Abstract
Florid osseous dysplasia (FOD) is an uncommon, benign, cemento-osseous lesion of the jaws. The etiology of FOD is still unknown. It is often asymptomatic and may be identified on routine dental radiographs. The classic radiographic appearance of FOD is amorphous, lobulated, mixed radiolucent/radiopaque masses of cotton-wool appearance with a sclerotic border in the jaws. In our case the lesion was found incidentally on routine periapical radiographs taken for restored teeth and edentulous areas. For further and detailed examination, a panoramic radiograph and cone-beam computed tomograph (CBCT) were taken. The panoramic radiograph and CBCT revealed maxillary bilateral and symmetrical, non-expansile, well-defined, round, radiopaque masses in contact with the root of the maxillary right second molar and left first molar teeth. Our aim in presenting this case report was to highlight the importance of imaging in diagnosis of FOD.
Florid osseous dysplasia (FOD) is an uncommon, benign, osseous lesion of the jaws. FOD is synonymous with gigantiform cementoma and familial multiple cementomas.1 FOD refers to a group of osseous lesions with multiquadrant involvement.2 In the 2005 edition of the World Health Organization (WHO) classification of odontogenic tumors, osseous dysplasia is classified into four groups: periapical osseous dysplasia (POD), focal osseous dysplasia, florid osseous dysplasia (FOD), and familial gigantiform cementoma.3 The classification is based on the location of the lesion. FOD is a widespread form of POD. If POD is seen in three or four quadrants, it is usually considered to be FOD.1
FOD is frequently found in middle-aged black women, but it can sometimes be observed in Caucasians and Asians.4,5 In addition, a familial distribution can be seen.6 The cause of FOD is still unknown.7 FOD is often asymptomatic and may be identified on routine dental radiographs.8-10 FOD lesions that are not infected do not require any treatment procedure. The lesions have a poor vascular supply; therefore, they tend towards infection and may not be treated with antibiotics.1,11,12 Mucosal ulceration, fistula formation with suppuration, and pain could be signs of a secondarily infected lesion. In such instances, surgical debridement and enucleation is required.12
Histologically, these lesions consist of normal bone trabeculae, cementum-like calcifications, and fibrous connective tissue.4,9 An avascular cementum-like lesion replaces normal vascular bone in the affected area.10
The classic radiographic appearance is amorphous, lobulated, and mixed radiolucent and radiopaque masses (cotton-wool appearance) with a sclerotic border in the jaws.12 Mature lesions appear more radiopaque than early-stage lesions and have the soft tissue capsule.1 FOD is usually bilateral and symmetric.8 FOD is localized to the root apices of teeth and the teeth associated are vital.9 The lesion can cause loss of the lamina dura.5 Radiological examination plays a vital role in diagnosing these lesions. Panoramic radiographs exhibit a multiquadrant appearance that is characteristic of these radiopaque masses. Three-dimensional (3D) radiological imaging modalities like cone-beam computed tomography (CBCT) provide more detailed information by virtue of their ability to produce axial, coronal, and sagittal views.
This report described the clinical, histopathological, and radiological features of FOD. Our aim in presenting this case report was to highlight the importance of imaging in the diagnosis of FOD.
A 42-year-old female patient was admitted to the Department of Dentomaxillofacial Radiology, Faculty of Dentistry, Ankara University with a complaint of bleeding on the gums. The patient's medical history included having undergone treatment for pernicious anemia and a gastric ulcer two years earlier. On intraoral examination, the patient was asymptomatic except for a few restored and missing teeth.
A lesion was found incidentally on routine periapical radiographs taken for the restored teeth and edentulous areas (Fig. 1). Radiopaque masses were coincidentally observed in the periapical radiographs but the exact boundaries of the masses could not be seen. For further and more detailed examination, cone-beam computed tomography (CBCT) and a panoramic radiograph were taken. The panoramic radiograph and CBCT revealed maxillary bilateral and symmetrical, well-defined, round, radiopaque masses in contact with the root of the maxillary right second molar and left first molar teeth. Lobular, irregularly shaped radiopacities with clear radiolucent demarcation were also present in the right edentulous mandibular molar area (Figs. 2 and 3). The bucco-lingual aspects of the lesions were best visualized on the axial CBCT image (Fig. 4). CBCT added valuable radiographic information regarding the relationships of the lesions with significant anatomical structures, cortical plates, and tooth roots. After ethyl chloride application, the teeth were found to be vital. The overlying mucosa and gingiva had no signs of inflammation. A diagnostic biopsy was taken from the right mandibular molar area under local anesthesia. The obtained specimen was sent for a histopathological examination. Dirty yellow, bone-hard tissues of 1 cm×1 cm×0.6 cm dimensions were analyzed in this examination. On the basis of the histopathologic findings, the tumor was diagnosed as FOD (Fig. 5). Because of the asymptomatic nature of the tumor, no further treatment was proposed. The patient was advised to have routine follow-up examinations at six-month intervals. The patient has been encouraged to maintain an effective oral hygiene program. The case has been followed up over the last 14 months and has remained asymptomatic.
Osseous dysplasias (periapical, focal, florid osseous dysplasias, and familial gigantiform cementoma) are a group of disorders that involve the same pathological processes.10 The clinical and radiological features of osseous dysplasia help to distinguish these lesions from others. POD is mostly confined to the anterior mandible, within the space between the canines.8 FOD is a widespread form of POD and is a single lesion.1,5 The differential diagnosis of FOD includes Paget's disease, chronic osteomyelitis, and Gardner's syndrome.1,10 Paget's disease is often polyostotic and shows changes in the level of serum calcium, phosphorous, and alkaline phosphatase.1,2,10 Gardner's syndrome may involve jaw bone changes similar to those with FOD, but FOD does not show any of the other skeletal changes that are seen in Gardner's syndrome.10
Chronic osteomyelitis is a primary infection of the mandible presenting with unilateral pain, soft tissue swelling, fever, and lymphadenopathy.8,10 The secondarily infected lesion of FOD has a wider radiolucent border than chronic osteomyelitis.1 Steven et al reported a case that was diagnosed as chronic osteomyelitis with underlying infected FOD.8
MacDonald-Jankowski published a systematic review on FOD in 20036 that reviewed 158 cases, the mean age of which was 49 years. Half of these cases had pain, swelling, and pus discharge/fistula with the frequencies of 52%, 31%, and 18%, respectively. FODs can affect several areas of the jaws: posterior mandible area (99%), posterior maxilla (73%), anterior mandible (64%), and anterior maxilla (36%). The study stated that 97% of the cases were female patients. The FOD features observed in the present case report were in accordance with the results of that study.
FOD may cause bone expansion and facial deformity. Ong and Siar provided their patient with surgical treatment to reduce the mass of the swellings.2 In rare cases, FOD can be a hereditary condition with an autosomal dominant familial heredity.4 In our case, no familial aspect was observed.
Gündüz et al7 reported a case of FOD in which the lesion was seen throughout the alveolar processes of all quadrants of the maxilla and the mandible. The location of our case was similar to that of their case. The lesion was identified in three quadrants of the jaws in our case.
While some reports have described diagnosing FOD by clinical and radiological evaluation,5,7,10,13 others performed a biopsy.4,8,12 In the present case, a biopsy was also taken to confirm the diagnosis.
In line with the various other reported cases, our patient was asymptomatic and the lesion was noticed incidentally on periapical radiographs taken for other purposes.4,5,7,10,13
Up to now, two cases diagnosed by CT have been reported in the literature7,13 CBCT images are useful diagnostic tools for identifying the location and extent of the lesion. CBCT can be utilized to discriminate FOD from lesions that display a similar sclerotic appearance on panoramic and periapical radiography.7 Unlike the previous reports, in the diagnosis of the present case, not only clinical and radiological methods but also histological methods were used. The precise histological diagnosis was made in the light of the radiological examinations.
Clinicians should know the properties of such lesions and should be aware of their radiographic appearance. Periapical radiographs may be insufficient to determine multifocal localization and the limits of the lesion. Therefore, panoramic radiographs and CT images are preferable for a broader and more detailed examination. FOD does not require treatment as long as it is asymptomatic. However, when infection of the lesion, resulting from trauma occurs, it requires surgical debridement and enucleation since antibiotics may not be effective due to the avascular nature of the lesion.
Figures and Tables
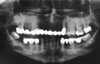 | Fig. 2A panoramic radiograph shows the mixed radiolucent/radiopaque masses with a cotton-wool appearance and with the entire border in three quadrants. |
 | Fig. 3CBCT cross-sectional images reveal the relationship between the lesion and the structures around the lesion, which is a radiopaque conglomerate separate from the bone with a radiolucent border. |
References
1. White SC, Pharoah MJ. Oral radiology: principles and interpretation. 6th ed. St. Louis: Mosby/Elsevier;2000. p. 437.
2. Ong ST, Siar CH. Florid cemento-osseous dysplasia in a young Chinese man. Case report. Aust Dent J. 1997; 42:404–408.

