Abstract
PURPOSE
The aim of this study was to evaluate whether the push-out bond strength varies between oval and circular fiber posts, and to examine the effect on the resin cement thicknesses around the posts.
MATERIALS AND METHODS
Eighteen mandibular premolar roots were separated into two groups for oval and circular fiber posts systems. Post spaces were prepared and fiber posts were luted to the post spaces. Roots were cut horizontally to produce 1-mm-thick specimens. Resin cement thicknesses were determined with a metallographic optical microscope and push-out tests were done.
For ensuring post-endodontic restorations which provide tooth function and form with adequate force distribution, placement of fiber posts to the root canal are used commonly.1 Moreover, the placement of a post is often needed for the restoration of a root canal treated tooth in order to support the core material.2,3 Due to the requirement for aesthetics, circular fiber posts have recently gained popularity and these materials are developed gradually.2 The lack of adaptation of the circular posts to the canal walls are filled with resin cements. But, the major factor for clinical performance of the post supported restorations is cement thickness.4
Adhesive failures associated with fiber posts are common and usually happens along the resin cement that fills the post-dentin interface.5 Although the ideal thickness of the resin cement needed to improve retentive bond strength is unknown, the fit of the fiber posts into the post spaces should be as tight as possible.6 Ovoid shaped fiber posts have recently been introduced because of the clinical problems in oval-shaped canals, especially in canines and mandibular premolars.7 Oval fiber posts are produced to mimic the oval-shaped canals, thus it can be a better fit to the post-spaces.7,8
The present study evaluated whether the push-out bond strength to dentin varies between oval and circular fiber posts, and how the resin cement thickness around oval and circular fiber posts cemented into oval shaped canals differed. The first null hypothesis of the current study was that the push-out bond strength is not significantly different circular versus oval fiber posts in ovoid root canals. The second null hypothesis of the current study was that the resin cement thickness is not significantly different circular versus oval fiber posts in ovoid root canals.
Eighteen human mandibular first premolars with similar size that was free of restoration and caries, and that had been stored in normal saline solution immediately after extraction, were used in this study. First, the root canals were determined as ovoid shape when the ratio of the bucco-lingual to mesio-distal root canal diameter, calculated at 5 mm from the apex, was ≥2, as described by Wu et al.9 In addition, all teeth were scanned with a cone-beam computerized tomography (NewTom 5G FP, Verona, Italy) to identify the oval-shaped root canals. Finally, 18 teeth with ovalshaped canals were included to this in vitro research. External debris on the teeth was removed with a cavitron (Cavitron; Dentsply, York, PA, USA) and the root surfaces were gently scraped with curettes to clean periodontal ligament remnants. The crowns of the teeth were removed at the cemento-enamel junction with a slow-speed diamond saw (Isomet; Buehler, Lake Bluff, IL, USA) under water cooling. The root canal lengths were standardized by cutting the roots to a uniform length of 14 mm. The working length was adjusted 1 mm away from the anatomic apex. The root canals were prepared with ProTaper Ni-Ti rotary instruments (Dentsply Maillefer, Ballaigues, Switzerland) up to ProTaper F3 instrument. Irrigation was performed using 5 mL of 2.5% NaOCl between each instrument during the cleaning and shaping of the root canal. The final irrigation was performed using 5 mL of 17% ethylenediaminetetraacetic acid (EDTA) for 1 minute, followed by copious irrigation with distilled water. After drying with paper points, the root canal treatments were done with a cold lateral condensation technique using gutta-percha (Dentsply Maillefer, Petropolis, RJ, Brazil) and resin sealer (AH Plus; Dentsply DeTrey GmbH, Konstanz, Germany). The pulp chambers of the roots were temporarily filled with Cavit (3M ESPE AG, Seefeld, Germany), and the roots were stored at 37℃, 100% humidity for 7 days.
After storage, roots were randomly separated into two groups for oval and circular fiber posts (n=9) and the procedures mentioned below were done by one operator in a standardized procedure.
