Abstract
Periprosthetic joint infection (PJI) due to Salmonella is rare. It frequently occurs patients receiving immunosuppressive medicine. We describe two periprosthetic Salmonella infection of two immunocompromised patients. Both of patients were receiving azathioprine and prednisolone therapy. First patient presented six years after total hip arthroplasty with a huge abscess on her right thigh that was reached to femoral component through the lytic area of lateral femur. Second patient presented with drainage from his hip and he had undergone two-step revision surgery for PJI 3 months ago. There is no consensus in the treatment of periprosthetic salmonella infections. We prefer two-step revision surgery for these infections as previously described in the literature.
The rate of periprosthetic infection after total hip arthroplasty (THA) is reported to be 1-2%1). These infections are associated with an increase in hospital stay, need for repeat surgery, increase in costs, long-term antibiotic use, and decreased quality of life2). While isolated organisms are most commonly Gram-positive cocci, rarely Gramnegative bacteria are also reported as causative organisms2). Periprosthetic joint infections (PJIs) due to Salmonella are rare with only 30 cases reported in the literature3). The incidence of Salmonella infection increases in patients with sickle cell anemia, collagen vascular diseases, alcoholism, malignancies, immunosuppression, and past history of gastrointestinal system surgeries. Also the infections caused by Salmonella, the spread of the infection is hematogenous45).
There is no consensus in the literature as to whether periprosthetic Salmonella infections should be treated with one or two-step revision surgery4). There are reports of success with both treatment modalities6). We aimed to present two patients with immunosuppression due to azathioprine and prednisolone treatments who had PJIs caused by Salmonella and were treated with two-step revision surgery.
A woman aged 59 years presented with severe pain and swelling in her right thigh with a history of femoral head avascular necrosis due to steroid use and subsequent right THA in our clinic. The patient was under azathioprine 50 mg once a day and prednisolone 2 mg once a day treatments at that time for pemphigus vulgaris treatment was started for 6 months before THA. After asymptomatic 6 years, once again she had right hip pain for the last two months, which had recently increased. On presentation there was swelling, redness, and a temperature increase in the right thigh. Her temperature was 37.8℃. Her right hip joint was tender with movement and there was a fluctuating mass in the right thigh. Bloodcount showed erythrocyte sedimentation rate (ESR), 99 (0-20 normally) mm/hour; C reactive protein (CRP), 101 (0-5 normally) mg/L; white blood cell count (WBC), 12,100/µL (4,100-11,200/µL normally); neutrophil count (Neu), 10,400/µL (86.4%). Aspiration of the fluctuating mass in the right thigh yielded a yellow green purulent exudate. Consequently, thigh magnetic resonance imaging (MRI) was ordered. The MRI (Fig. 1) showed an abscess in the right thigh with dimensions of 138×83×68 mm, which was urgently treated with percutaneous drainage. A single drain was placed. The material culture was positive for Salmonella typhimurium (Fig. 2) and it was consulted with Department of Infectious Diseases. Ciprofloxacin 400 mg twice a day intravenously (IV) was started. Right hip computed tomography (CT) showed that the abscess in the thigh reached the prosthesis through a lytic area in the lateral femur (Fig. 3) and thus the decision was made for two-step revision surgery. In the first stage, peroperative debridement was performed and components were removed. The femoral and acetabular components were noticed to be loosened. A spacer with antibiotic (gentamycin) and cement with vancomycin was placed. After ciprofloxacin 400 mg twice a day treatment for a total of 5 weeks, CRP levels were back to normal. There was no discharge or drainage from the wound. The patient was referred to the Department of Infectious Diseases and was put on oral antibiotics. The treatment of oral ciprofloxacin 400 mg once a day was completed for four months and CRP was 3 mg/L, ESR 13 mm/hour, WBC 9,300/µL determined and decided to second step revision surgery. The surgery was performed after six months first step revision (Fig. 4). The patient was followed up for sixteen months and had no pain or complaint with the operated hip.
A man aged 64 years presented to our clinic with oozing from his hip following drainage of a two-step revision surgery. He had a history of bilateral THA due to bilateral femoral head avascular necrosis after prednisolone and azathioprine treatments for vasculitic neuropathy three years ago. The patient was started to use prednisolone and azathioprine for four years before the bilateral THA. The patient underwent two-step revision surgery for a left PJI after undergoing 3 debridement procedures in another hospital one year ago. At the time of presentation his preoperative laboratory examinations were CRP, 59 mg/L; WBC, 8,800/µL (63.9% Neu); ESR, 101 mm/hour. He had pain on his left hip pain with hip motion (Fig. 5). He did not have fever. The patient was scheduled for another two-step revision surgery after being diagnosed as having a periprosthetic hip infection. In the first step, the components were removed, the infection site was debrided, and a spacer with antibiotics was placed. Samples retrieved peroperatively yielded positive culture result Salmonella type C and patient was thus put on cefazolin 1 g four times a day IV and ciprofloxacin 400 mg twice a day IV and he use them for perform to second step revision. His stool and blood cultures were negative. With the decrease of acute-phase reactants, the patient was discharged after consulting the Department of Infectious Diseases. The patient developed no concomitant pathologies during follow-up and therefore underwent the second step of the revision surgery 5 months later. CRP was 4 mg/L, ESR 22 mm/hour, WBC 7,200/µL determined and decided to second step revision surgery. The surgery was performed after 5 months first step revision. The patient was followed up for 27 months and had no pain or complaint with the operated hip (Fig. 6).
PJIs are among the morbid complications of hip arthroplasty2). The most common causative organisms of periprosthetic infections are Gram-positive cocci2). Infections may have a subclinical course especially in immunosuppressed patients and who may be infected with organisms rarely encountered in clinical practice7). Salmonella spp. is a Gram-negative rod in the Enterobacteriaceae family and although the primary infection source is animals, it can also spread from humanto-human with a fecal-oral route, the causative organisms of 4% of all PJI5). Salmonella presents with different symptoms and signs in clinical practice. It most commonly presents with gastroenterities and is seen in 68.3% of cases; however, no gastrointestinal symptoms were present in our patients. It has a self-limiting course and antibiotic treatment is rarely indicated. Gastrointestinal carriage is another presentation; bacteria are released into the gastrointestinal system months to years after the gastroenteritis episode. The rarer but more serious presentation is bacteremia and focal infections. Focal infections usually develop after bacteremia and can be seen in differents parts of the body35). There is no consensus in the treatment of periprosthetic Salmonella infections; however, treatment includes surgery and antibiotics46). Ampicillin, chloramphenicol, trimethoprim sulfamethoxazole, amoxicillin, third-generation cephalosporins and quinolones are proven to be effective in Salmonella infections5). It remains contentious as to whether surgical intervention is required in the treatment, and further, whether surgery should be performed in one or two steps678). In a study by Day et al.6) with 12 periprosthetic Salmonella infections, 9 patients underwent revision surgeries and 3 had suppressive antibiotic therapy after the first step. In this group, recurrence occurred in one patient. Kobayashi et al.8) reported successful results in bilateral knee prosthesis infections with debridement, irrigation, and antibiotic treatment. However, there are studies with conflicting results. Gupta et al.9) gave antibiotic suppression to 4 out of the 6 patients with periprosthetic Salmonella infections in their series without first revising the prothesis. They then performed two-step revision to all patients because of infection recurrence9). Tóth et al.10) reported successful results of two-step revision after Salmonella infection in their case report of 2 patients. They suggested that one-step revision may be an option for periprosthetic infections caused by other organisms but usually not recommended for infections caused by Salmonella10). We also prefer two-step surgery for Salmonella-infected arthroplasties, as reported in the literature. Although Salmonella infections are rarely seen after hip arthroplasty, this infection must be in differential diagnosis in patients with comorbidities. Two-step surgery is applicable in the treatment of Salmonella infections.
Infections may have a subclinical course especially in immunosuppressed patients and who may be infected with organisms rarely encountered in clinical practice. Salmonella infections are rarely seen after hip arthroplasty. The aim of this case report is that to raise awareness the fact that Gram negative organisms should be kept in mind especially in immunosuppressive patients using azathioprine.
Figures and Tables
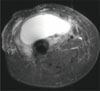 | Fig. 1Magnetic resonance imaging showed a huge abscess in the right thigh, which was urgently treated with percutaneous drainage. |
 | Fig. 3The X-ray (A) and computed tomography (B) images showed that huge abscess on the right thigh had reached to femoral component through the lytic area of lateral femur related to periprostetic joint infection. |
 | Fig. 4Postoperative X-ray after first step (A) and second step (B) revision surgery for periprostetic joint infection. Second step surgery was performed after 15 months. |
ACKNOWLEDGEMENTS
The authors would like to acknowledge Department of Orthopedics and Traumatology, Istanbul University Faculty of Medicine.
References
1. Zimmerli W, Ochsner PE. Management of infection associated with prosthetic joints. Infection. 2003; 31:99–108.

2. Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008; 466:1710–1715.

3. de la Torre B, Tena D, Arias M, Romanillos O. Recurrent prosthetic joint infection due to Salmonella enteritidis: case report and literature review. Eur J Orthop Surg Traumatol. 2012; 22:Suppl 1. 89–97.

4. Oe K, Wada T, Ohno H, Kushida T, Iida H. Salmonella septic arthritis following total knee arthroplasty for rheumatoid arthritis in a patient receiving etanercept. J Orthop Sci. 2011; 16:258–262.

5. Cohen JI, Bartlett JA, Corey GR. Extra-intestinal manifestations of Salmonella infections. Medicine (Baltimore). 1987; 66:349–388.

6. Day LJ, Qayyum QJ, Kauffman CA. Salmonella prosthetic joint septic arthritis. Clin Microbiol Infect. 2002; 8:427–430.

7. McDonald DJ, Fitzgerald RH Jr, Ilstrup DM. Two-stage reconstruction of a total hip arthroplasty because of infection. J Bone Joint Surg Am. 1989; 71:828–834.

8. Kobayashi H, Hall GS, Tuohy MJ, Knothe U, Procop GW, Bauer TW. Bilateral periprosthetic joint infection caused by Salmonella enterica serotype Enteritidis, and identification of Salmonella sp using molecular techniques. Int J Infect Dis. 2009; 13:e463–e466.

9. Gupta A, Berbari EF, Osmon DR, Virk A. Prosthetic joint infection due to Salmonella species: a case series. BMC Infect Dis. 2014; 14:633.
10. Tóth K, Janositz G, Kovács G, Sisák K, Rudner E. Successful treatment of late Salmonella infections in total hip replacement-report of two cases. BMC Infect Dis. 2010; 10:160.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download