georges et al., [15] | Cefepime | 4 g/d as Cl | 2 g q12 h | Amikacin |
| Lorente et al., [16] | Meropenem | LD, 1 g over 0.5 h, then 1 g q6 h as CI | 1 g q6 h (0.5-h infusion) | Tobramycin |
| Lorente et al., [17] | Ceftazidime | LD, 1 g over 0.5 h, then 2 g q12 h as CI | 2 g q12 h (0.5-h infusion) | Tobramycin |
| Sakka et al., [21] | Imipenem | LD, 1 g over 40 min, then 2 g/24 h as CI for 3 days, then 1 g q8 h over 40 min | 1 g q8 h (40-min infusion) | N/S |
| Chastre et al., [19] | Doripenem/Imipenem | Doripenem 500 mg q8 h as 4-hr EI | Imipenem 500 mg q6 h | Aminoglycoside |
| Lorente et al., [18] | Piperacilin/tazobactam | LD, 4.5 g over 0.5 h, then 4.5 g q6 h as CI | 4.5 g q6 h (0.5-h infusion) | Tobramycin |
| Wang et al., [20] | Meropenem | 500 mg q6 h as 3-h EI | 1 g q8 h (1-h infusion) | N/S |
| Fahimi et al., [22] | Piperacillin/tazobactam | 3.375 g q8 for 4 h as CI | 3.375 g q6 for 30 min | N/S |
Table 3
Subgroup analysis of selected studies

Notes
Financial Support Supported by a Merit Review Grant (CX000478) from the Department of Veterans Affairs (AES). None of the authors report any relevant conflict of interest. The views expressed in this review do not communicate an official position of the Department of Veterans Affairs.
References
2. Safdar N, Dezfulian C, Collard HR, Saint S. Clinical and economic consequences of ventilator-associated pneumonia: a systematic review. Crit Care Med. 2005; 33:2184–2193.

3. Fagon JY, Chastre J, Hance AJ, Montravers P, Novara A, Gibert C. Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. Am J Med. 1993; 94:281–288.

4. Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998; 26:1–10. quiz 11-2.

5. Kim MK, Capitano B, Mattoes HM, Xuan D, Quintiliani R, Nightingale CH, Nicolau DP. Pharmacokinetic and pharmacodynamic evaluation of two dosing regimens for piperacillin-tazobactam. Pharmacotherapy. 2002; 22:569–577.

6. Kim MK, Xuan D, Quintiliani R, Nightingale CH, Nicolau DP. Pharmacokinetic and pharmacodynamic profile of high dose extended interval piperacillin-tazobactam. J Antimicrob Chemother. 2001; 48:259–267.

7. Burgess DS, Waldrep T. Pharmacokinetics and pharmacodynamics of piperacillin/tazobactam when administered by continuous infusion and intermittent dosing. Clin Ther. 2002; 24:1090–1104.

8. Roberts JA, Webb S, Paterson D, Ho KM, Lipman J. A systematic review on clinical benefits of continuous administration of beta-lactam antibiotics. Crit Care Med. 2009; 37:2071–2078.

9. Tamma PD, Putcha N, Suh YD, Van Arendonk KJ, Rinke ML. Does prolonged beta-lactam infusions improve clinical outcomes compared to intermittent infusions? A meta-analysis and systematic review of randomized, controlled trials. BMC Infect Dis. 2011; 11:181.
10. Mah GT, Mabasa VH, Chow I, Ensom MH. Evaluating outcomes associated with alternative dosing strategies for piperacillin/tazobactam: a qualitative systematic review. Ann Pharmacother. 2012; 46:265–275.

11. Deeks JJ, Dinnes J, D'Amico R, Sowden AJ, Sakarovitch C, Song F, Petticrew M, Altman DG. International Stroke Trial Collaborative Group. European Carotid Surgery Trial Collaborative Group. Evaluating non-randomised intervention studies. Health Technol Assess. 2003; 7:iii–x. 1–173.

12. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996; 17:1–12.