Group 1: A #2 Gates Glidden bur (Mani Inc., Tochigi, Japan) was used to remove the gutta-percha and the post spaces were all prepared with special preparation drills (D.T. #0.5 and D.T. #2, Bisco Inc., Schaumburg, IL, USA) to a depth of 10 mm from the cemento-enamel junction under continuous water cooling from a handpiece (25 mL/min). Root canals were lubricated with a 2.5% NaOCl irrigation solution between each drill. The drill speed was set at 8000 rpm.
Group 2: A #2 Gates Glidden bur was used to remove the gutta-percha (Mani Inc.) and an oval-shaped medium-grit (76-µm) diamond-coated ultrasonic tip (Ellipson tip; RTD/Satelec, Merigcac, France) that was mounted on an ultrasonic unit (Satelec P5 Newtron XS; Acteon Group, Mount Laurel, NJ, USA) at medium power until a 10-mm post space was obtained. Incessant water cooling from a handpiece (25 mL/min) was used at the entire stages of the preparations.
The oval fiber posts (with an apical width and thickness dimensions are 1.1 and 0.5 mm, respectively; whereas the bucco-lingual dimension is 1.9 mm, and mesio-distal dimension is 1.1 mm cervically) and circular fiber posts (with an apical diameter of 1 mm; and cervical diameter of 1.8 mm) were then luted with dual-polymerizing luting agent (Panavia F 2.0, Kuraray, Japan) to the post spaces. The posts were cleaned properly with alcohol, rinsed with distilled water, and air-dried.
The ED Primer II (Kuraray, Japan) was mixed at a ratio of 1 : 1, applied to the dentin walls of the post spaces using a microbrush (Microbrush X, Microbrush Corp, Grafton, WI, USA) for 30 seconds, and slowly air-dried; the excess was then removed with paper points. Panavia F 2.0 was mixed for 20 seconds and placed in the post spaces using a lentulo spiral filler (Dentsply-Maillefer). Posts were coated with luting cement and gently seated by finger pressure. Excess cement was removed. Cement was polymerized for 40 seconds using a light-polymerizing unit (3M ESPE, Elipar S10, Germany) by placing the light tip perpendicular to the post for 40 seconds. Then, the roots were stored at 37℃, 100% humidity for 7 days before testing.
Each root was cut horizontally with a slow-speed diamond saw (Buehler) to obtain six 1-mm-thick specimens (two apical, two middle, and two cervical). The thickness of each specimen was carefully monitored with a digital caliper. Afterwards, all specimens were examined with an operation microscope (Zeiss, OpmiPico, Germany) to determine any artifacts arised by the slicing process, and no artifacts were observed.
A digital image of each specimen was taken to measure the resin cement thicknesses using a metallographic optical microscope (Leica, Germany) with ×5 magnification. Eight points were determined in each digital image and resin cement thicknesses were measured between the canal wall and the fiber-post perimeter at these points.
Following the resin cement thickness measurement procedures, the push-out tests were done at a cross-head speed of 0.5 mm/min-1 with a universal testing machine (Instron, Canton, MA, USA). Due to the tapered design of the posts, three different sizes of plungers were used for the push-out tests. The diameter of the plunger was 1 mm for the cervical two specimens, 0.5 mm for the two middle specimens, and 0.3 mm for the two apical specimens. This ensured that the plunger only contacted the post during loading. The load needed to dislodge the posts was recorded in Newtons.
The force (F) required to dislodge the fiber posts was transformed into tension (in MPa) by dividing the dislodgement force in Newtons by the interfacial area of the post fragment. Transformation to MPa was calculated differently for the different geometrical shape of the circular and oval fiber posts.
