Abstract
PURPOSE
Occlusal splints are commonly used to prevent tooth wear caused by bruxism. However, the effects of splints on occlusion are still unclear. Although it is rarely alluded in literature, splints can provoke severe occlusal alterations and other complications. This study was aimed to identify differences in the responses of individuals with bruxism and healthy individuals to a full-arch maxillary stabilization splint in terms of occlusal changes.
MATERIALS AND METHODS
Occlusal contacts in 20 (5 male, 15 female) bruxism patients and 20 (5 male, 15 female) controls with normal occlusion were evaluated before and after occlusal splint therapy. T-Scan III, a computerized occlusal analysis system, was used to simultaneously measure occlusion and disclusion times as well as left-right and anterior-posterior contact distributions before splint therapy and 3 months after therapy. Wilcoxon and Mann-Whitney U tests were used for statistical analyses (α=.05).
RESULTS
No differences were found in the posterior contact of bruxism patients before and after stabilization splint treatment. However, differences in posterior contact were observed between bruxists and normal individuals prior to treatment, and this difference disappeared following treatment.
CONCLUSION
The results of this study showed the use of a stabilization splint may not have an effect on occlusion. However, the area of posterior occlusal contact among bruxists was found to be greater than that of normal individuals. According to this study, the clinical use of splints may be harmless.
Bruxism is a disorder characterized by grinding or clenching of the teeth.1 The Glossary of Prosthodontic Terms define bruxism as parafunctional grinding of teeth or an oral habit consisting of involuntary, rhythmic, or spasmodic nonfunctional gnashing, grinding, or clenching of teeth with movement of the mandible other than chewing that may lead to occlusal trauma.2
The etiology of bruxism is not well known, but it is understood to be multifactorial in nature.3 Bruxism and teeth grinding during sleep have been linked to additional factors such as tooth interference in dental occlusion, psychosocial factors such as anxiety or stress, and pathophysiological factors such as disease, trauma, genetics, smoking, alcohol, caffeine, illicit drugs and medications.3-5 Two different types of occlusal management strategies have been used to treat bruxism: occlusal interventions and occlusal appliances.6 Whereas occlusal appliances are commonly used to prevent tooth wear caused by bruxism and/or heavy loading and are not harmful to patients, occlusal interventions such as equilibration, rehabilitation and orthodontic alignment are not supported by the literature.7
Occlusal appliances are usually constructed of hard acrylic resin and worn in the upper jaw.8 Despite their widespread use9, the efficacy of and indications for occlusal appliances are still controversial.6,7,10,11 The effects of a stabilization splint on occlusion have not been reported in the literature. Therefore, this study used a computer-aided occlusal analysis system to analyze the possible side-effects of stabilization splints on occlusion.
Subjects were selected from patients applying to the Department of Prosthodontics at the Erciyes University Faculty of Dentistry after the completion of a diagnostic screening for bruxism. Groups were comprised of 20 individuals with bruxism and 20 healthy volunteers as control.
Inclusion criteria for the bruxism group were as follows12: 1) knowledge or awareness of bruxing (clenching and grinding of teeth during sleep or while awake); 2) masticatory muscle stiffness upon waking; 3) attestation by the subject's sleep partner to grinding noises; 4) presence of mucosal, buccal and/or lateral tongue ridging. Exclusion criteria for both the bruxism and control groups were as follows: 1) signs or symptoms of disk displacement, arthritis or arthrosis of the temporomandibular joint (TMJ); 2) diagnosis of a systemic disease that could affect the masticatory system (e.g. osteoarthritis); 3) a history of trauma in TMJ region; 4) orthodontic treatment history; 5) missing teeth (third molars are not evaluated).
The healthy individuals within the control group did not undergo splint treatment, but were selected based on similarities of age and social status with the patient group in order to facilitate the comparison of disclusion, occlusion and contact distribution values between normal individuals and bruxists.
