Abstract
Background
Atopic dermatitis, a chronic recurrent disease, is frequently encountered in clinical practice. In the last 30 years, the prevalence of atopic dermatitis has rapidly increased due to industrialization. Therefore, there have been attempts in recent years to find new ways of treating and preventing atopic dermatitis.
Objective
In this double-blind, randomized, placebo-controlled study, a combination of Bifidobacterium bifidum, Lactobacillus acidophilus, Lactobacillus casei, and Lactobacillus salivarius strains were evaluated in the treatment of atopic dermatitis in pediatric patients.
Methods
Forty pediatric patients (23 males and 17 females) aged 1~13 years were enrolled. One eligible individual who was approached declined to participate. The probiotic group was administered a probiotic complex containing B. bifidum, L. acidophilus, L. casei, and L. salivarius for 8 weeks. The placebo group, on the other hand, was administered skim milk powder and dextrose. All of the parameters including serum cytokines, eosinophil cationic protein), SCORing Atopic Dermatitis (SCORAD) index, and total serum immunoglobulin E (IgE) were measured in both the probiotic group and the placebo group at the end of 8 weeks.
Results
Probiotic intervention in pediatric atopic dermatitis patients effectively reduced the SCORAD index and serum cytokines interleukin (IL)-5, IL-6, interferon (IFN)-γ, and total serum IgE levels, but did not reduce levels of serum cytokines IL-2, IL-4, IL-10, ECP, or tumor necrosis factor-α (TNF-α) compared to the placebo group.
Atopic dermatitis (AD) is a common infant or early childhood disease for which genetic factors may create a disposition and is triggered by a variety of antigens. AD is characterized by chronic or relapsing inflammatory dermatitis1. Atopy is described as "a personal or familial tendency to produce IgE antibodies in response to low doses of allergens, usually proteins, and to develop typical symptoms such as asthma, rhinoconjunctivitis, or AD2." The prevalence of AD has increased in with industrialization3. Thus, new approaches have attracted interest in the treatment of AD.
While probiotic means "for life," allergic diseases (AD, allergic rhinitis, asthma, etc.) have been demonstrated in the treatment of many systemic diseases4. In this study, we have examined the clinical and anti-inflammatory effects of probiotic supplementation in pediatric patients with AD.
Forty pediatric patients (23 males and 17 females) aged 1~13 years participated in the study between October 2007 and April 2008. All children met the diagnostic criteria for AD as defined by Hanifin and Rajka5. The inclusion criteria were: a moderate to severe Scoring Atopic Dermatitis (SCORAD) index score6,7; being 1~13 years of age; absence of any other disease; having used no medication including antihistamines and corticosteroids for fourteen days prior to the study; and absence of gastrointestinal malabsorption.
Patients were referred to a nurse who was involved in the study to receive either probiotics or placebo. The nurse randomized each patient to two different treatment groups using the closed-envelope method. The authors had no role in the treatment decision and were blinded to the treatment groups. In this randomized double-blind, placebo-controlled study, patients were assigned to one of two groups, probiotics (Group 1) or placebo (Group 2). Group 1 (n=20) received two bags containing 2×109 of four types of probiotic bacteria (Bifidobacterium bifidum, Lactobacillus acidophilus, Lactobacillus casei, and Lactobacillus salivarius) made by a commercially available supplementation (proBiotik® pur, Ella Farma, Münster, Germany), while those in Group 2 (n=20) received skim milk powder (Dairy Inc., Enka Milk Joint Stock Company, Turkey) and dextrose (Havana Chemistry, Pharmaceutical Medical Limited Company, Istanbul, Turkey) daily for a total of eight weeks.