13. Hanes SD, Wood GC, Herring V, Croce MA, Fabian TC, Pritchard E, Boucher BA. Intermittent and continuous ceftazidime infusion for critically ill trauma patients. Am J Surg. 2000; 179:436–440.

14. McNabb JJ, Nightingale CH, Quintiliani R, Nicolau DP. Cost-effectiveness of ceftazidime by continuous infusion versus intermittent infusion for nosocomial pneumonia. Pharmacotherapy. 2001; 21:549–555.

15. Georges B, Conil JM, Cougot P, Decun JF, Archambaud M, Seguin T, Chabanon G, Virenque C, Houin G, Saivin S. Cefepime in critically ill patients: continuous infusion vs. an intermittent dosing regimen. Int J Clin Pharmacol Ther. 2005; 43:360–369.

16. Lorente L, Lorenzo L, Martin MM, Jimenez A, Mora ML. Meropenem by continuous versus intermittent infusion in ventilator-associated pneumonia due to gram-negative bacilli. Ann Pharmacother. 2006; 40:219–223.

17. Lorente L, Jiménez A, Palmero S, Jiménez JJ, Iribarren JL, Santana M, Martín MM, Mora ML. Comparison of clinical cure rates in adults with ventilator-associated pneumonia treated with intravenous ceftazidime administered by continuous or intermittent infusion: a retrospective, nonrandomized, open-label, historical chart review. Clin Ther. 2007; 29:2433–2439.

18. Lorente L, Jiménez A, Martín MM, Iribarren JL, Jiménez JJ, Mora ML. Clinical cure of ventilator-associated pneumonia treated with piperacillin/tazobactam administered by continuous or intermittent infusion. Int J Antimicrob Agents. 2009; 33:464–468.

19. Chastre J, Wunderink R, Prokocimer P, Lee M, Kaniga K, Friedland I. Efficacy and safety of intravenous infusion of doripenem versus imipenem in ventilator-associated pneumonia: a multicenter, randomized study. Crit Care Med. 2008; 36:1089–1096.

20. Wang D. Experience with extended-infusion meropenem in the management of ventilator-associated pneumonia due to multidrug-resistant Acinetobacter baumannii. Int J Antimicrob Agents. 2009; 33:290–291.

21. Sakka SG, Glauner AK, Bulitta JB, Kinzig-Schippers M, Pfister W, Drusano GL, Sörgel F. Population pharmacokinetics and pharmacodynamics of continuous versus short-term infusion of imipenem-cilastatin in critically ill patients in a randomized, controlled trial. Antimicrobial Agents Chemother. 2007; 51:3304–3310.

22. Fahimi F, Ghafari S, Jamaati H, Baniasadi S, Tabarsi P, Najafi A, Akhzarmehr A, Hashemian SM. Continuous versus intermittent administration of piperacillin-tazobactam in intensive care unit patients with ventilator-associated pneumonia. Indian J Crit Care Med. 2012; 16:141–147.

23. Lorente L, Leon C. [Femoral venous catheterization. Does it really need to be avoided?]. Med Intensiva. 2009; 33:442–449.
24. Priest WS, Smith JM, McGEE CJ. The effect of anticoagulants on the penicillin therapy and the pathologic lesions of subacute bacterial endocarditis. N Engl J Med. 1946; 235:699–706.

25. Chant C, Leung A, Friedrich JO. Optimal dosing of antibiotics in critically ill patients by using continuous/extended infusions: a systematic review and meta-analysis. Crit Care. 2013; 17:R279.

26. Falagas ME, Tansarli GS, Ikawa K, Vardakas KZ. Clinical outcomes with extended or continuous versus short-term intravenous infusion of carbapenems and piperacillin/tazobactam: a systematic review and meta-analysis. Clin Infect Dis. 2013; 56:272–282.

27. Teo J, Liew Y, Lee W, Kwa AL. Prolonged infusion versus intermittent boluses of beta-lactam antibiotics for treatment of acute infections: a meta-analysis. Int J Antimicrob Agents. 2014; 43:403–411.

