Abstract
Purpose
The aim of our study is to evaluate the effects of administration of perioperative supplemental oxygen on anastomoses.
Methods
Forty male Wistar albino rats were used in the study and randomized into 4 groups. Ischemia-reperfusion models were built in groups 3 and 4. Jejunojejunostomy was performed in all rats and assigned to an oxygen/nitrous oxide mixture with a fraction of inspired oxygen of 30% in groups 1 and 3 and 80% in groups 2 and 4. The measurements of perianastomotic tissue oxygen pressure, bursting pressure, level of hydroxyproline were evaluated and compared in all groups.
Anastomotic leak (AL) is the most distressing early complication of gastrointestinal anastomosis; it also requires frequent reoperation. Systemic situations such as anemia, diabetes mellitus, malnutrition, vitamin deficiencies, smoking, and steroid therapy increase the risk of AL [1]. Some local factors such as presence of irradiated bowel anastomose involving disease affected bowel and inadequate blood flow are associated with AL [1]. AL is also associated with technical issues that present on early postoperative days. Uncontrolled leakage with diffuse peritonitis causes high morbidity and mortality. Most of the general factors suggest that vasoconstrictive effects may be the cause of local ischemia, and dehiscence of anastomosis. One of the most important factors is perfusion and the state of local oxygenation of the gastrointestinal anastomoses.
Oxygen (O2) is essential for oxidative metabolism and electron transport chain of living cells. Changes in O2 concentration represent a fundamental physiological stimulus for all aerobic organisms. Intracellular O2 concentration is maintained within a narrow range due to oxidative damages from hyperoxia or hypoxia. In fact, oxygen tension below 20 mmHg is significantly associated with AL, and hyperbaric O2 therapy leads to increased bursting pressure and hydroxyproline content in both normal and ischemic anastomoses [23].
Anastomose repair progresses most rapidly in optimally perfused tissue, and an adequate supply of O2 to the wound is necessary for proper healing. However, the role of supplemental O2 therapy in anastomotic healing is still very much at an experimental stage. The aim of our study is to evaluate the effects of administration of perioperative supplemental oxygen on anastomoses, and identify if AL reduces on rat models.
This study was performed with the Guide for the Care and Use of Laboratory Animals (National Research Council Institute for Laboratory Animal Research, US, Washington, National Academies Press, 1996) and the animal protocols were approved by the Animal Ethics Committee of the Ankara University with register number 2011-123-481.
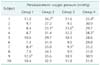
Our study is a randomized experimental study that was performed between February 2013 and April 2013 at Ankara University Faculty of Medicine, Laboratory of Experimental Animals and Research. Forty-six- to forty-eight-week-old male Wistar Albino rats weighing 200-250 mg were used in this study. They were randomized into 4 groups, each consisting of 10 rats, kept under 12-hour light and 12-hour dark cycles, and fed with standard rat chow and water. Intramuscular general anesthesia was performed with 40 mg of ketamine per kg (Alfamine, Alfasan Interventional B.V., Woerden, The Netherland) and 5 mg of xylazine per kg (Rompun, Bayer Turk Chemical Industry Limited Co., Istanbul, Turkey) to all rats. The rats in groups 1 and 2 received jejunojejunostomy, with a gas mixture of 30% O2 and 70% N2O in group 1 and 80% O2 and 20% N2O in group 2. In order to evaluate the effects of perioperative supplemental oxygen on high-risk anastomosis, we added the ischemia and reperfusion groups. We performed jejunojejunostomy after 60 minutes ischemia and 60 minutes reperfusion with a gas mixture of 30% O2 and 70% N2O in group 3 and 80% O2 and 20% N2O in group 4 (Table 1).
The procedures were performed by only one surgeon for standardization in accordance with the principles of asepsis and antisepsis. The rats were placed in the supine position. All rats were ventilated with planned oxygen concentration for 2 hours. After a median incision of the abdomen approximately 4 cm from xiphoid process, an automatic retractor was placed. Jejunojejunostomy was performed directly for groups 1 and 2. We applied 60 minutes ischemia, and 60 minutes reperfusion for groups 3 and 4, then jejunojejunostomy was performed.
A jejunum ans was cut at 2- to 3-cm distal of Trietz ligament and anastomosed with 7/0 polypropylene (Prolene, Ethicon, West Somerville, NJ, USA) number of 6 equidistant interrupted sutures. Tissue oxygen pressure of perianastomotic region was measured after anastomose. Then, 10 mL 0.9% NaCl was given in to the abdomen in order to support postoperative fluid replacement. Abdominal incisions were sutured full-thickness continuously with 3/0 silk material (Sterisilk, SSM, Istanbul, Turkey).