Blood samples collected at baseline and ten weeks later were followed by storing plasma frozen at -80℃ until all cytokine analyses were performed. Total immunoglobulin E (IgE) levels were analyzed using total and 3gAllergy™ assays (Immulite 2,000 Immunoassay System, Siemens Healthcare Diagnostics, Siemens Healthcare Diagnostics Inc., Deerfield, IL, USA), following the manufacturer's instructions. Eosinophil cationic protein (ECP) and cytokine levels were determined using enzyme-linked immunosorbent assay (BioSource International, Inc., Camarillo, CA, USA) using a Triturus® System (Grifols International S.A., manufactured by Grifols-Quest Inc.).
The study protocol followed the Declaration of Helsinki and included written consent by the parents or guardians of the participating patients. The study was approved by the Drug Research Ethics Committee and was supported by the Scientific Research Projects.
All analyses were conducted using SPSS 11.5 statistical program (SPSS Inc., Chicago, IL, USA). A ratio test was applied to compare the proportion of patients in groups by age and sex. Pre- and post-treatment differences of serum cytokines, total IgE levels, ECP, and changes in SCORAD indices were compared using a paired t-test. p-values<0.01 were considered statistically significant.
One female patient in the placebo group failed to attend her follow-up visits resulting in withdrawal from the study. Comprising 58.9% of the patients, 23 males (aged 1~12 years, mean [standard deviation, SD] 7.6±3) and 16 females (aged 1~13 years, mean [SD] 9.3±3.2) completed the study.
The SCORAD index changed from 35.4±13.4 to 12.4±7.2 and from 28.1±6.1 to 15.3±5.1 in the probiotic and placebo groups, respectively. The post-treatment decrease in the SCORAD index in the probiotic group was greater than the decrease in the placebo group, a difference that was statistically significant (p=0.0015; Table 1, Fig. 1).
As seen in Fig. 1, there was a decrease in the serum interleukin (IL)-5, IL-6 and interferon (IFN)-γ levels of the probiotic group after treatment. The difference between the post-treatment decreases in cytokines IL-5 (p=0.0012) and IL-6 (p=0.0016) and IFN-γ (p=0.0011) was statistically significant compared to the difference in decreases of these cytokines in the placebo group. The difference between the rates of post-treatment decreases in the serum levels of IL-2 (p=0.023), IL-4 (p=0.67), IL-10 (p=0.013), ECP (p=0.021), and tumor necrosis factor-α (TNF-α; p=0.437) and the rates of post-treatment decrease of these cytokines in the placebo group did not have statistical significance.
The serum total IgE level decreased from 427±500 IU/ml to 281.9±405 IU/ml in the probiotic group. In the placebo group, the serum total IgE increased from 337.3±298 IU/ml to 347.7±271.3 IU/ml. The difference between the post-treatment serum IgE levels of the probiotic group and those of the placebo group was statistically significant (p=0.0035).
There is a growing interest in using probiotic supplements not only by consumers for its health-promoting effects on a daily basis but also by health care professionals for its efficacy as a supplement and therapeutic product to treat a variety of medical conditions8. Probiotics affect allergic conditions on a number of levels. In the intestinal system, they inhibit the epithelial and mucosal adherence of pathogens and prevent their invasion through the epithelium9. Probiotics compete with pathogens for limited loci by their ability to adhere to intestinal epithelium and mucus. They also inhibit the proliferation of pathogens by consuming the nutrients in the intestine. Furthermore, the antibacterial potential of certain probiotic strains involves secretion of hydrogen peroxide, organic acids, and bacteriocins that inhibit the growth of pathogens. Hydrolytic enzymes contribute to the increase of free fatty acids, short chain fatty acids, lactic acid, propionic acid, and butyric acid in the intestinal lumen, thus setting up an appropriate pH. Probiotics alter mucosal immunity considerably. This involves an increase in antibody production and activities of phagocytes and natural killer cells, modulation of the nuclear factor-κB pathway, and induction of T-cell apoptosis10. In addition, probiotics have been shown to modify the structure of potential allergens that cause allergic diseases and alleviate their immunogenicity11.