For circular posts that were considered truncated cones, the method used to transform to MPa was similar to that used by Costa et al.10 The upper and lower diameters of the specimens were measured individually, and the following formula was used: Mpa=F/SL. SL was calculated using the following equation: SL=π(R+r)g; where SL=sealer adhesion area; π=3.14; R=mean radius of the cervical post (mm); r=mean radius of the apical post (mm); g=slice thickness (mm). The radius of each specimen was calculated from digital images.
For the oval posts the above formula could not be used because the oval post specimen shape is not considered a truncated cone. The oval post presents a section made up of a rectangle and two equal circular segments. Therefore, a fragment of an oval post was considered as a geometric solid figure made up of a truncated rectangular based pyramid (thicker lines) and two equal parts of a truncated cone. Therefore the lateral surface area was calculated using a method similar to that used by Coniglio et al.7 Two digital images of each specimen were taken from apical and cervical sides using a metallographic optical microscope with ×5 magnification. Then, an image processing software program (Photoshop CS5, Adobe, San Jose, CA, USA) was used to determine points' axis and ordinate as pixel. r1, r2, OH, O'H' HD, H'D', AB, A'B' distances stated in the formula were translated to mm from the pixel format:
where O=The center of the circle of the oval post section; H= the intersection of the major (CF) and minor axis (DE) of the oval post; A, B, D, E= the corners of the oval post section; r1=mean radius of the cervical side of the post (mm); r2=mean radius of the apical side of the post (mm); and O was calculated with an analytical geometry rule which is the center of the circle from three identified points (A, B, C points). The symbol (') indicates the equivalent segments on both sides of the specimen. The other letters in the formula are defined in Fig. 1.
Two separate Kruskal-Wallis ANOVA on ranks were applied to compare the push-out and resin cement thickness data in each canal third. The post hoc analysis was performed with Dunn's method. Mann-Whitney U-tests were done to detect differences between the oval and circular post groups for each canal third. The failure mode data were analysed using the chi-square test. Statistical analyses were performed using SigmaStat software, version 12.0 (Systat Software, San Jose, CA, USA), and the statistical significance was determined as P<.05.
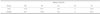
Table 1 is presented to show push-out test results. In terms of the push-out test results of the cervical, middle and apical specimens of the oval and circular fiber-post groups, there were no significant differences among the groups (P>.05).
Comparisons in terms of root segments for the oval fiber-post group revealed that the bond strengths in the apical specimens were lower than in the cervical specimens and the middle specimens (P<.05). The bond strength results in the cervical and middle specimens did not reveal statistically significance (P>.05).
When the bond strengths were evaluated in terms of the root segments for the circular fiber-post group, significantly higher bond strength values were measured in the cervical compared with the apical specimens (P<.05). There were no significant differences between the bond strengths in the cervical and middle specimens and in the middle and apical specimens (P>.05).
The resin cement thicknesses of the oval posts were higher than those of the circular post group in the cervical, middle and apical specimens (P<.05) (Table 2).
Circular posts had a significantly higher resin cement thickness in the cervical third than in the apical and middle thirds (P<.05). In addition, the resin cement layer of the oval posts was thicker in the cervical and apical specimens than in the middle specimen (P<.05).
According to the chi-square test for the failure mode comparisons within the groups no significant differences were revealed (P>.05).The most frequent type of failure mode in all groups was adhesive failure between cement and dentine. Any cohesive failure at the post was not observed (Table 3).