Following laparotomy, superior mesenteric artery and collaterals of inferior mesenteric artery and duodenum were identified. Microvascular clamps (Vasculostatt-Scanlan, St Louis, MO, USA) were placed and pulsatile arterial flow that was observed in the intestinal mesentery disappeared. Then abdominal incision was sutured with 3/0 silk material continuously. Relaparotomy was administered after 60 minutes, and microvascular clamps were removed. Intestines turned into the old pink color, and pulsatile arterial flow was determined. Again abdominal incisions were sutured and after 60 minutes, jejunojejunostomy was performed for groups 3 and 4.
Perianastomotic tissue oxygen pressure (PtiO2) was measured by use of tissue oxygen monitoring system (Licox, Integra Life Science, San Diego, CA, USA), and the microprobes of the vehicle (Licox CMP cc1, Integra Life Science) 0.6 mm sized, measuring tissue oxygen pressure by polarographic method. The microprobe was placed to the anastomose 5 mm advancing in the intestinal wall. The values of the body temperature of rats were entered into tissue oxygen monitoring system manually during the measurement. The probe was held within the tissue for 30 minutes for calibration, and then the data were obtained, and noted as perianastomotic oxygen pressure in mmHg.
Relaparotomy was performed on the seventh postoperative day. With anastomose in situ, an incision was made proximally to anastomose in the jejunum. A catheter was introduced and fixed with 2-0 silk thread. Distal of anastomose was ligated with 2-0 silk to close the intestinal lumen. A 3-way circuit was coupled to the catheter, the register gauge and an arterial blood pressure monitoring system. A flow of 2 mL/min was injected in to the circuit until the rupture of anastomose and the maximum pressure was recorded at the time of the rupture in mmHg.
The tissue samples were kept frozen at -80℃ until use. Then samples were weighed on a precision scale, and homogenized in saline. The homogenates were centrifuged at 2,000 rpm for 15 minutes. Supernatants were hydrolyzed for 16-18 hours by equal amounts of hydrochloric acid. The released hydroxyproline was oxidized with chloramine, then reacted with Ehrlich reagent to form chromophore compound and then spectrophotometric measures (560 nm) were obtained. Tissue hydroxyproline levels were calculated and noted as microgram/mg wet tissue.
Statistical analyses were performed using SPSS ver. 11.5 (SPSS Inc., Chicago, IL, USA). Perianastomotic tissue oxygen pressure, anastomose bursting pressure, and the level of hydroxyproline were compared between 4 groups. Data were expressed as median (minimum and maximum values). The Mann-Whitney U test was used for comparison of 2 independent groups. A value of P < 0.05 was accepted as statistically significant.
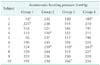
All of the 40 experimental animals were followed up for 7 days, and they all underwent relaparotomy. There was no mortality, intra-abdominal abscess, or AL. All bursts were at anastomotic site during the measurement of anastomotic bursting pressure. The subjects were divided into 4 groups, and the measurements of perianastomotic tissue pressures, anastomotic bursting pressures, and levels of hydroxyproline were noted.
Anastomotic bursting pressures of the subjects in all groups are shown in Table 3. The median values of each group were 155.5, 236.5, 123.5, and 218.5 mmHg respectively (Fig. 2).
We compared the groups for anastomotic bursting pressures. The values of bursting pressures in group 2 were identified significantly higher than group 1 (P = 0.002). Similarly, we found significant high values of bursting pressures for group 4 compared with group 3 (P < 0.001). However, there were not any significant differences between groups 1 and 3 and also between groups 2 and 4 (P > 0.05).
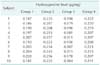
The anastomoses were resected and analyzed for the levels of tissue hydroxyproline after the measurements of anastomotic bursting pressures. The levels of hydroxyproline of the subjects in all groups are shown in Table 4. The median values of each group were 0.195, 0.234, 0.197, and 0.213 µg/mg respectively (Fig. 3).
The levels of tissue hydroxyproline were compared, and the values for group 2 were identified higher than group 1 significantly (P < 0.001). And, we also found significantly high values for group 4 compared with group 3 (P = 0.003). However, there were not any significant differences between groups 1 and 3, and between groups 2 and 4 (P > 0.05).
The gastrointestinal anastomose is one of the most important issues in surgical practice. Numerous studies have been carried out so far in order to reveal superiority of different techniques. The common aim of these studies was to investigate the techniques for reducing the complication rates to an acceptable value.
