1. Pitout JD. Recent changes in the epidemiology and management of extended-spectrum β-lactamase-producing
Enterobacteriaceae. F1000 Med Rep. 2009; 1:pii:84.

2. Jadhav S, Mısra R, Gandham N, Ujagare M, Ghosh P, Kalpana A, et al. Increasing incidence of multidrug resistance Klebsiella pneumoniae infections in hospital and community settings. Int J Microbiol Res. 2012; 4:253–257.
3. Bradford PA, Urban C, Mariano N, Projan SJ, Rahal JJ, Bush K. Imipenem resistance in
Klebsiella pneumoniae is associated with the combination of ACT-1, a plasmid-mediated AmpC β-lactamase, and the loss of an outer membrane protein. Antimicrob Agents Chemother. 1997; 4:563–569. PMID:
9055993.
4. Kaczmarek FM, Dib-Hajj F, Shang W, Gootz TD. High-level carbapenem resistance in a
Klebsiella pneumoniae clinical isolate is due to the combination of
blaACT-1 β-lactamase production, porin OmpK35/36 insertional inactivation, and down-regulation of the phosphate transport porin phoE. Antimicrob Agents Chemother. 2006; 50:3396–3406. PMID:
17005822.
5. Nordmann P, Dortet L, Poirel L. Carbapenem resistance in
Enterobacteriaceae: here is the storm! Trends Mol Med. 2012; 18:263–272. PMID:
22480775.
6. Giani T, Pini B, Arena F, Conte V, Bracco S, Migliavacca R, et al. Epidemic diffusion of KPC carbapenemase-producing
Klebsiella pneumoniae in Italy: results of the first countrywide survey, 15 May to 30 June 2011. Euro Surveill. 2013; 18:pii:20489.

7. Poirel L, Héritier C, Tolün V, Nordmann P. Emergence of oxacillinase-mediated resistance to imipenem in
Klebsiella pneumoniae. Antimicrob Agents Chemother. 2004; 48:15–22. PMID:
14693513.
8. Aktaş Z, Kayacan CB, Schneider I, Can B, Midilli K, Bauernfeind A. Carbapenem-hydrolyzing oxacillinase, OXA-48, persists in
Klebsiella pneumonia in Istanbul, Turkey. Chemotherapy. 2008; 54:101–106. PMID:
18303258.
9. Carrër A, Poirel L, Eraksoy H, Cagatay AA, Badur S, Nordmann P. Spread of OXA-48-positive carbapenem-resistant
Klebsiella pneumonia isolates in Istanbul, Turkey. Antimicrob Agents Chemother. 2008; 52:2950–2954. PMID:
18519712.
10. Gülmez D, Woodford N, Palepou MF, Mushtaq S, Metan G, Yakupogullari Y, et al. Carbapenem-resistant
Escherichia coli and
Klebsiella pneumonia isolates from Turkey with OXA-48-like carbapenemases and outer membrane protein loss. Int J Antimicrob Agents. 2008; 31:523–526. PMID:
18339523.
11. Poirel L, Ozdamar M, Ocampo-Sosa AA, Türkoğlu S, Ozer UG, Nordmann P. NDM-1-producing
Klebsiella pneumoniae now in Turkey. Antimicrob Agents Chemother. 2012; 56:2784–2785. PMID:
22391536.
12. Copur Cicek A, Ozad Duzgun A, Saral A, Sandalli C. Determination of a novel integron-located variant (
blaOXA-320) of Class D β-lactamase in
Proteus mirabilis. J Basic Microbiol. 2014; 54:1030–1035. PMID:
24027220.
13. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. M100-S23. Wayne, PA: Clinical and Laboratory Standards Institute;2013.
14. Altschul SF, Madden TL, Schäffer AA, Zhang J, Zhang Z, Miller W, et al. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 1997; 25:3389–3402. PMID:
9254694.