To reflect the root canal morphology after drilling the root canals in oval shaped teeth and to eliminate possible disadvantages of circular fiber posts, oval fiber posts were developed with a minimally invasive diamond-coated ultrasonic tip.8,11 The anatomical, oval Ellipson Fiber Post is formed with a high percentage loading 64% vol. (80% wt.) of pretensed long continuous unidirectional quartz fibers with epoxy resin, and is radiopaque. The Ellipson Post is quite translucent for adequate light transmission. Ellipson post has an elastic modulus of 13 Gpa, and a flexural strength of 1600 MPa, and has no risk of corrosion. The Ellipson tip for the minimally invasive oval preparation with ultrasonic, is stainless steel with a diamond coated tip of 76 micron grain, a diameter of 1.8 mm and has depth gauge markings. This tip can be used to simultaneously remove root canal filling material, clean the canal and shape the canal to adapt the oval Ellipson Fiber Post.12
To assess the bond strength between fiber posts and the root canal dentin, conventional shear and tensile tests, microshear, microtensile, and pull-out and push-out tests have been used.13,14,15,16 It is suggested that the bond strength is better obtained by the push-out test than with the conventional shear test because the fracture occurs parallel to the dentin bonding interface in the push-out test, which makes it a true shear test.13 Chen et al.17 stated that, the stresses concentrate at the filler-loading pin and filler-dentin interfaces in push-out method. Additionally, as premature failures occur during specimen preparation and because of the large data distribution observed in microtensile tests, the push-out test is considered more reliable.15,16,18 The shear stress achieved with the push-out tests is comparable to the stress, under clinical conditions, at the interface between the dentin and the luting cement, as well as between the post and the luting cement.19 According to a previous study, investigators showed the pin diameter, specimen thickness, and elastic modulus of the filling material all affected the push-out bond strength values.17 In the present study, luting resin cement, specimen thickness and pin diameter was set standard; also, oval and circular posts have the same elastic modulus. This situation might be one of the factors that lead to similar push-out results between the groups.
To determine the interfacial area of the circular and oval fiber posts, which have different geometrical shapes, two distinct formulas were applied to calculate the push-out bond strength in megapascals. The interfacial area of the circular fiber-post specimens was calculated as described by Costa et al.,10 whereas a specific formula that was introduced by Coniglio et al.7 was modified in the present study to calculate the interfacial area of the oval fiber-post specimens.
In this study, the push-out bond strengths and resin cement thicknesses of two post systems were evaluated. The push-out bond strengths of the oval and circular fiber posts were not significantly different. Therefore, the results obtained support the first null hypothesis that the push-out bond strengths of the oval and circular fiber posts would not differ significantly in ovoid root canals. These results are in agreement with those of Coniglio et al.,7 who found that the oval tip-oval post system resulted in comparable push-out bond strength values to the circular drill-post system. The results of the study do not support the second hypothesis that the resin cement thickness would not differ significantly whether oval and circular fiber posts were used in ovoid root canals.
Muñoz et al.20 reported no significant difference in resin cement thicknesses between oval and circular fiber posts, whereas Coniglio et al.8 showed that the resin cement thicknesses of oval fiber posts were significantly less than those of circular fiber posts in ovoid root canals. In a recent study, Rengo et al.21 evaluated the volume of luting cement around the oval and circular fiber posts by means of CT imaging in ovoid root canals; and found that there were significantly higher cement thicknesses around oval post group than the circular post group as our study. In the present study, the resin cement thicknesses of the oval fiber posts were significantly greater than those of the circular fiber posts. In our study, the cervical diameter of the circular fiber posts was 1.8 mm, whereas the oval fiber posts had a bucco-lingual dimension of 1.9 mm, and a mesio-distal dimension of 1.1 mm cervically. Further, the apical diameter of the circular fiber posts was 1 mm, and the apical width and thickness dimensions of the oval fiber posts were 1.1 and 0.5 mm, respectively. The explanation for the smaller resin cement thickness of the circular fiber posts in our study may be related to the wider mesial-distal dimension of circular fiber posts compared to oval fiber posts. In addition, the vibration of the medium grit diamond-coated ultrasonic tip used for oval fiber posts might have resulted in a wider post space than the original dimension of the post. Therefore, using the fine grit diamond-coated ultrasonic tip could be recommended for achieving lower resin cement thicknesses.8
The differing results of Muñoz et al.20 and Coniglio et al.8 may be related to the circular fiber post diameters that were not explained clearly in these studies. Additionally, in these studies the post space lengths were 11 and 8 mm, respectively, whereas our study used 10-mm post-space lengths. Furthermore, in our study root canals were prepared using ProTaper system up to F3 instrument. However, Muñoz et al.20 and Coniglio et al.8 prepared narrower root canals in their study, with Protaper F2 and MTwo 25/0.6 as the master apical files, respectively.