In total, 40 individuals participated in the study (30 female: mean age: 27.5 ± 3.5 years and 10 male: mean age: 24.6 ± 4.2 years). A written informed consent was signed by all participants, and the protocol was approved by the Faculty Research Ethical Committee (2009.2.1)
All routine clinical examinations and T-scan measurements were performed by the same dentist. Bruxism was treated using a maxillary stabilization splint. They were produced by mounting maxillary casts on a semi-adjustable articulator using a face-bow transfer. Maxillary and mandibular casts were articulated in their intercuspal position. The vertical dimension of the articulator were increased 5 mm by using incisal pin. Splints were fabricated from self-curing clear acrylic, with a cuspid guide to create a rise in protrusive and lateral movements. Splints were adjusted with the participants in the horizontal position in order to provide habitual closure and stable occlusion in the retruded contact position (RCP).13 Participants were asked to use the splint continuously, even while asleep. No occlusal adjustment, prosthodontic treatment, or other treatment that might alter tooth occlusal surfaces was performed. Three months after the initiation of splint treatment, participants were clinically re-examined by the same dentist using the T-scan III occlusal analysis system to evaluate occlusal changes.
Occlusal contact data was measured using T-scan III for Windows (on loan from Tekscan Inc., Boston, MA, USA). T-scan III includes a digital sensor with a thickness of 85 microns consisting of 2,500 pressure-sensitive cells that incorporates a double layer of Mylar, a polyester film with pressure-variable electrical conductivity that allows it to register relative force and distribution of tooth contacts over a pixel size of 1.6 mm2 as well as the initiation and length of contact to within 10 milisecond. For each subject, a new sensor was fitted to a rigid, autoclavable, fork-shaped plastic holder and placed in mouth in contact with the central maxillary incisors and away from the lateral sectors. The same sensor was used for all recordings of a given patient. The patient was instructed to bite down sensor stably, and the resulting drop in electrical resistance was visualized on a computer monitor. The image is adapted by the T-scan III system software, which is capable of recognizing individual dental patterns and missing teeth according to individual tooth size entered into the system.
In order to compensate for individual variations in bite force, the T-scan sensor was recalibrated between patients prior to measurement. For each patient, the same sensitivity value was maintained across all recordings. An initial reading was taken prior to splinting, and another reading was performed 3 months after the insertion of the splint in order to evaluate occlusal changes following splint therapy and to compare the results with those of healthy controls.
The following occlusal parameters were evaluated: 1) occlusion time, defined as the time from the first contact of teeth to maximal intercuspation; 2) disclusion time, defined as the time from maximal intercuspation to the last contact of teeth; 3) left-right occlusal contact area distribution ratios and 4) anterior-posterior occlusal contact area distribution ratios.
Statistical analysis was conducted using SigmaStat (version 3.5, Systat software Inc., San Jose, CA, USA). Normality of distribution of variables was examined using the Kolmogorov-Smirnov test. Due to the abnormal distribution, Wilcoxon tests were used to compare pre- and posttreatment values within groups, and Mann-Whitney U tests were used to compare values between groups, with a difference of P<.05 considered statistically significant.
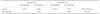
No statistically significant differences were found in occlusion time or disclusion time. Table 1 shows the median and 25%-75% values for each group, and Table 2 shows the results of Mann-Whitney U and Wilcoxon tests comparing inter- and intra group data.
No statistical differences were found between right-left and anterior-posterior contacts. Therefore, analysis was conducted using data for left-side and posterior contact (Fig. 1). As Table 3 shows, no significant differences were observed in left-side contact distribution values pre- and post-treatment or between treatment and control groups (Pre-treatment: 55.2%; Post-treatment: 53.7%; Control: 48.9%, P>.05). Similarly, no significant differences were observed between pre- and post-treatment posterior contact distribution values (Pre-treatment: 94.7%; Post-treatment: 92.8%; P=.164). Interestingly, however, although no significant difference was observed between the post-treatment and control posterior contact distribution values (Post-treatment 92.8%; Control: 79.8%; P=.251), a significant difference was identified between the pre-treatment and control posterior contact distribution values (Pre-treatment: 94.7%; Control: 79.8%; P=.010).
