Abstract
Materials and Methods
A total of 54 patients diagnosed with clinical BPH underwent transurethral prostate resection to address their primary urological problem. All patients were evaluated by use of a comprehensive medical history and rectal digital examination. The preoperative evaluation also included serum prostate-specific antigen (PSA) measurement and ultrasonographic measurement of prostate volume. Prostate cancer was detected in one patient, who was then excluded from the study. We performed conventional cytogenetic analyses of short-term cultures of 53 peripheral blood samples obtained from the BPH patients.
Results
The mean (±standard deviation) age of the 53 patients was 67.8±9.4 years. The mean PSA value of the patients was 5.8±7.0 ng/mL. The mean prostate volume was 53.6±22.9 mL. Chromosomal abnormalities were noted in 5 of the 53 cases (9.4%). Loss of the Y chromosome was the most frequent chromosomal abnormality and was observed in three patients (5.7%). There was no statistically significant relationship among age, PSA, prostate volume, and chromosomal changes.
Conclusions
Loss of the Y chromosome was the main chromosomal abnormality found in our study. However, this coexistence did not reach a significant level. Our study concluded that loss of the Y chromosome cannot be considered relevant for the diagnosis of BPH as it is for prostate cancer. Because BPH usually occurs in aging men, loss of the Y chromosome in BPH patients may instead be related to the aging process.
Benign prostatic hyperplasia (BPH) is one of the most common diseases found in adult men [1]. BPH is characterized by the proliferation of smooth muscle cells and epithelial cells within the prostatic transition zone [1]. The exact etiology and mechanisms underlying BPH development and progression are still unknown [12]. Alteration of hormonal levels, permanent chronic inflammation, abnormal wound repair processes, and prostate stem or progenitor cell expansion are the main factors that promote BPH [2].
Because of the difficulty of culturing prostatic epithelial cells, cytogenetic information about malignant and benign prostatic tumors is limited. In recent years, cytogenetic studies have focused on prostate cancer; however, a variety of specific chromosomal changes have been identified in several benign neoplasms [3].
In this study, 54 patients diagnosed with clinical BPH underwent transurethral prostate resection (TUR-P) to address their primary urological problem. All patients were evaluated by use of a comprehensive medical history and digital rectal examination. The preoperative evaluation also included serum prostate-specific antigen (PSA) measurement and ultrasonographic measurement of prostate volume. Prostate biopsies were performed if necessary. After blood samples were obtained for cytogenetic analysis, TUR-P procedures were performed and pathologic specimens were examined. Prostate cancer was detected in one patient, who was then excluded from the study. We performed conventional cytogenetic analyses of short-term cultures of 53 peripheral blood samples obtained from patients with histologically diagnosed BPH.
A 5-mL blood sample was collected from each of the 53 BPH patients. Standard-protocol chromosomal investigations were then performed on peripheral blood lymphocyte cultures. The cells were cultured in Roswell Park Memorial Institute (RPMI) culture media (Sigma-Aldrich, St. Louis, MO, USA; 5 mL of RPMI 1640 with 10% fetal calf serum, 5 µg/mL of phytohemagglutinin, 100 U/mL of penicillin, 100 µg/mL of streptomycin, 2mM of L-glutamine) for 72 hours, at which point the cells were harvested. Hypotonic treatment of the cells was performed in 0.075 M KCI for 20 minutes at 37℃. The cells were then washed in a fixative solution (3:1, methanol/glacial acetic acid) overnight and dropped onto clean slides. Preparations were stored at -20℃. The chromosomes were analyzed at a band resolution of 450-550. For each patient, 20 metaphase plates were analyzed by G-banding by use of automated karyotyping software (CytoVision, Leica Biosystems, USA). All chromosomal abnormalities were reported in accordance with the current international standard nomenclature [8].
