Abstract
In this study, we present the surgical treatment of obstructive sleep apnea in a child with Treacher Collins syndrome. A 10-year-old girl with a past history of Treacher Collins syndrome presented to our clinic with her parents for respiratory distress and insomnia. The patient was referred to a sleep laboratory where she was diagnosed with obstructive sleep apnea, which was a consequence of her Treacher Collins syndrome. The patient underwent mandibular distraction osteogenesis under general anesthesia. The mandible was expanded by 15 mm using internal bilateral distractors. After distraction osteogenesis, the patient’s respiratory problems resolved, and she was able to sleep comfortably. Distraction osteogenesis was an effective method of advancing the mandible, increasing the upper airway space and ultimately preventing obstructive sleep apnea syndrome in patients with Treacher Collins syndrome.
Obstructive sleep apnea syndrome (OSAS) is characterized by recurrent obstruction of the upper airway during sleep. It is a major health problem that affects 2% to 4% of children and adults, and ultimately influences multiple organ systems1. It is typically diagnosed using lateral cephalometry, computed tomography and polysomnography2. Partial or complete obstruction of the upper airway during sleep decreases oxygen saturation, causes sleep disruption, and adversely affects patients’ physical and psychological health13. OSAS is common among patients with craniofacial deformities4. In children, it can lead to growth retardation, aggression, hyperactivity, attention-deficit disorder, cognitive function disorders and poor socialization5. Furthermore, OSAS can suppress memory, learning and problem solving abilities in children6.
Treacher Collins syndrome (TCS) is an autosomal dominant, craniofacial disease with an incidence of approximately 1 in 50,000 live births7. The clinical findings in patients with TCS include zygomatic and mandibular hypoplasia, abnormalities of the outer ear and inner ear bones, cleft palate, choanal atresia and eyelid abnormalities8. Abnormal anatomy in the upper airway increases the risk of OSAS. Therefore, the prevalence of OSAS tends to be high in patients with TCS9.
In recent years, distraction osteogenesis has become the preferred treatment of choice for airway obstruction in patients with congenital syndromes such as TCS and Pierre Robin syndrome10. Distraction osteogenesis prevents upper airway obstruction by advancing the mandible anteriorly and removing the tongue base from the oropharynx.
The purpose of this case report was to present the surgical treatment of obstructive sleep apnea using distraction osteogenesis in a child with TCS.
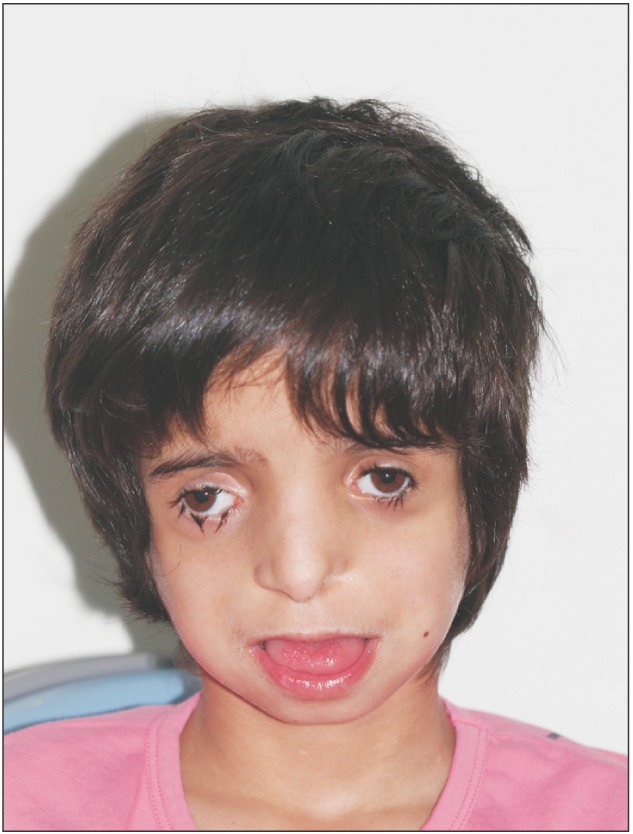
A 10-year-old girl with TCS presented to our clinic with her parents for respiratory distress and insomnia. The clinical examination revealed symmetrically underdeveloped zygomatic bones, depressed palpebral fissures with a partial absence of eyelashes in the lower eyelids.(Fig. 1) There was also mandibular hypoplasia. The patient’s tongue was protruding outside of her mouth, as she could not close her mouth due to mandibular micrognathia. There was posterior maxillary vertical hypoplasia, as well as a significantly increased occlusal plane angle. The external ear development was abnormal. The patient had hearing problems. The patient was diagnosed with obstructive sleep apnea, which was likely a result of her TCS.
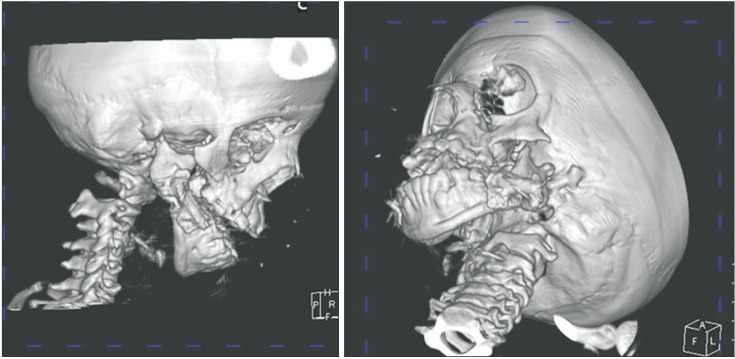
After a radiological examination (Fig. 2), mandibular distraction osteogenesis was planned. A submandibular incision was performed under general anesthesia. The mandibular corpus was revealed by blunt dissection. An osteotomy was performed with piezo surgery from the front of the ramus to be perpendicular to the mandibular corpus.(Fig. 3) A monocortical incision was made in the section corresponding to the mandibular canal in order to protect the inferior alveolar nerve. An osteotomy was then completed using chisels. Distractors were placed (Fig. 4), and the wound was closed primarily with resorbable sutures. The same procedure was performed on both sides of the mandible. There were no surgical or neurological complications encountered during the operation. The patient was treated with cefamezin (500 mg, twice a day) and intramuscular diclofenac sodium (once a day) for one week. After one week, the distraction was performed to provide 1 mm expansion per day. A 15-mm expansion was provided in the mandible using internal bilateral distractors. After a three-month latent phase (Fig. 5), the distractors were removed through the same incision site under general anesthesia. After distraction osteogenesis, the patient’s respiratory problems resolved. She was able to position her tongue in her mouth, and could sleep comfortably. The patient was doing well at her one-year follow-up examination.(Fig. 6)
