Abstract
Background
The majority of chronic urticaria cases are chronic idiopathic urticaria (CIU) with no specific identifiable etiology. The role of autoantibodies in such cases remains controversial.
Methods
This study was performed on 30 patients with CIU and 30 individuals without any systemic or dermatologic disease. After the volar parts of right and left forearms were cleansed, 0.05 ml serum physiologic and 0.05 ml autologous serum were injected intradermally on the right forearm 5 cm apart from each other, resulting in the formation of small papules; meanwhile, 0.05 ml histamine alone was injected to the left forearm. The test results were evaluated after 30 minutes as positive in positive cases.
Results
The autologous serum test produced significant and non-significant results in patients with CIU and controls, respectively. The positivity rates of the autologous serum test in the CIU and control groups were 53.3% and 26.6%, respectively. There was no relationship between autologous serum test positivity and sex in either group. In male patients with CIU, positive results ranged widely with age, while in female patients, positive results were mainly observed at younger ages with a narrow age range.
Urticaria is a heterogeneous disease group that involves erythematous edematous papules or swelling. Urticaria is classified according to the duration and clinical features of the disease. Chronic urticaria is defined as when swelling continues for longer than 6 weeks. The majority of chronic urticaria cases with no specific etiology are identified after laboratory analysis; these cases constitute a group termed chronic idiopathic urticaria (CIU). Patients with CIU have autoantibodies with high affinity against immunoglobulin E (IgE) receptors (FcεRIα) and less frequently anti-IgE autoantibodies, which are capable of activating mast cell and basophil degranulation. These patients are classified as having autoimmune chronic urticaria1,2,3,4.
Clinical and histological findings remain insufficient to confirm if the development of CIU is linked to autoantibodies1. The autologous serum test is the simplest and best in vivo clinical test for measuring the activity of histamine release by basophils; it is the most commonly used diagnostic test for measuring autoantibodies5. Autoreactivity is achieved by the intradermal injection of autologous serum, through which, factors can indirectly affect the release of mediators from cutaneous mast cells and other cells or directly affecting the skin microvasculature, resulting in pruritic swelling and erythema6.
A positive autologous serum test result indicates the presence of functional autoantibodies or histamine-releasing factors in serum7. The percentage of positive autologous serum test results in adults with CIU when measured using different positivity criteria ranges between 4.1% and 76.5%6. Patients without CIU and healthy individuals generally have negative autologous serum test results1,2,3.
The general consensus is that there is no sensitivity for positive autologous serum test results in patients without CIU and healthy individuals6. In the literature, the percentage of healthy controls with positive autologous serum test results ranges between 0% and 45%4. In another study in which patients with CIU were compared to healthy controls, the sensitivity and specificity of the autologous serum test were 55% and 31%, respectively8. These studies indicate that a positive autologous serum test result is indicative of the presence of autoimmunity rather than directly indicative of autoimmune urticaria9. However, additional investigations are required to determine the sensitivity and specificity of the autologous serum test as an indicator for the presence of autoantibodies10.
Therefore, this study determined the usefulness and the positivity percentages of the autologous serum test in the diagnosis of CIU in 30 patients with CIU and 30 healthy individuals as controls.
This clinical study involved 30 patients with CIU and 30 healthy controls without any underlying systemic or dermatologic disease who were admitted to the Dermatology Department Clinics at Cerrahpasa Medical Faculty, Istanbul University between 2008 and 2011. All participants provided written informed consent using a form from the Ethics committee of Cerrahpasa Medical Faculty, Istanbul University.
Patients younger than 15 and older than 70 years were excluded. Each patient underwent a detailed medical history taking and physical examination. Full laboratory tests including complete blood count, routine biochemistry, erythrocyte sedimentation rate, C-reactive protein, hepatitis markers, antinuclear antibody, thyroid functions tests, anti-thyroid antibodies, C3, C4, urinalysis, stool test for parasites, and Helicobacter pylori antigens in stool were performed in all patients. Patients without any underlying etiologic factor for urticaria were included.
In addition, 30 healthy individuals without a history of urticaria attack or any known autoimmune or dermatologic diseases were included in the healthy control group. All subjects were provided detailed information about the autologous serum test. Statistical analyses were performed by using the χ2 test. Statistical analysis was conducted by using SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) and SAS 9.1 ver. (New York, NY, USA).
Five milliliters venous blood was taken from all subjects by using sterile 27-gauge 10-ml syringes. The blood samples were placed in glass tubes without anticoagulants. Venous blood was stored at room temperature for 30 minutes and subsequently centrifuged for 10 minutes at 500×g. Meanwhile, 0.05 ml 0.9% sterile serum physiologic solution and 0.05 ml histamine were used as negative and positive controls for the skin test, respectively.
The test was applied to patients without active urticarial lesions and those who were known not to develop urticarial plaques within the last 24 hours. In both groups, the injections were made to the volar surface of the right and left forearms. After the areas were cleansed, the injections of 0.05 ml physiologic and autologous serum were made 5 cm apart on the right forearm, and a papule was created by an intradermal injection of 0.05 ml histamine on the left forearm.