This study examined the effects of splint stabilization treatment on the occlusal contacts of bruxism patients. Occlusal contact is traditionally assessed with articulating paper or other thin strips whose pull-out force at intercuspation helps to reveal initial contacts. Dark, wide marks are understood to be sites of high pressure, whereas lighter marks are associated with sites subjected to lesser loads, and the presence of numerous, similar markings is suggestive of equal, evenly distributed loads.14 However, as some authors have noted, the marks produced by articulating paper may be difficult to reproduce and lend themselves to subjective interpretation, and because they can be affected by patient bite quality, occlusal morphology and salivary impregnation of dental surfaces, which can diffuse the articulating paper ink, they can result in false positives.15 In a recent in vitro study designed to investigate marking surface as the only variable, articulating paper was placed between epoxy resin models of dental arches that were then mounted on an articulator and subjected to compression loads ranging from 25-450 Newtons applied by a uniaxial pneumatic simulator. The results showed that despite a general increase in the marking surface with an increase in applied load, there was only a one-in-five chance that a pair of similar markings would describe the same load.16 Moreover, because articulating paper is unable to register occlusal contact force or time sequencing, it is an insufficient indicator of occlusal contact simultaneity.15,16
In contrast, the T-scan III system uses the center of force position or the quality of the sensor-loading graph and displays (Fig. 2) contacts instantaneously as the patient bites on the sensor, registering multiple consecutive opening/closing cycles.14 Not only does T-Scan measure the intensity and timing of every contact, it translates this information into easily interpreted graphics. Introduced in the United States nearly 30 years ago, the system was revised following doubts with regard to its reliability in occlusal analysis, and improvements were duly noted in a number of studies.14,17-20 Recent publications have reported T-scan III to show good reproducibility of surface measurements and registration of relative forces14,17,18, and Koos et al.17 has shown that readings are unaffected by changing the sensor or repeating measurements. Not only has T-scan been found to provide reliable results in the identification of occlusal contact distribution17,21,22, a study comparing the sensitivity of various occlusal indicators found T-scan to be the only indicator unaffected by saliva.23 Moreover, a 2002 study of the T-Scan II system found that the system provided adequate repeatability in examining the occlusal contacts of complete prosthesis users as well as dentate subjects.24
To date, however, there has been no studies examining the effects of the operator on the values obtained from the T-scan system; therefore, this study was conducted with a single operator and a control group in order to establish normal values.
The name of the most common occlusal appliance, the stabilization splint, suggests that its use in treatment can bring about improvements in occlusion25, however, other possible mechanisms may be involved. Recently, debate has centered around the use of the so-called nociceptive trigeminal inhibition (NTI) splint, a mini-anterior appliance that covers only a few maxillary anterior teeth. Systematic reviews have found such splints to be effective in treating some TMD patients, but have also raised the possibility of adverse effects from its use.26-28
There are very few studies examining possible occlusal changes related to splint therapy. Fujii et al.12 used articulating paper to examine the change in occlusal contacts preand post-splint treatment in bruxism patients with and without myofascial pain. However, the results may be debatable, given the unreliability of articulating paper noted above.
Kerstein and Wright29 was the first to propose that some TMD patients, including bruxists, could be treated by reducing their disclusion time. Their study showed how muscle contraction during excursive function increased with a lengthy disclusion time (>1.39 seconds) and decreased to near rest-state values with a short disclusion time (<0.5 seconds). They went on to describe how disclusion time could be reduced through a technique for occlusal adjustment that they referred to as "immediate complete anterior guidance development", or ICAGD.30 Given that treatment in the present study was conducted using stabilization splints rather than occlusal adjustment, it is not surprising that no differences were found between the post-treatment disclusion times of bruxists and healthy individuals.
In our study, the mean disclusion time for all subjects was less than 1.39 seconds, and no link was found between disclusion time and bruxism. The similarities in occlusion time between bruxists and healthy individuals found in our study differs from Kerstein and Wright's finding that disclusion time increases in patients with myofascial pain dysfunction.19,30,31 The different findings could be related to slight differences in the inclusion criteria between the studies.
The present study found that use of a stabilization splint may not cause changes in occlusion. It also found that bruxism patients tends to have larger areas of posterior contact than healthy individuals. If this finding could be confirmed through future studies with larger patient cohorts, a new parameter could be established for bruxism diagnosis.
Figures and Tables
References
1. Attanasio R. An overview of bruxism and its management. Dent Clin North Am. 1997; 41:229–241.
2. The glossary of prosthodontic terms. J Prosthet Dent. 2005; 94:10–92.
3. Bader G, Lavigne G. Sleep bruxism; an overview of an oromandibular sleep movement disorder. Sleep Med Rev. 2000; 4:27–43.
4. Lobbezoo F, van der Zaag J, Naeije M. Bruxism: its multiple causes and its effects on dental implants - an updated review. J Oral Rehabil. 2006; 33:293–300.
5. Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008; 35:476–494.
6. Lobbezoo F, van der Zaag J, van Selms MK, Hamburger HL, Naeije M. Principles for the management of bruxism. J Oral Rehabil. 2008; 35:509–523.
7. Johansson A, Omar R, Carlsson GE. Bruxism and prosthetic treatment: a critical review. J Prosthodont Res. 2011; 55:127–136.