We obtained the written consent from the patient’s legal gardian.
TCS is a rare congenital, craniofacial condition with an incidence of 1 in 50,000 live births7. TCS is characterized by a convex facial profile, prominent nasal dorsum, retrusive lower jaw and zygomatic bone, and hypoplastic mandible811. The external ears may also be absent, malformed or mispositioned. Hypoplasia of varying degrees may also be seen in the external ear canals and middle ear bones, leading to hearing loss12. The diagnosis of TCS is performed with the help of a detailed clinical evaluation and molecular genetic tests11. The patient in this case had already been diagnosed with TCS, and had the characteristic clinical features.
There is increased prevalence of obstructive sleep apnea in patients with craniofacial deformities than there is in those without such anatomical abnormalities4. OSAS can cause growth retardation, attention deficits, or cognitive function disorders in children5. Children with OSAS also experience reduced learning and problem-solving abilities compared to those of children without OSAS6. OSAS increases the risk of cardiovascular and metabolic complications for both children and adults7. Therefore, the diagnosis and treatment of OSAS are very important.
Severe cases of obstructive sleep apnea in children are treated with a permanent tracheostomy. There are many morbidities of long-term tracheostomies, including tracheomalacia, chronic bronchitis, throat tightness and dislocation of the tracheostomy tube13. Therefore, it can be difficult to care for patients with tracheostomy13. Distraction osteogenesis is the preferred treatment method in patients with obstructive sleep apnea due to mandibular shortness1314. Other procedures, including orthognathic surgery, rib grafts, sternoclavicular grafts, and total joint prostheses have also been used to reconstruct the major facial and TMJ deformities associated with TCS15. In this case study, the patient was performed successfully by distraction osteogenesis. We preferred distraction osteogenesis to avoid mandible relapse.
Mandibular advancement for the treatment of OSAS was initially performed using bilateral external distracters10. External devices are advantageous because of their ease of use, manipulation and versatility. However, external devices also create aesthetic, social problems and produce scars. These devices have reduced retention period and an increased relapse incidence compared to those of internal devices16. In this study, we performed distraction osteogenesis using internal devices in the treatment of obstructive sleep apnea. We considered an extraoral multi-vector distractor. However, we deferred the use of this device in our patient, because we believed that she would be bothered by the device, potentially compromising the treatment. Therefore, we chose an intraoral distractor device. We were unable to perform orthognathic surgery in this patient. Internal distractors increase patient comfort, increase device stability during the treatment and provide better bone quality over those of external devices10.
Long term follow-up examinations are indicated in these patients in order to evaluate the effects of mandibular growth, airway relapse, and the need for additional surgical intervention. In addition to head and neck computed tomography, three-dimensional tomography is used to evaluate mandibular distraction and its effects on airway volume1017. The use of plain radiography is not as effective as three-dimensional tomography because it only provides two-dimensional images. We did not detect any relapse at the one-year follow-up of our patient using computed tomography.
In this study, distraction osteogenesis was effective in advancing the mandible, increasing the upper airway space and eliminating OSAS in our patient with TCS.
References
1. Akre H, Øverland B, Åsten P, Skogedal N, Heimdal K. Obstructive sleep apnea in Treacher Collins syndrome. Eur Arch Otorhinolaryngol. 2012; 269:331–337. PMID: 21626120.