To prevent interference between the erythemas and swellings caused by the autologous serum and histamine, they were injected to different arms. If a papule was not observed after the injection, the injection was considered to have been administered too deep and was repeated 2 days later.
The results were evaluated after 30 minutes. If the swelling resulting from the autologous serum exceeded that from serum physiologic injection by 1.5 mm, the swelling was defined as positive. The swelling diameter was measured as the mean between the widest diameter and perpendicular diameter. All readings were performed by the same investigator. Erythema was evaluated according to the criteria of Sabroe and Greaves1 as follows: degree 0, redness that is light pink or skin colored similar to the redness caused by physiologic serum; degree 1, formation of pink swelling by the autologous serum, while the physiologic serum injection site remains normal; degree 2, the redness caused by the autologous serum and histamine are the same, while the physiologic serum injection site has the same skin color; positive test reaction, the erythema caused by the autologous serum is evaluated as degree 2 and the diameter of the swelling is at least 1.5 mm greater than the swelling caused by physiologic serum.
If there were erythema without swelling, the test result was considered negative. A positive test result was accepted as positive after 30 minutes, while the test was repeated after another 30 minutes in negative cases. If there was no reaction at all after 60 minutes, the test was evaluated as negative. If only erythema developed, the test result was considered negative. If degree 2 erythema developed along with swelling compatible with positive criteria, the results were considered positive.
A total of 60 subjects, including 30 with CIU and 30 healthy individuals, were enrolled in this study. There were 19 men (30%) and 41 women (70%).
In the CIU group, 16 patients (53%) exhibited swelling at least 1.5 mm larger than that caused by the negative control as well as degree 2 erythema; thus, their results were evaluated as positive. Meanwhile, the other 14 patients (47%) with CIU exhibited no positive swelling or erythema after 30 minutes; in these patients, the test was repeated at 60 minutes; again there was no swelling detected by that time. Therefore, according to the positivity criteria, 16 and 14 CIU patients had positive and negative autologous serum test results, respectively. The 16 patients with positive results included 11 women and 5 men; 7 of them were younger than 35 years, and 9 were older than 35 years.
Meanwhile, in the control group, 8 subjects (27%) exhibited swelling with a diameter that exceeded the diameter of the swelling caused by the negative control by at least 1.5 mm with grade 2 erythema. The other 22 controls exhibited neither swelling nor erythema. Therefore, 8 (27%) and 22 (73%) controls had positive and negative autologous serum test results, respectively.
In all subjects who exhibited no swelling at 30 minutes, swelling failed to form during the retest at 60 minutes. The 8 controls that had positive results included 4 women and men each; 5 were younger than 35 years of age and 3 were older than 35 years.
In the CIU group, 16 and 14 patients had positive and negative autologous serum test results, respectively. Thus, the positivity rate of the autologous serum test in CIU patients was 53.3%, which was significant. The positive and negative predictive value of the autologous serum test in CIU patients was 91.6%. Meanwhile, 8 and 22 healthy controls had positive and negative autologous serum test results, respectively. Thus, the sensitivity and specificity of the autologous serum test in CIU patients were 66.6% and 61.1%, respectively. Accordingly, the autologous serum test applicability rate was determined to be 63.3%, which was significant.
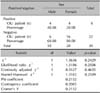
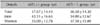
There were 11 female and 5 male CIU patients with positive autologous serum test results. Meanwhile, 30% and 70% of CIU group constituted men and women, respectively. Fig. 1 and Table 1 show the demographic characteristics of the CIU patients and healthy controls with positive autologous serum test results. The χ2 test was used to determine whether the positivity rate of autologous serum test results in CIU patients was associated with sex. However, the results showed no association (Table 2, 3).
In the healthy control group, among those with positive autologous serum test results, 4 were men and 4 were women. Among all healthy controls, 33% and 67% were men and women, respectively. The χ2 test was also used to determine if autologous serum test positivity was associated with sex. However, the results showed no association between the sex and autologous serum test positively in healthy controls.
Among CIU patients with positive autologous serum test results, 7 and 9 were younger and older than 35 years of age, respectively. The mean age of positive patients was 37.55 years. While male CIU patients with positive autologous serum test results had a wide age range, positive female patients were younger and had a narrow age range.
Among healthy controls with positive autologous serum test results, 5 and 3 subjects were younger and older than 35 years, respectively. The mean age of controls with positive autologous serum test results was 37.25 years. Male healthy controls with positive autologous serum test results had a wide age range, whereas positive female controls were younger and had a narrow age range.
Urticaria comprises a wide disease spectrum11. It is classified into 3 basic groups according to its clinical features: spontaneous, physical, and special types. Approximately one-third of spontaneous urticaria cases are chronic urticaria2.
Urticaria has many etiologic. Despite this, no cause can be found in 80%~90% of cases. In such cases, the disease is classified as CIU10,12. From 25%~60% of patients with CIU have circulating functional antibodies with high affinity for IgE receptors (FcεRIα) or antibodies against IgE itself; these antibodies cause positive autologous serum test results3. There is currently strong evidence of an autoimmune basis in about 50% of patients diagnosed with CIU13.