One of the important factors for safety of anastomose is sufficient tissue perfusion [45]. The wound healing process is faster in optimally perfused tissue, and sufficient oxygen should reach to the wound for proper healing. Many studies show less wound infection with perioperative 80% O2 support compared with 30% O2 ventilation [467]. Belda et al. [4] studied with a total of 143 patients receiving 30%, and 148 receiving 80% perioperative oxygen, and they identified significant reductions in the risk of wound infection. Contrary to this, Mayzler et al. [8] studied a group of 38 patients and performed elective colorectal surgery, but there was no significant difference between 80% and 30% O2 supplied groups in wound infection. However, in the study of Mayzler et al. [8], the small sample size was a restriction factor to evaluate if perioperative oxygen supplement reduces the incidence of wound infection in elective colorectal surgery. And also, Pryor et al. [9] stopped their study because the wound infection in high oxygen group was more than 2 times. The meta analysis of this subject was performed with 3,001 patients, and an absolute 3%, and relative 25% reduction in the risk of the surgical site infection was reported [10]. In another meta analysis about the effects of supplemental perioperative oxygen on surgical site infection showed a benefit in preventing surgical site infection in patients undergoing colorectal surgery [11]. Also, Turan et al. [12] studied the postoperative side effects and reported less nausea and vomiting with perioperative 80% O2 ventilation. A recent prospective randomized, double-blind, controlled study of Schietroma et al. [13] showed that supplemental 80% FiO2 reduced postoperative surgical site infections. In this study, surgical site infection did not occurred in any subjects and so the beneficial effect of supplemental 80% FiO2 was not detected under these terms. Also, in our opinion, more subjects were needed for evaluation of surgical site infection.
Garcia-Botello et al. [3] evaluated the effects of perioperative oxygen support on pH and pCO2 of the colorectal anastomoses, and they further found that the application of 80% O2 perioperatively was related to the recovery of relative anastomotic hypoperfusion during the surgery and postoperative 6th hour. Similarly, we identified high perianastomotic oxygen saturation and bursting pressure with perioperative 80% O2 ventilation, which suggested that there was not any hypoperfusion on anastomoses.
Clinically and physiologically reversible signs of perioperative application of high concentrated oxygen ventilation occur at least 0-24 hours [141516]. Schietroma et al. [17] studied the effect of high oxygen ventilation on the intraperitoneal anastomosis in middle and inferior rectal cancer and they showed that the risk of anastomosis leakage is 46% less on the 80% O2 administered group versus 30% O2 administered group.
Kimberger et al. [18] showed increase in tissue oxygen pressure during 100% O2 ventilation, although intra-anastomotic tissue oxygen pressure remained low. The reason for this is thought to be the variation due to the distance of the oxygen sensitive probe which is used to evaluate the intra-anastomotic tissue oxygen levels to the area of the stitches. Because of the variation in tissue oxygen pressure levels, they thought about evaluating the tissue oxygen levels from the perianastomotic area with the perianastomotic tissue oxygen pressure evaluation probe which has a narrower range of variation that is more reliable as a possible predictive factor [18]. In light of this information and the difficulty of making evaluations in the rat intestine, we made the evaluations only in the perianastomotic area in our study.
Collagen is the essential structural protein of the connective tissue. And it is responsible for the stability of the anastomosis and the elasticity of the tissue. Proline and lysine are the basic aminoacids responsible for the collagen synthesis. Proline and lysine react with ascorbic acid and oxygen to form tropocollagen. Collagen fibrils are formed by the polymerization of tropocollagen. Because of the expected increase in the hydroxylation of lysine and proline in the oxygen supported group, the consequence is the strengthening of tissue collagen levels and the power of the anastomosis [19]. When analysis is made on the data on the anastomotic bursting pressure, the anastomotic bursting pressure levels are found to be statistically higher in both the 80% O2 supported only group, and the 80% O2 supported group within the ischemia-reperfusion performed group versus groups that did not get any oxygen support. But there were no significant differences between ischemia reperfusion groups and non ischemic groups with the same FiO2. This data can lead to interrogation whether or not our ischemia reperfusion model is correct. However, this model was applied similarly in groups 3 and 4, and it did not make a difference in terms of comparison between 30% and 80% FiO2 support (group 1 vs. group 2 and group 3 vs. group 4).
We also evaluated the anastomotic tissue hydroxyproline level which is a parameter that helps to evaluate the anastomosis healing. Anastomotic tissue hydroxyproline levels are statistically higher in the 80% O2 ventilated group versus the 30% O2 ventilated group.
The experiments were performed in a small laboratory room, and ventilator and rats were very close to eachother. Thus, the experiment was not blinded to the operator; this was a limitation of the study.
In conclusion, we researched the effects of 80% O2 on intestinal anastomoses, which resulted in high perianastomotic tissue saturation, bursting pressures, and tissue hydroxyproline. We think that perioperative high oxygen support contributes positively to the anastomotic healing.