2. Jin SM, Lee HS, Ryu HH, Ryu SH, Shin DY, Kim CH, et al. Retrospective study on the airway obstruction aspects of computed tomography and lateral cephalometry and the correlation of polysomnography in obstructive sleep apnea patients. J Korean Assoc Oral Maxillofac Surg. 2012; 38:295–304.

3. Okşayan R, Sökücü O, Uyar M, Topçuoğlu T. Effects of edentulism in obstructive sleep apnea syndrome. Niger J Clin Pract. 2015; 18:502–505. PMID: 25966722.

4. Hoeve LJ, Pijpers M, Joosten KF. OSAS in craniofacial syndromes: an unsolved problem. Int J Pediatr Otorhinolaryngol. 2003; 67(Suppl 1):S111–S113. PMID: 14662180.

5. Rosen CL, Storfer-Isser A, Taylor HG, Kirchner HL, Emancipator JL, Redline S. Increased behavioral morbidity in school-aged children with sleep-disordered breathing. Pediatrics. 2004; 114:1640–1648. PMID: 15574628.

6. Hoeve HL, Joosten KF, van den Berg S. Management of obstructive sleep apnea syndrome in children with craniofacial malformation. Int J Pediatr Otorhinolaryngol. 1999; 49(Suppl 1):S59–S61. PMID: 10577777.

7. Østertun Geirdal A, Øverland B, Heimdal K, Storhaug K, Asten P, Akre H. Association between obstructive sleep apnea and health-related quality of life in individuals affected with Treacher Collins syndrome. Eur Arch Otorhinolaryngol. 2013; 270:2879–2884. PMID: 23455582.

8. Posnick JC, Ruiz RL. Treacher Collins syndrome: current evaluation, treatment, and future directions. Cleft Palate Craniofac J. 2000; 37:434. PMID: 11034023.

9. Plomp RG, Bredero-Boelhouwer HH, Joosten KF, Wolvius EB, Hoeve HL, Poublon RM, et al. Obstructive sleep apnoea in Treacher Collins syndrome: prevalence, severity and cause. Int J Oral Maxillofac Surg. 2012; 41:696–701. PMID: 22521672.

10. Rachmiel A, Emodi O, Rachmiel D, Aizenbud D. Internal mandibular distraction to relieve airway obstruction in children with severe micrognathia. Int J Oral Maxillofac Surg. 2014; 43:1176–1181. PMID: 25052572.

11. Mohan RP, Verma S, Agarwal N, Singh U. Treacher Collins syndrome: a case report. BMJ Case Rep. 2013; DOI: 10.1136/bcr-2013-009341.

12. Posnick JC. Treacher Collins syndrome: perspectives in evaluation and treatment. J Oral Maxillofac Surg. 1997; 55:1120–1133. PMID: 9331237.

13. Rachmiel A, Emodi O, Aizenbud D. Management of obstructive sleep apnea in pediatric craniofacial anomalies. Ann Maxillofac Surg. 2012; 2:111–115. PMID: 23483041.

14. Morovic CG, Monasterio L. Distraction osteogenesis for obstructive apneas in patients with congenital craniofacial malformations. Plast Reconstr Surg. 2000; 105:2324–2330. PMID: 10845284.

15. Wolford LM, Perez DE. Surgical management of congenital deformities with temporomandibular joint malformation. Oral Maxillofac Surg Clin North Am. 2015; 27:137–154. PMID: 25483449.

16. Diner PA, Kollar E, Martinez H, Vazquez MP. Submerged intraoral device for mandibular lengthening. J Craniomaxillofac Surg. 1997; 25:116–123. PMID: 9234090.

17. Kaban LB, Seldin EB, Kikinis R, Yeshwant K, Padwa BL, Troulis MJ. Clinical application of curvilinear distraction osteogenesis for correction of mandibular deformities. J Oral Maxillofac Surg. 2009; 67:996–1008. PMID: 19375009.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download