For CIU to be considered an autoimmune entity, the serum sampled from afflicted individuals must induce a reaction in the autologous serum test transferred passively into the skin of healthy individuals. Disease regression due to antibody suppression as well as the relationship between disease severity and functional antibodies are accepted as the basic underlying mechanisms1.
Clinical and histological findings in CIU are insufficient to confirm if CIU develops in relation to the presence of autoantibodies. The antibodies in patients with CIU can be detected by the following 4 methods: autologous serum test, histamine release from basophils, western blotting, and enzyme-linked immunosorbent assay. The autologous serum test is a simple and inexpensive method compared to the others. Although its clinical value is not very well defined yet, it is still used to determine the presence of autoantibodies1,2,3,4,14.
When using different positivity criteria for evaluating the autologous serum test in adult CIU patients, the frequency of positive autologous serum test results ranges between 4.1% and 76.5%. This wide range can be attributed to many factors such as patient selection, disease severity, methodology, sensitivity evaluation, and the fact that the prevalence rate of autoimmune urticaria is unknown in the population being tested6.
This study excluded test results in which red swelling formed in the negative control area or no swelling failed to form at the histamine injection site.
The best results for maximizing the positive predictive value can be obtained when the test is read at 30 minutes compared to readings at 15 and 60 minutes6. Therefore, we read the results at 30 minutes. Nevertheless, in cases showing negative results at 30 minutes, we reevaluated the test at 60 minutes. No positive autologous serum test results were observed at 60 minutes in any subjects with negative autologous serum test results at 30 minutes.
There is no relationship between the sensitivity of the autologous serum test and age, personal or familial history, or with age of disease onset. Nevertheless, another study reports the prevalence of positive autologous serum test results is noticeably higher in women (76%) than men (35%)6. In addition, Taskapan et al.7 report that the autologous serum test positivity rate is higher in women. In contrast, another study shows no significant associations with epidemiologic characteristics except for disease duration, frequency of attacks, diurnal variation, and angioedema15. The positivity rate in all the women in the present study was 37%. Thus, the finding that men had a higher autologous serum test positivity rate in the present study is discordant with previous studies. Nevertheless, the present study is concordant with other studies in that there was no relationship between sex and autologous serum test positivity.
In previous studies, positive autologous serum test results occurred mostly between 18 and 30 years of age7. In the present study, the mean age of patients was 37.67 years, which is comparable to the previous studies. The mean ages of men and women with positive autologous serum test results were 42.11 and 35 years, respectively. Therefore, it can be concluded that men exhibit positive autologous serum test results at later ages distributed over a wide range compared to women. Positive autologous serum test results were very rare in elderly women.
Guttman-Yassky et al.8 report that IgG antibodies against IgE and FcεRI alone are insufficient for the development of skin sensitivity in the autologous serum test; these antibodies are also reported in patients with non-idiopathic urticaria and some other diseases as well as healthy populations.
In the literature, positive autologous serum test results are reported to occur in 0%~45% of healthy subjects. Guttman-Yassky et al.8 report autologous serum test positivity rates as 45.0% and 40.5% of healthy controls, respectively. Meanwhile, Taskapan et al.7 report the highest rate of autologous serum test positivity in healthy subjects (55.55%). Moreover, Kocatürk et al.16 studied 70 adults with chronic spontaneous urticaria and 62 controls who underwent the autologous serum test and autologous plasma test repeated 2 days after the first visit; the autologous serum test was positive in 44 patients (63%) and 9 controls (14.5%). Metz et al.17 report results from 3 centers in Spain, England, and Germany; they reports that autologous serum test was positive in 37.5% of chronic urticaria patients. In the present study, the autologous serum test positivity rates of CIU and healthy controls were 53.3% and 26.6%, respectively. Therefore, we conclude that the positivity rate of the autologous serum test in healthy population is non-significant.
Positive autologous serum test results are significant in CIU patients and non-significant in healthy controls. Therefore, autologous serum test is the simplest in vivo test for measuring histamine release from basophils. Regardless, existing clinical and histological findings do not fully clarify if the development of CIU is associated with autoantibodies. Hence, the autologous serum test is an important test that can be used to demonstrate the presence of autoantibodies.
The autologous serum test should be mandatory for the diagnosis of CIU. However, as autologous serum test produces coincidental positive results in healthy controls, the distinct positivity of the test must be clarified. Because of its importance, the autologous serum test is helpful for the selection of immunotherapy in patients resistant to classical therapy as well as for making a clinical diagnosis and approaching therapy.
Figures and Tables
Table 3
Relationship between sex and positive AST results in healthy controls
Twenty-five percent of the cells have expected counts less than 5. χ2 may not be a valid test. The cut-off for rejected H0 was 0.2429. This analysis showed no relationship between AST positivity and sex. AST: autologous serum test, df: degrees of freedom, H0: no relationship, H1: relationship present.
References
1. Sabroe RA, Greaves MW. Chronic idiopathic urticaria with functional autoantibodies: 12 years on. Br J Dermatol. 2006; 154:813–819.
4. Mete N, Gülbahar O, Sin A, Kokuludağ A, Sebik F. Kronik idiopatik ürtikerde otolog serum testi. Ege Tıp Dergisi. 2003; 42:25–29.
5. George M, Balachandran C, Prabhu S. Chronic idiopathic urticaria: comparison of clinical features with positive autologous serum skin test. Indian J Dermatol Venereol Leprol. 2008; 74:105–108.