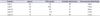
The mean (±standard deviation) age of the 53 patients was 67.8±9.4 years. The mean PSA value of the patients was 5.8±7.0 ng/mL. The mean prostate volume was 53.6±22.9 mL. Chromosomal abnormalities were noted in 5 of the 53 cases (9.4%). Loss of the Y chromosome was the most frequent chromosomal abnormality (3 patients, 5.7%). The other two cases had abnormalities of the 22nd chromosome (46, XY, 22pss) and the 13th chromosome (46, XY, 13ps+), respectively (Table 1, Fig. 1). There was no statistically significant relationship between age (p=0.40), PSA (p=0.23), prostate volume (p=0.66), and chromosomal changes.
BPH and prostate adenocarcinoma are two common prostatic diseases in aging men. The molecular mechanisms underlying BPH development and progression are not fully understood. Many factors, including hormone level alterations, sustained chronic inflammation, aberrant wound repair processes, and prostate stem/progenitor cell expansion could promote BPH [29].
Cytogenetic abnormalities have been reported in approximately 1,000 epithelial tumors, and a small number of characteristic changes have been identified in these tumors, particularly in tumors of the breast, lung, and prostate [10]. The frequency of chromosome instability in circulating peripheral blood lymphocytes is a relevant biomarker for susceptibility to cancer in humans [111213]. Moreover, chromosome instability has been found in many benign lesions [3].
Chromosomal changes in normal prostatic tissue and in BPH tissue have been investigated in few studies in contrast to prostate cancer tissues. Gu et al. [14] analyzed telomerase-immortalized cell lines from the tissues of 5 patients. Of these, 3 were patients with prostate cancer and 2 were patients with BPH. Y loss was observed in all; however, loss of chromosomes 8 and 13 was observed only in prostate cancer cell lines [14]. Nadal et al. [15] investigated Y loss and its possible implication in the tumorigenic process of the prostate and analyzed the prostatic tissues of 28 prostate cancer patients who underwent surgery and tissue from the normal prostate of 4 four organ donors with no clinical history of cancer. Prostatic tissues obtained from prostate cancer patients were grouped as tumoral and nontumoral tissues. Y loss was detected in 52.9% of tumoral tissue samples and in 26.9% of nontumoral tissue samples. However, Y loss was not detected in donor prostatic tissues in this study [15].
Data are limited about the chromosomal changes found in BPH. Aly et al. [5] investigated 28 tissue samples of BPH patients who underwent TUR-P, adenomectomy, or cystectomy for bladder cancer by conventional cytogenetic analysis and found Y loss in 9 (32.1%) and trisomy 7 in 3 patients. Those authors suggested that Y loss may contribute to the development of prostate cancer [5]. Casalone et al. [6] analyzed cell cultures of 10 cases of BPH and observed chromosomal abnormalities in 5 of the 10 cases (50%). In all 5 abnormal cases, loss of the Y chromosome was present. The authors concluded that Y loss could also be considered suggestive of a possible progression from BPH with Y loss to adenocarcinoma [6]. Balachandar et al. [4] investigated chromosomal aberrations in peripheral blood lymphocyte cultures from patients clinically presumed to have BPH and reported 13 chromosomal aberrations (chromosomes 1, 6, 8, 13, 16, and 18) in 27 patients. No Y loss was detected in that study [4].
In our study, we successfully investigated peripheral blood samples by conventional cytogenetic analysis of 53 patients with histologically proven BPH who underwent TUR-P. Chromosomal abnormalities were detected in 5 patients (9.4%). Y loss, which was the most common chromosomal abnormality, was detected in 3 patients (5.7%). We thus detected a relatively lower incidence of Y loss than in the studies mentioned above. However, these studies included few BPH patients/tissues; additionally, heterogeneity in the tissues or the techniques used to investigate the chromosomal abnormalities may contribute to these conflicting results. Gu et al. [14] included only two BPH patients. Nadal et al. [15] investigated the nontumor tissues of prostate cancer patients; however, this means that these patients' prostates were not normal and had a tendency to progress to cancer. Another study included prostatic tissues of patients with a diagnosis of bladder cancer [5]. In Balachandar et al's [4] study, only PSA levels were accepted as a criterion for the diagnosis of BPH. The presence of BPH was not confirmed by any pathologic specimens. BPH is a histopathologic definition and thus requires a histopathological examination of prostate tissue samples [16]. PSA cannot be used as an absolute diagnostic indicator for BPH, and any amount of PSA in the blood does not rule out prostate cancer [1718]. Otherwise, in another study, Y loss was detected in prostate cancer cells but not in benign prostatic stromal cells, which is compatible with our results [19]. To our knowledge, we have investigated the largest number of samples of histologically proven BPH patients in the literature and detected a rate of Y loss of 5.7%. Our results suggest that Y loss may not be significantly related with BPH.