8. Nassif NJ, al-Ghamdi KS. Managing bruxism and temporomandibular disorders using a centric relation occlusal device. Compend Contin Educ Dent. 1999; 20:1071–1074. 10761078
9. Forssell H, Kalso E, Koskela P, Vehmanen R, Puukka P, Alanen P. Occlusal treatments in temporomandibular disorders: a qualitative systematic review of randomized controlled trials. Pain. 1999; 83:549–560.
10. Dao TT, Lavigne GJ. Oral splints: the crutches for temporomandibular disorders and bruxism? Crit Rev Oral Biol Med. 1998; 9:345–361.
11. Magdaleno F, Ginestal E. Side effects of stabilization occlusal splints: a report of three cases and literature review. Cranio. 2010; 28:128–135.
12. Fujii T, Torisu T, Nakamura S. A change of occlusal conditions after splint therapy for bruxers with and without pain in the masticatory muscles. Cranio. 2005; 23:113–118.
13. Fujii T. Occlusal conditions just after the relief of temporomandibular joint clicking. Cranio. 1999; 17:143–148.
14. Cohen-Levy J, Cohen N. Computerized analysis of occlusal contacts after lingual orthodontic treatment in adults. Int Orthod. 2011; 9:410–431.
15. Kerstein RB. Articulating paper mark misconceptions and computerized occlusal analysis technology. Dent Implantol Update. 2008; 19:41–46.
16. Carey JP, Craig M, Kerstein RB, Radke J. Determining a relationship between applied occlusal load and articulating paper mark area. Open Dent J. 2007; 1:1–7.
17. Koos B, Godt A, Schille C, Göz G. Precision of an instrumentation-based method of analyzing occlusion and its resulting distribution of forces in the dental arch. J Orofac Orthop. 2010; 71:403–410.
18. Throckmorton GS, Rasmussen J, Caloss R. Calibration of T-Scan sensors for recording bite forces in denture patients. J Oral Rehabil. 2009; 36:636–643.
19. Kerstein RB, Lowe M, Harty M, Radke J. A force reproduction analysis of two recording sensors of a computerized occlusal analysis system. Cranio. 2006; 24:15–24.
20. Hützen D, Rebau M, Kordass B. Clinical reproducibility of GEDAS - Greifswald Digital Analyzing System for displaying occlusal contact patterns. Int J Comput Dent. 2006; 9:137–142.
21. Garrido García VC, García Cartagena A, González Sequeros O. Evaluation of occlusal contacts in maximum intercuspation using the T-Scan system. J Oral Rehabil. 1997; 24:899–903.
22. González Sequeros O, Garrido García VC, García Cartagena A. Study of occlusal contact variability within individuals in a position of maximum intercuspation using the T-SCAN system. J Oral Rehabil. 1997; 24:287–290.
23. Saraçoğlu A, Ozpinar B. In vivo and in vitro evaluation of occlusal indicator sensitivity. J Prosthet Dent. 2002; 88:522–526.
24. Kenji O, Shigezo H, Iwao H. A clinical application of the T-Scan II system-usefulness for evaluating occlusal contacts of complete denture wearers. Kokubyo Gakkai Zasshi. 2002; 69:277–284.
25. Carlsson GE. Some dogmas related to prosthodontics, temporomandibular disorders and occlusion. Acta Odontol Scand. 2010; 68:313–322.
26. Stapelmann H, Türp JC. The NTI-tss device for the therapy of bruxism, temporomandibular disorders, and headache -where do we stand? A qualitative systematic review of the literature. BMC Oral Health. 2008; 8:22.
27. Klasser GD, Greene CS. Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:212–223.
28. Jokstad A. The NTI-tss device may be used successfully in the management of bruxism and TMD. Evid Based Dent. 2009; 10:23.
29. Kerstein RB, Wright NR. Electromyographic and computer analyses of patients suffering from chronic myofascial paindysfunction syndrome: before and after treatment with immediate complete anterior guidance development. J Prosthet Dent. 1991; 66:677–686.
30. Kerstein RB. Disocclusion time-reduction therapy with immediate complete anterior guidance development to treat chronic myofascial pain-dysfunction syndrome. Quintessence Int. 1992; 23:735–747.
31. Kerstein RB. Reducing chronic masseter and temporalis muscular hyperactivity with computer-guided occlusal adjustments. Compend Contin Educ Dent. 2010; 31:530–534. 536538




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download