3. Barnes L, Eveson JW, Reichart P, Sidransky D. Pathology and genetics of head and neck tumours. World Health Organization Classification of tumours. Lyon: IARC Press;2005. p. 323.
4. Gonçalves M, Píspico R, Alves Fde A, Lugão CE, Gonçalves A. Clinical, radiographic, biochemical and histological findings of florid cemento-osseous dysplasia and report of a case. Braz Dent J. 2005; 16:247–250.

5. Dağıstan S, Tozoğlu Ü, Göregen M, Çakur B. Florid cemento-osseous dysplasia: a case report. Med Oral Patol Oral Cir Bucal. 2007; 12:E348–E350.
6. MacDonald-Jankowski DS. Florid cemento-osseous dysplasia: a systematic review. Dentomaxillofac Radiol. 2003; 32:141–149.

7. Gündüz K, Avsever H, Karaçaylı Ü, Senel B, Pişkin B. Florid cemento-osseous dysplasia: a case report. Braz Dent J. 2009; 20:347–350.

8. Singer SR, Mupparapu M, Rinaggio J. Florid cemento-osseous dysplasia and chronic diffuse osteomyelitis: report of a simultaneous presentation and review of the literature. J Am Dent Assoc. 2005; 136:927–931.
9. Minhas G, Hodge T, Gill DS. Orthodontic treatment and cemento-osseous dysplasia: a case report. J Orthod. 2008; 35:90–95.

10. Jerjes W, Banu B, Swinson B, Hopper C. Florid cemento-osseous dysplasia in a young Indian woman. A case report. Br Dent J. 2005; 198:477–478.

11. Worawongvasu R, Songkampol K. Fibro-osseous lesions of the jaws: an analysis of 122 cases in Thailand. J Oral Pathol Med. 2010; 39:703–708.

12. Bencharit S, Schardt-Sacco D, Zuniga JR, Minsley GE. Surgical and prosthodontic rehabilitation for a patient with aggressive florid cemento-osseous dysplasia: a clinical report. J Prosthet Dent. 2003; 90:220–224.

13. Beylouni I, Farge P, Mazoyer JF, Coudert JL. Florid cemento-osseous dysplasia: report of a case documented with computed tomography and 3D imaging. Oral Surg Oral Med Pathol Oral Radiol Endod. 1998; 85:707–711.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download