In the study conducted by Casalone et al. [6] with an average patient age of 60.7 years, patients who experienced loss of the Y chromosome were on average 71.6 years old. In our study, the average age of all patients was 68 years, and the mean age of patients with loss of the Y chromosome was 78 years. According to these findings, loss of the Y chromosome may also be related to aging. Many studies have shown an age-associated loss of the X chromosome in women and of the Y chromosome in men [20212223]. Guttenbach et al. [24] reported that the Y hypoploidy was very low in patients of all ages, reaching a frequency of 1.34% in men aged 75 to 80 years. They concluded that the frequency of Y hypoploidy increased with age, demonstrating a highly positive linear correlation [22]. Thus, Y chromosome abnormalities may be related to increasing age rather than BPH.
The other chromosomal aberrations observed in our study were at the 22nd chromosome (46, XY, 22pss) in one patient and the 13th chromosome (46, XY, 13ps+) in another patient. Both aberrations also are frequently reported in prostate cancer in the literature [14252627]. It seems that they also may not be related with BPH.
Loss of the Y chromosome was the main chromosomal abnormality found in our study. However, this coexistence did not reach a significant level. We concluded that loss of the Y chromosome cannot be considered relevant for the diagnosis of BPH as it is for prostate cancer. Because BPH usually occurs in aging men, loss of the Y chromosome in BPH patients may be related to the aging process. There is a need for larger, well-designed studies to identify the possible genetic abnormalities underlying BPH etiopathogenesis.
Figures and Tables
References
1. McVary KT, Roehrborn CG, Avins AL, Barry MJ, Bruskewitz RC, Donnell RF, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011; 185:1793–1803.
2. David M, Berman RR, Veltri RW. Development, molecular biology, and physiology of the prostate. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders;2012. p. 2533–2569.
3. Dal Cin P, Van Den Berghe H. Chromosome abnormalities in benign prostatic hyperplasia. In : Petrovich Z, Baert L, editors. Benign prostatic hyperplasia: innovations in management. New York: Springer-Verlag;1994. p. 49–56.
4. Balachandar V, Kumar BL, Devi SM, Sangeetha R, Manikantan P, Kumar SS, et al. Identification of chromosome aberrations among benign prostatic hyperplasia patients in tamilnadu, Southern India. Int J Hum Genet. 2010; 10:159–164.
5. Aly MS, Dal Cin P, Van de Voorde W, van Poppel H, Ameye F, Baert L, et al. Chromosome abnormalities in benign prostatic hyperplasia. Genes Chromosomes Cancer. 1994; 9:227–233.
6. Casalone R, Portentoso P, Granata P, Minelli E, Righi R, Meroni E, et al. Chromosome changes in benign prostatic hyperplasia and their significance in the origin of prostatic carcinoma. Cancer Genet Cytogenet. 1993; 68:126–130.
7. Brothman AR, Lesho LJ, Somers KD, Schellhammer PF, Ladaga LE, Merchant DJ. Cytogenetic analysis of four primary prostatic cultures. Cancer Genet Cytogenet. 1989; 37:241–248.
8. Shaffer LG, McGowan-Jordan J, Schmid M, editors. ISCN 2013: an international system for human cytogenetic nomenclature. Basel: Karger;2013.