Figures and Tables
Fig. 1
The median values of perianastomotic oxygen pressures for each group. We evaluated perianastomotic oxygen pressure for each group, and identified the values of group 2 significantly higher than group 1 (P < 0.001). Similarly, we found a significant high value of perianastomotic oxygen pressure for group 4 compared with group 3 (P < 0.001). However, there were no significant differences between groups 1 and 3 and also between groups 2 and 4 (P > 0.05).

References
1. Chen C. The art of bowel anastomosis. Scand J Surg. 2012; 101:238–240.
2. Sheridan WG, Lowndes RH, Young HL. Tissue oxygen tension as a predictor of colonic anastomotic healing. Dis Colon Rectum. 1987; 30:867–871.
3. Garcia-Botello SA, Garcia-Granero E, Lillo R, Lopez-Mozos F, Millan M, Lledo S. Randomized clinical trial to evaluate the effects of perioperative supplemental oxygen administration on the colorectal anastomosis. Br J Surg. 2006; 93:698–706.
4. Belda FJ, Aguilera L, Garcia de la Asuncion J, Alberti J, Vicente R, Ferrandiz L, et al. Supplemental perioperative oxygen and the risk of surgical wound infection: a randomized controlled trial. JAMA. 2005; 294:2035–2042.
5. Hunt TK, Pai MP. The effect of varying ambient oxygen tensions on wound metabolism and collagen synthesis. Surg Gynecol Obstet. 1972; 135:561–567.
6. Greif R, Akca O, Horn EP, Kurz A, Sessler DI. Outcomes Research Group. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med. 2000; 342:161–167.
7. Brasel K, McRitchie D, Dellinger P. EBRS Group. Canadian Association of General Surgeons and American College of Surgeons Evidence Based Reviews in Surgery. 21: the risk of surgical site infection is reduced with perioperative oxygen. Can J Surg. 2007; 50:214–216.
8. Mayzler O, Weksler N, Domchik S, Klein M, Mizrahi S, Gurman GM. Does supplemental perioperative oxygen administration reduce the incidence of wound infection in elective colorectal surgery? Minerva Anestesiol. 2005; 71:21–25.
9. Pryor KO, Fahey TJ 3rd, Lien CA, Goldstein PA. Surgical site infection and the routine use of perioperative hyperoxia in a general surgical population: a randomized controlled trial. JAMA. 2004; 291:79–87.
10. Qadan M, Akca O, Mahid SS, Hornung CA, Polk HC Jr. Perioperative supplemental oxygen therapy and surgical site infection: a meta-analysis of randomized controlled trials. Arch Surg. 2009; 144:359–366.
11. Al-Niaimi A, Safdar N. Supplemental perioperative oxygen for reducing surgical site infection: a meta-analysis. J Eval Clin Pract. 2009; 15:360–365.
12. Turan A, Apfel CC, Kumpch M, Danzeisen O, Eberhart LH, Forst H, et al. Does the efficacy of supplemental oxygen for the prevention of postoperative nausea and vomiting depend on the measured outcome, observational period or site of surgery? Anaesthesia. 2006; 61:628–633.
13. Schietroma M, Cecilia EM, Sista F, Carlei F, Pessia B, Amicucci G. High-concentration supplemental perioperative oxygen and surgical site infection following elective colorectal surgery for rectal cancer: a prospective, randomized, double-blind, controlled, single-site trial. Am J Surg. 2014; 208:719–726.
14. DuBois AB, Turaids T, Mammen RE, Nobrega FT. Pulmonary atelectasis in subjects breathing oxygen at sea level or at simulated altitude. J Appl Physiol. 1966; 21:828–836.
15. Caldwell PR, Lee WL Jr, Schildkraut HS, Archibald ER. Changes in lung volume, diffusing capacity, and blood gases in men breathing oxygen. J Appl Physiol. 1966; 21:1477–1483.
16. Montgomery AB, Luce JM, Murray JF. Retrosternal pain is an early indicator of oxygen toxicity. Am Rev Respir Dis. 1989; 139:1548–1550.
17. Schietroma M, Carlei F, Cecilia EM, Piccione F, Bianchi Z, Amicucci G. Colorectal Infraperitoneal anastomosis: the effects of perioperative supplemental oxygen administration on the anastomotic dehiscence. J Gastrointest Surg. 2012; 16:427–434.
18. Kimberger O, Fleischmann E, Brandt S, Kugener A, Kabon B, Hiltebrand L, et al. Supplemental oxygen, but not supplemental crystalloid fluid, increases tissue oxygen tension in healthy and anastomotic colon in pigs. Anesth Analg. 2007; 105:773–779.
19. Cohen IK, Diegelmann RF, Lindblad WJ. Wound healing: biochemical & clinical aspects. Philadelphia: W.B. Saunders Co.;1992.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download