28. Shiu J, Wang E, Tejani AM, Wasdell M. Continuous versus intermittent infusions of antibiotics for the treatment of severe acute infections. Cochrane Database Syst Rev. 2013; 3:CD008481.

29. Kasiakou SK, Sermaides GJ, Michalopoulos A, Soteriades ES, Falagas ME. Continuous versus intermittent intravenous administration of antibiotics: a meta-analysis of randomised controlled trials. Lancet Infect Dis. 2005; 5:581–589.

30. Lodise TP, Lomaestro BM, Drusano GL. Society of Infectious Diseases Pharmacists. Application of antimicrobial pharmacodynamic concepts into clinical practice: focus on beta-lactam antibiotics: insights from the Society of Infectious Diseases Pharmacists. Pharmacotherapy. 2006; 26:1320–1332.

31. Jaruratanasirikul S, Sriwiriyajan S, Punyo J. Comparison of the pharmacodynamics of meropenem in patients with ventilator-associated pneumonia following administration by 3-hour infusion or bolus injection. Antimicrob Agents Chemother. 2005; 49:1337–1339.

32. De Jongh R, Hens R, Basma V, Mouton JW, Tulkens PM, Carryn S. Continuous versus intermittent infusion of temocillin, a directed spectrum penicillin for intensive care patients with nosocomial pneumonia: stability, compatibility, population pharmacokinetic studies and breakpoint selection. J Antimicrob Chemother. 2008; 61:382–388.

33. Boselli E, Breilh D, Rimmelé T, Poupelin JC, Saux MC, Chassard D, Allaouchiche B. Plasma and lung concentrations of ceftazidime administered in continuous infusion to critically ill patients with severe nosocomial pneumonia. Intensive Care Med. 2004; 30:989–991.

34. Chytra I, Stepan M, Benes J, Pelnar P, Zidkova A, Bergerova T, Pradl R, Kasal E. Clinical and microbiological efficacy of continuous versus intermittent application of meropenem in critically ill patients: a randomized open-label controlled trial. Crit Care. 2012; 16:R113.

35. Roberts JA, Boots R, Rickard CM, Thomas P, Quinn J, Roberts DM, Richards B, Lipman J. Is continuous infusion ceftriaxone better than once-a-day dosing in intensive care? A randomized controlled pilot study. J Antimicrob Chemother. 2007; 59:285–291.

36. Grant EM, Kuti JL, Nicolau DP, Nightingale C, Quintiliani R. Clinical efficacy and pharmacoeconomics of a continuous-infusion piperacillin-tazobactam program in a large community teaching hospital. Pharmacotherapy. 2002; 22:471–483.

37. Melsen WG, Rovers MM, Groenwold RH, Bergmans DC, Camus C, Bauer TT, Hanisch EW, Klarin B, Koeman M, Krueger WA, Lacherade JC, Lorente L, Memish ZA, Morrow LE, Nardi G, van Nieuwenhoven CA, O'Keefe GE, Nakos G, Scannapieco FA, Seguin P, Staudinger T, Topeli A, Ferrer M, Bonten MJ. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infect Dis. 2013; 13:665–671.

38. Lodise TP Jr, Lomaestro B, Drusano GL. Piperacillin-tazobactam for Pseudomonas aeruginosa infection: clinical implications of an extended-infusion dosing strategy. Clin Infect Dis. 2007; 44:357–363.

39. Boselli E, Breilh D, Rimmele T, Guillaume C, Xuereb F, Saux MC, Bouvet L, Chassard D, Allaouchiche B. Alveolar concentrations of piperacillintazobactam administered in continuous infusion to patients with ventilator-associated pneumonia. Crit Care Med. 2008; 36:1500–1506.

40. Felton TW, Goodwin J, O'Connor L, Sharp A, Gregson L, Livermore J, Howard SJ, Neely MN, Hope WW. Impact of Bolus dosing versus continuous infusion of Piperacillin and Tazobactam on the development of antimicrobial resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2013; 57:5811–5819.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download