In the present study, for both oval and circular fiber posts, the bond strengths in the apical specimens were significantly lower compared to the cervical specimens. Factors possibly affecting the lower bond strengths to root dentin in the apical root specimens could be the non-uniform adaptation of the luting agent or its incomplete polymerization, both related to the difficult access of postspace walls during handling.22
The oval and circular posts used in the current study were both of quartz fiber. The cementation agent used in this study was uniform between the posts. The only criterion that may affect the push-out bond strength is resin cement thickness. Previous studies reported that, regardless of the anatomy of the posts, the resin cement thickness did not affect the push-out bond strength.8,23,24 In the light of the results of the current study, the resin cement thickness in the oval fiber-post group was greater than in the circular fiber-post group, and resin cement thickness did not affect the push-out bond strength.
When considering failure modes after push-out tests, there were no significant difference between groups; in addition, adhesive failure between dentin and cement were the most frequent type; and this shows the weak link between the root dentin and luting cement. The situation might be a result of debris that have remained on canal walls and reduced the bonding. Findings of the present study are in accordance with Scotti et al.'s study.1
Figures and Tables
 | Fig. 1(A) Cervical aspect of circular fiber-post slice (R represents the radius of the circular post). (B) Apical aspect of circular fiber-post slice (r represents the radius of the circular post). (C) Cervical aspect of oval fiber-post slice (A, B, C, D, E, F points were used to determine the distance of AB, OH, HD, radius of ovality [r1]; and, ML, L, DL, D, DB, B, MB, M points were used to measure the resin cement thicknesses). (D) Apical aspect of oval fiber-post slice (A', B', C', D', E', F'points were used to determine the distance of A'B', O'H', H'D', radius of ovality [r2]. |
Table 1
Median (Quartiles) values push-out strengths of oval and circular fiber post groups

| Apical | Middle | Cervical | P | |
|---|---|---|---|---|
| Oval |
3.739a (1.39 - 7.43) |
9.863b (6.58 - 11.77) |
12.639b (7.8 - 14.2) |
<.001 |
| Circular |
4.611a (2.72 - 7.57) |
7.094a.b (5.06 - 9.50) |
10.309b (6.3 - 12.8) |
<.001 |
| P | .361 | .196 | .704 |
Table 2
(Quartiles) values resin cement thicknesses of oval and circular fiber post groups

References
1. Scotti N, Forniglia A, Bergantin E, Paolino DS, Pasqualini D, Berutti E. Fibre post adaptation and bond strength in oval canals. Int Endod J. 2014; 47:366–372.
2. Ho YC, Lai YL, Chou IC, Yang SF, Lee SY. Effects of light attenuation by fibre posts on polymerization of a dual-cured resin cement and microleakage of post-restored teeth. J Dent. 2011; 39:309–315.
3. Kremeier K, Fasen L, Klaiber B, Hofmann N. Influence of endodontic post type (glass fiber, quartz fiber or gold) and luting material on push-out bond strength to dentin in vitro. Dent Mater. 2008; 24:660–666.
4. Grandini S, Goracci C, Monticelli F, Borracchini A, Ferrari M. SEM evaluation of the cement layer thickness after luting two different posts. J Adhes Dent. 2005; 7:235–240.
5. D'Arcangelo C, Cinelli M, De Angelis F, D'Amario M. The effect of resin cement film thickness on the pullout strength of a fiber-reinforced post system. J Prosthet Dent. 2007; 98:193–198.
6. Egilmez F, Ergun G, Cekic-Nagas I, Vallittu PK, Lassila LV. Influence of cement thickness on the bond strength of tooth-colored posts to root dentin after thermal cycling. Acta Odontol Scand. 2013; 71:175–182.