6. Konstantinou GN, Asero R, Maurer M, Sabroe RA, Schmid-Grendelmeier P, Grattan CE. EAACI/GA(2)LEN task force consensus report: the autologous serum skin test in urticaria. Allergy. 2009; 64:1256–1268.

7. Taskapan O, Kutlu A, Karabudak O. Evaluation of autologous serum skin test results in patients with chronic idiopathic urticaria, allergic/non-allergic asthma or rhinitis and healthy people. Clin Exp Dermatol. 2008; 33:754–758.

8. Guttman-Yassky E, Bergman R, Maor C, Mamorsky M, Pollack S, Shahar E. The autologous serum skin test in a cohort of chronic idiopathic urticaria patients compared to respiratory allergy patients and healthy individuals. J Eur Acad Dermatol Venereol. 2007; 21:35–39.

9. Philpott H, Kette F, Hissaria P, Gillis D, Smith W. Chronic urticaria: the autoimmune paradigm. Intern Med J. 2008; 38:852–857.

11. Zuberbier T, Asero R, Bindslev-Jensen C, Walter Canonica G, Church MK, Giménez-Arnau A, et al. Dermatology Section of the European Academy of Allergology and Clinical Immunology. Global Allergy and Asthma European Network. European Dermatology Forum. World Allergy Organization. EAACI/GA(2)LEN/EDF/WAO guideline: definition, classification and diagnosis of urticaria. Allergy. 2009; 64:1417–1426.

13. Grattan CEH, Black AK. Urticaria and mastocytosis. In : Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's textbook of dermatology. 7th ed. Massachusetts: Blackwell Publishing Inc.;2004. p. 47.1–47.37.
14. Al-Hamamy HR, Hameed AF, Abdulhadi AS. Autologous serum skin test as a diagnostic aid in chronic idiopathic urticaria. ISRN Dermatol. 2013; 2013:291524.

15. Krupashankar DS, Shashikala K, Madala R. Clinical and investigative assessment of patients with positive versus negative autologous serum skin test: a study of 80 South Indian patients. Indian J Dermatol. 2012; 57:434–438.

16. Kocatürk E, Kavala M, Kural E, Sarıgul S, Zındancı I. Autologous serum skin test vs autologous plasma skin test in patients with chronic urticaria: evaluation of reproducibility, sensitivity and specificity and relationship with disease activity, quality of life and anti-thyroid antibodies. Eur J Dermatol. 2011; 21:339–343.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download