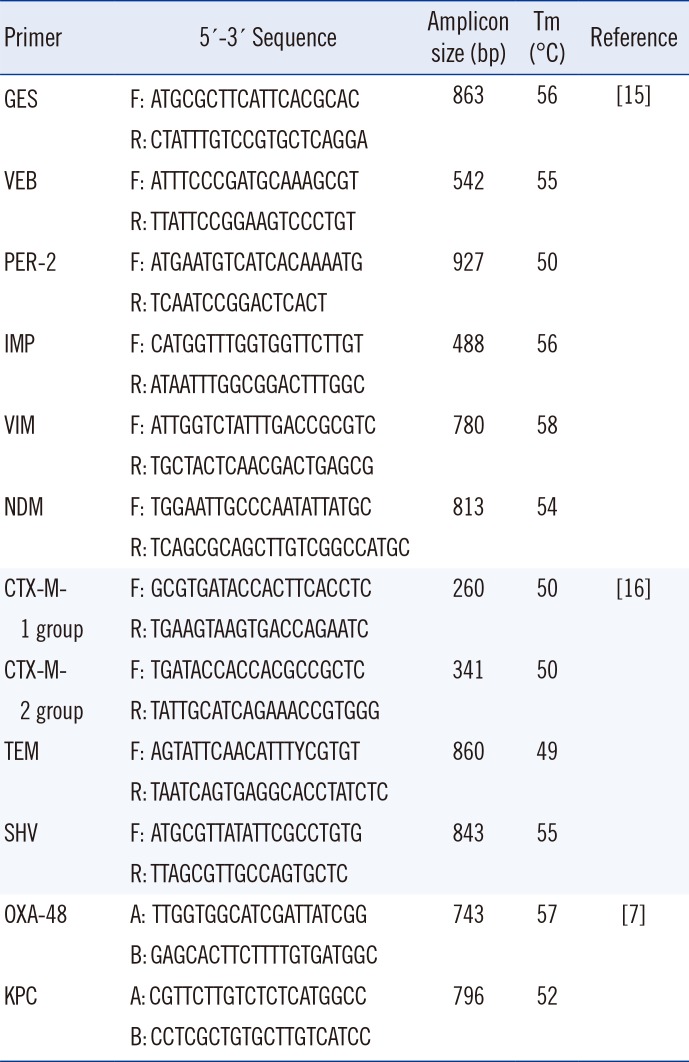
15. Copur Cicek A, Saral A, Iraz M, Ceylan A, Duzgun AO, Peleg AY, et al. OXA- and GES-type β-lactamases predominate in extensively drug-resistant
Acinetobacter baumannii isolates from a Turkish University Hospital. Clin Microbiol Infect. 2014; 20:410–415. PMID:
23957892.
16. Copur Cicek A, Saral A, Ozad Duzgun A, Yasar E, Cizmeci Z, Ozlem Balci P, et al. Nationwidestudy of
Escherichia coli producing extended-spectrum β-lactamases TEM, SHV and CTX-M in Turkey. J Antibiot. 2013; 66:647–650. PMID:
23838745.
17. Andriamanantena TS, Ratsima E, Rakotonirina HC, Randrianirina F, Ramparany L, Carod JF, et al. Dissemination of multidrug resistant
Acinetobacter baumannii in various hospitals of Antananarivo Madagascar. Ann Clin Microbiol Antimicrob. 2010; 9:17. PMID:
20591154.

18. Podschun R, Ullman U.
Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin Microbiol Rev. 1998; 11:589–603. PMID:
9767057.
19. Poirel L, Pitout JD, Nordmann P. Carbapenemases: molecular diversity and clinical consequences. Future Microbiol. 2007; 2:501–512. PMID:
17927473.

20. Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, et al. Characterization of a new metallo-beta-lactamase gene, bla(NDM-1), and a novel erythromycin esterase gene carried on a unique genetic structure in
Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother. 2009; 53:5046–5054. PMID:
19770275.
21. Johnson AP, Woodford N. Global spread of antibiotic resistance: the example of New Delhi metallo-β-lactamase (NDM)-mediated carbapenem resistance. J Med Microbiol. 2013; 62:499–513. PMID:
23329317.

22. Seija V, Medina Presentado JC, Bado I, Papa Ezdra R, Batista N, Gutierrez C, et al. Sepsis caused by New Delhi metallo-β-lactamase (blaNDM-1) and qnrD-producing Morganella morganii, treated successfully with fosfomycin and meropenem: case report and literature review. Int J Infect Dis. 2015; 30:20–26. PMID:
25447717.

23. Nordmann P, Poirel L, Walsh TR, Livermore DM. The emerging NDM carbapenemases. Trends Microbiol. 2011; 19:588–595. PMID:
22078325.

24. Kim SY, Rhee JY, Shin SY, Ko KS. Characteristics of community-onset NDM-1-producing
Klebsiella pneumonia isolates. J Med Microbiol. 2014; 63:86–89. PMID:
24173426.
25. Rasheed JK, Kitchel B, Zhu W, Anderson KF, Clark NC, Ferraro MJ, et al. New Delhi metallo-β-lactamase-producing Enterobacteriaceae, United States. Emerg Infect Dis. 2013; 19:870–878. PMID:
23731823.
26. Evans B, Amyes SG. OXA β-lactamases. Clin Microbiol Rev. 2014; 27:241–263. PMID:
24696435.

27. Alp E, Perçin D, Colakoğlu S, Durmaz S, Kürkcü CA, Ekincioğlu P, et al. Molecular characterization of carbapenem-resistant
Klebsiella pneumoniae in a tertiary university hospital in Turkey. J Hosp Infect. 2013; 84:178–180. PMID:
23623803.
28. Pitout JD, Nordmann P, Laupland KB, Poirel L. Emergence of
Enterobacteriaceae producing extended-spectrum β-lactamases (ESBLs) in the community. J Antimicrob Chemother. 2005; 56:52–59. PMID:
15917288.
29. Gür D, Gülay Z, Akan OA, Aktaş Z, Kayacan CB, Cakici O, et al. Resistance to newer beta-lactams and related ESBL types in gram-negative nosocomial isolates in Turkish hospitals: results of the multicentre HITIT study. Mikrobiyol Bul. 2008; 42:537–544. PMID:
19149074.
30. Onnberg A, Mölling P, Zimmermann J, Söderquist B. Molecular and phenotypic characterization of
Escherichia coli and
Klebsiella pneumoniae producing extended-spectrum β-lactamases with focus on CTX-M in a low-endemic area in Sweden. APMIS. 2011; 119:287–295. PMID:
21492229.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download