7. Coniglio I, Magni E, Cantoro A, Goracci C, Ferrari M. Push-out bond strength of circular and oval-shaped fiber posts. Clin Oral Investig. 2011; 15:667–672.
8. Coniglio I, Garcia-Godoy F, Magni E, Carvalho CA, Ferrari M. Resin cement thickness in oval-shaped canals: oval vs. circular fiber posts in combination with different tips/drills for post space preparation. Am J Dent. 2009; 22:290–294.
9. Wu MK, R'oris A, Barkis D, Wesselink PR. Prevalence and extent of long oval canals in the apical third. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 89:739–743.
10. Costa JA, Rached-Júnior FA, Souza-Gabriel AE, Silva-Sousa YT, Sousa-Neto MD. Push-out strength of methacrylate resin-based sealers to root canal walls. Int Endod J. 2010; 43:698–706.
11. Cheleux N. The Ellipson concept: an ultrasonic canal preparation combined with an oval fibre post. Int Dent SA. 2008; 3:52–58.
12. Rtd.fr/ellipson.php [Internet]. Saint Egreve: Association of RTD Online Resources Inc.;2004. Available from: www.rtd.fr/ellipson.php.
13. Bitter K, Kielbassa AM. Post-endodontic restorations with adhesively luted fiber-reinforced composite post systems: a review. Am J Dent. 2007; 20:353–360.
14. Ferrari M, Vichi A, Grandini S. Efficacy of different adhesive techniques on bonding to root canal walls: an SEM investigation. Dent Mater. 2001; 17:422–429.
15. Goracci C, Tavares AU, Fabianelli A, Monticelli F, Raffaelli O, Cardoso PC, Tay F, Ferrari M. The adhesion between fiber posts and root canal walls: comparison between microtensile and push-out bond strength measurements. Eur J Oral Sci. 2004; 112:353–361.
16. Schmitter M, Rammelsberg P, Gabbert O, Ohlmann B. Influence of clinical baseline findings on the survival of 2 post systems: a randomized clinical trial. Int J Prosthodont. 2007; 20:173–178.
17. Chen WP, Chen YY, Huang SH, Lin CP. Limitations of push-out test in bond strength measurement. J Endod. 2013; 39:283–287.
18. Mannocci F, Qualtrough AJ, Worthington HV, Watson TF, Pitt Ford TR. Randomized clinical comparison of endodontically treated teeth restored with amalgam or with fiber posts and resin composite: five-year results. Oper Dent. 2005; 30:9–15.
19. Erdemir U, Mumcu E, Topcu FT, Yildiz E, Yamanel K, Akyol M. Micro push-out bond strengths of 2 fiber post types luted using different adhesive strategies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 110:534–544.
20. Muñoz C, Llena C, Forner L. Oval fiber posts do not improve adaptation to oval-shaped canal walls. J Endod. 2011; 37:1386–1389.
21. Rengo C, Spagnuolo G, Ametrano G, Juloski J, Rengo S, Ferrari M. Micro-computerized tomographic analysis of premolars restored with oval and circular posts. Clin Oral Investig. 2014; 18:571–578.
22. Kalkan M, Usumez A, Ozturk AN, Belli S, Eskitascioglu G. Bond strength between root dentin and three glass-fiber post systems. J Prosthet Dent. 2006; 96:41–46.
23. Hagge MS, Wong RD, Lindemuth JS. Effect of dowel space preparation and composite cement thickness on retention of a prefabricated dowel. J Prosthodont. 2002; 11:19–24.
24. Perez BE, Barbosa SH, Melo RM, Zamboni SC, Ozcan M, Valandro LF, Bottino MA. Does the thickness of the resin cement affect the bond strength of a fiber post to the root dentin. Int J Prosthodont. 2006; 19:606–609.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download