Our results demonstrated an improved SCORAD index in both groups, but with higher levels in the probiotic group (65%) than in the placebo group (46%). In the probiotic group, a greater decrease of SCORAD index scores was shown after treatment in patients with high SCORAD index scores. However, this difference did not reach a statistically significant level (p=0.0015). SCORAD index of AD patients were evaluated before and after an eight-week intervention using a combination of the probiotics Lactobacillus paracasei Lpc-37, Lactobacillus acidophilus 74-2, and Bifidobacterium animalis subsp. lactis DGCC 420. It decreased by 15.5% in the probiotic group, while the decrease was only 8% in the placebo group12. In nine of thirteen randomized controlled trials studying the effectiveness of probiotics in the treatment or prevention of AD in children, the SCORAD index changed after one- or two-month probiotic administration13. There are other studies on the probiotic intervention indicating favorable results in the SCORAD index of AD patients14-19.
The serum total IgE level decreased from 427±500 IU/ml to 281.9±405 IU/ml in the probiotic group. In the placebo group, the serum total IgE increased from 337.3±298 IU/ml to 347.7±271.3 IU/ml. A significant difference was found between the probiotic and placebo groups regarding total IgE levels (p=0.0035).
Our study showed probiotics to be effective in reducing AD patients' serum IL-5, IL-6, and IFN-γ levels. A double-blind, placebo-controlled study, however, found no clinical or immunological effects of probiotics of the Lactobacillus strain in serum IL-4, IL-5, and IFN-γ levels in infants with AD compared with the placebo group after three months of treatment20. Another double-blind, placebo-controlled study of 230 infants with atopic eczema/dermatitis syndrome showed no difference in clinical signs and serum IgE levels for the Lactobacillus GG-administered group and the placebo group21. Other clinical studies did not report any difference in cytokine levels after treatment with probiotics13,22.
As a result, our study found probiotics effective in reducing AD patients' SCORAD index, serum IL-5, IL-6, IFN-γ, and total serum IgE levels but not effective in reducing serum IL-2, IL-4, IL-10, ECP, and TNF-α levels. The impact of probiotics on SCORAD indices is thought to be reduced by modification of immunogenicity of potential allergens. Probiotics are effective in the pathogenesis of AD through their effects such as restoring the mucosal barrier function in the intestines, degrading food antigens, regulating the intestinal microbial composition and activities, and stimulating the production of secretory IgA23. They also block Th2 allergic response by stimulating Th1 response13,23-26. Probiotics regulate local and systemic immunity and thus alleviate the severity of clinical symptoms.
Figures and Tables
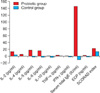 | Fig. 1Changes in the levels of serum cytokines, SCORAD index, and total serum IgE and comparisons before and after probiotic and placebo administration. SCORAD: SCORing Atoptic Dermatitis, IgE: immunoglobulin E, IL-2: interleukin-2, IL-4: interleukin-4, IL-5: interleukin-5, IL-6: interleukin-6, IL-10: interleukin-10, TNF-α: tumor necrosis factor-α, IFN-γ: interferon-γ, ECP: eosinophil cationic protein. |
Table 1
Changes in the levels of serum cytokines, SCORAD index, and total serum IgE levels and comparisons before and after probiotic and placebo administration