9. Roehrborn CG. Benign prostatic hyperplasia: etiology, pathophysiology, epidemiology, and natural history. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders;2012. p. 2570–2610.
10. Mitelman F. Catalog of chromosome aberrations in cancer. 4th ed. New York: Wiley;1991.
11. Hagmar L, Bonassi S, Stromberg U, Brøgger A, Knudsen LE, Norppa H, et al. Chromosomal aberrations in lymphocytes predict human cancer: a report from the European Study Group on Cytogenetic Biomarkers and Health (ESCH). Cancer Res. 1998; 58:4117–4121.
12. Bonassi S, Abbondandolo A, Camurri L, Dal Pra L, De Ferrari M, Degrassi F, et al. Are chromosome aberrations in circulating lymphocytes predictive of future cancer onset in humans? Preliminary results of an Italian cohort study. Cancer Genet Cytogenet. 1995; 79:133–135.
13. Jellinghaus W, Okada K, Ragg C, Gerhard H, Schröder FH. Chromosomal studies of human prostatic tumors in vitro. Invest Urol. 1976; 14:16–19.
14. Gu Y, Li H, Miki J, Kim KH, Furusato B, Sesterhenn IA, et al. Phenotypic characterization of telomerase-immortalized primary non-malignant and malignant tumor-derived human prostate epithelial cell lines. Exp Cell Res. 2006; 312:831–843.
15. Nadal M, Pera G, Pujadas J, Abril J, Gonzalez L, Aguilo F, et al. Aneuploidy of chromosome Y in prostate tumors and seminal vesicles: a possible sign of aging rather than an indicator of carcinogenesis? Mol Carcinog. 2007; 46:543–552.
16. Donnell RF. Benign prostate hyperplasia: a review of the year's progress from bench to clinic. Curr Opin Urol. 2011; 21:22–26.
17. Mottet N, Bastian PJ, Bellmunt J, van den Bergh RC, Bolla M, van Casteren NJ, et al. Guideline on prostate cancer. Anheim (NL): European Association of Urology;2014.
18. Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015; 67:1099–1109.
19. Van Dekken H, Alers J. Loss of chromosome Y in prostatic cancer cells but not in stromal tissue. Cancer Genet Cytogenet. 1993; 66:131–132.
20. Catalan J, Autio K, Kuosma E, Norppa H. Age-dependent inclusion of sex chromosomes in lymphocyte micronuclei of man. Am J Hum Genet. 1998; 63:1464–1472.
21. Stone JF, Sandberg AA. Sex chromosome aneuploidy and aging. Mutat Res. 1995; 338:107–113.
22. Guttenbach M, Koschorz B, Bernthaler U, Grimm T, Schmid M. Sex chromosome loss and aging: in situ hybridization studies on human interphase nuclei. Am J Hum Genet. 1995; 57:1143–1150.
23. Fitzgerald PH, McEwan CM. Total aneuploidy and age-related sex chromosome aneuploidy in cultured lymphocytes of normal men and women. Hum Genet. 1977; 39:329–337.
24. Guttenbach M, Schakowski R, Schmid M. Aneuploidy and ageing: sex chromosome exclusion into micronuclei. Hum Genet. 1994; 94:295–298.
25. Brothman AR, Maxwell TM, Cui J, Deubler DA, Zhu XL. Chromosomal clues to the development of prostate tumors. Prostate. 1999; 38:303–312.
26. Christensen GB, Baffoe-Bonnie AB, George A, Powell I, Bailey-Wilson JE, Carpten JD, et al. Genome-wide linkage analysis of 1,233 prostate cancer pedigrees from the International Consortium for Prostate Cancer Genetics using novel sumLINK and sumLOD analyses. Prostate. 2010; 70:735–744.
27. Sun J, Zheng SL, Wiklund F, Isaacs SD, Li G, Wiley KE, et al. Sequence variants at 22q13 are associated with prostate cancer risk. Cancer Res. 2009; 69:10–15.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download