SCORAD: SCORing Atoptic Dermatitis, BT: before treatment, SD: standard deviation, AT: after treatment, IL-2: interleukin-2, IL-4: interleukin-4, IL-5: interleukin-5, IL-6: interleukin-6, IL-10: interleukin-10, TNF-α: tumor necrosis factor-α, IFN-γ: interferon-γ, ECP: eosinophil cationic protein, IgE: immunoglobulin E. *Statistical used paired t-test for testing. p values<0.05 were considered statistically significant.
References
1. Kristal L, Klein PA. Atopic dermatitis in infants and children. An update. Pediatr Clin North Am. 2000. 47:877–895.
2. Johansson SG, Hourihane JO, Bousquet J, Bruijnzeel-Koomen C, Dreborg S, Haahtela T, et al. A revised nomenclature for allergy. An EAACI position statement from the EAACI nomenclature task force. Allergy. 2001. 56:813–824.

3. Bengmark S, García de Lorenzo A, Culebras JM. Use of pro-, pre- and synbiotics in the ICU--future options. Nutr Hosp. 2001. 16:239–256.
4. Gill HS, Guarner F. Probiotics and human health: a clinical perspective. Postgrad Med J. 2004. 80:516–526.

5. Cosickic A, Skokic F, Colic-Hadzic B, Jahic M. Clinical characteristics and estimation severity of the atopic dermatitis in children. Med Arh. 2010. 64:178–182.
6. Carr WW. Improvements in skin-testing technique. Allergy Asthma Proc. 2006. 27:100–103.
7. Oranje AP, Glazenburg EJ, Wolkerstorfer A, de Waard-van der Spek FB. Practical issues on interpretation of scoring atopic dermatitis: the SCORAD index, objective SCORAD and the three-item severity score. Br J Dermatol. 2007. 157:645–648.

8. Boyle RJ, Robins-Browne RM, Tang ML. Probiotic use in clinical practice: what are the risks? Am J Clin Nutr. 2006. 83:1256–1264.

9. Servin AL, Coconnier MH. Adhesion of probiotic strains to the intestinal mucosa and interaction with pathogens. Best Pract Res Clin Gastroenterol. 2003. 17:741–754.

10. Morita H, He F, Fuse T, Ouwehand AC, Hashimoto H, Hosoda M, et al. Adhesion of lactic acid bacteria to caco-2 cells and their effect on cytokine secretion. Microbiol Immunol. 2002. 46:293–297.

11. Maassen CB, van Holten-Neelen C, Balk F, den Bak-Glashouwer MJ, Leer RJ, Laman JD, et al. Strain-dependent induction of cytokine profiles in the gut by orally administered Lactobacillus strains. Vaccine. 2000. 18:2613–2623.

12. Roessler A, Friedrich U, Vogelsang H, Bauer A, Kaatz M, Hipler UC, et al. The immune system in healthy adults and patients with atopic dermatitis seems to be affected differently by a probiotic intervention. Clin Exp Allergy. 2008. 38:93–102.

13. Betsi GI, Papadavid E, Falagas ME. Probiotics for the treatment or prevention of atopic dermatitis: a review of the evidence from randomized controlled trials. Am J Clin Dermatol. 2008. 9:93–103.
14. Weston S, Halbert A, Richmond P, Prescott SL. Effects of probiotics on atopic dermatitis: a randomised controlled trial. Arch Dis Child. 2005. 90:892–897.

15. Van Leent EJM, Bos JD. Katsambas AD, Lotti TM, editors. Atopic dermatitis. European handbook of dermatological treatments. 2003. 2nd ed. Berlin: Springer-Verlag;54–62.

16. Isolauri E. Probiotics in the prevention and treatment of allergic disease. Pediatr Allergy Immunol. 2001. 12:56–59.

17. Kalliomäki M, Salminen S, Arvilommi H, Kero P, Koskinen P, Isolauri E. Probiotics in primary prevention of atopic disease: a randomised placebo-controlled trial. Lancet. 2001. 357:1076–1079.

18. Kalliomäki M, Salminen S, Poussa T, Arvilommi H, Isolauri E. Probiotics and prevention of atopic disease: 4-year follow-up of a randomised placebo-controlled trial. Lancet. 2003. 361:1869–1871.

19. Sistek D, Kelly R, Wickens K, Stanley T, Fitzharris P, Crane J. Is the effect of probiotics on atopic dermatitis confined to food sensitized children? Clin Exp Allergy. 2006. 36:629–633.

20. Brouwer ML, Wolt-Plompen SA, Dubois AE, van der Heide S, Jansen DF, Hoijer MA, et al. No effects of probiotics on atopic dermatitis in infancy: a randomized placebo-controlled trial. Clin Exp Allergy. 2006. 36:899–906.

21. Viljanen M, Savilahti E, Haahtela T, Juntunen-Backman K, Korpela R, Poussa T, et al. Probiotics in the treatment of atopic eczema/dermatitis syndrome in infants: a double-blind placebo-controlled trial. Allergy. 2005. 60:494–500.

22. Prescott SL, Dunstan JA, Hale J, Breckler L, Lehmann H, Weston S, et al. Clinical effects of probiotics are associated with increased interferon-gamma responses in very young children with atopic dermatitis. Clin Exp Allergy. 2005. 35:1557–1564.

24. Winkler P, Ghadimi D, Schrezenmeir J, Kraehenbuhl JP. Molecular and cellular basis of microflora-host interactions. J Nutr. 2007. 137:756S–772S.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download