Abstract
Objective
The aim of this study was to determine whether different types of adhesive systems and enamel-protective agents will affect the tensile bond strength of lingual brackets.
Methods
A total of 75 extracted mandibular incisors were randomly divided into 5 groups and lingual brackets were bonded. Group 1 specimens received Transbond XT (3M Unitek, Monrovia, CA, USA), Group 2 required the application of a fluoride-releasing resin (Ortho-coat, Pulpdent, Watertown, MA, USA) with Transbond XT, Group 3 specimens received a chlorhexidine varnish (Cervitec Plus, Ivoclar Vivadent, Schaan, Lichtenstein) with Transbond XT. In Group 4, a light-cured orthodontic adhesive (Aegis Ortho, Bosworth, Skokie, USA) was applied and in Group 5, an antimicrobial self-etching primer (Clearfil Protect Bond, Kuraray, Osaka, Japan) was used.
Results
There were no significant differences in bond strength whether fluoride-releasing resin or chlorhexidine varnish were used or not. Group 5 had significantly higher bond strength and adhesive remnant index (ARI) values than other groups (p < 0.001). The application of enamel-protective products did not have an adverse affect on the bond strength of lingual brackets.
Conclusions
These products might provide benefits both for the patient and the clinician, by supporting the oral hygiene during lingual orthodontic treatment. The higher ARI score may be beneficial for Clearfil Protect Bond but its excessive bond strength should be considered in clinical practice, especially where the enamel is thin.
Esthetic materials have appeared in the market, since the number of adult patients seeking orthodontic treatment has increased in recent years. During the last two decades, the problem of esthetics during orthodontic treatment has been solved by attaching fixed appliances to the lingual surfaces of teeth.1 Despite the esthetic advantages, disadvantages such as patient discomfort have also been mentioned in several studies.1-3 While some studies have focused on tongue irritations, pain, speech and eating problems,1,3 other studies dealt with difficulties with oral hygiene.2,4
Fixed orthodontic appliances induce changes in the oral environment, such as increased retention sites for food particles and dental plaque, a low-pH environment and increased proportions of Streptococcus mutans.5-7 Consequently, the risk of decalcification and dental caries increases in some cases.8,9 Attempts have been made to maintain proper oral hygiene around brackets and bands in orthodontic patients. For this purpose, fluoride releasing and/or antimicrobial agents have been applied in orthodontic patients.9 New materials have recently appeared in the market which includes fluoride-releasing resins,10 chlorhexidine varnishes,11 amorphous calcium phosphate (ACP) containing orthodontic adhesive,12 and anti-microbial agents.13,14 These products claim to prevent demineralization and white spot lesions around orthodontic brackets, and maintain plaque control throughout the treatment.
Although Gorelick et al.15 emphasized that flow of saliva is a major factor in avoiding decalcification of enamel on the lingual surfaces of the mandibular incisors, maintaining oral hygiene is more difficult for patients with lingual brackets than with buccal brackets, since perfect oral hygiene is particularly important in these patients. Also the small tooth surface from the bracket to gingival margin is conducive to the retention of dental plaque. The clinical application of aforementioned agents can be useful, but they must first provide an acceptable level of bond strength. Morphological differences exist between labial and lingual tooth surfaces especially in anterior teeth, as well as the etching surface areas.16 Besides, the base surface area of lingual brackets show differences due to the lingual surface anatomy of incisors.
Therefore, the aim of this study was to evaluate whether different orthodontic adhesives provide satisfactory bond strength for lingual orthodontic brackets in the mandibular anterior region. For this purpose, the effect of a fluoride-releasing resin (Ortho-Coat; Pulpdent Co, Watertown, MA, USA), a chlorhexidine varnish (Cervitec Plus; Ivoclar Vivadent, Schaan, Lichtenstein), a light-cured orthodontic adhesive containing Amorphous Calcium Phosphate (ACP) (Aegis Ortho; Bosworth, Skokie, Ill, USA), and an antimicrobial self-etching primer (Clearfil Protect Bond; Kuraray Medical Inc., Okayama, Japan) were compared with a commonly used orthodontic adhesive, Transbond XT (3M Unitek, Monrovia, CA, USA).
A total of seventy-five caries-free human mandibular incisors, extracted with orthodontic and periodontal indications, were used in this study. The teeth were stored in distilled water with thymol crystals (%1 wt/vol) added to inhibit bacterial growth at room temperature after extraction. The criteria for tooth selection included intact enamel that had not been pretreated with chemical agents and no visible cracks or enamel irregularities.
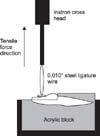
The teeth were cleaned and polished with a fluoride-free pumice slurry and rubber cups for 10 seconds and thoroughly washed and dried with an oil-free air stream. They were examined under a light stereomicroscope at × 10 magnification to ensure the absence of caries and enamel cracks. The sample was randomly divided in five groups of 15 specimens each. All were embedded horizontally in cold-curing acrylic (Orthocryl, Dentaurum, Ispringen, Germany) using metal ring moulds (Fig 1).
Lower incisor metal lingual orthodontic brackets (American Orthodontics, Sheboygan, Wis, USA) were used and placed by the same researcher in order to standardize the pressure. The dimensions of the lingual brackets were derived from the manufacturer and mean base surface area of the brackets were calculated as 9.16 mm2.
Group 1 utilized the conventional bonding with Transbond XT primer (3M Unitek, Monrovia, CA, USA) according to the manufacturer's guidelines. The lingual enamel was etched for 30 seconds with 37% phosphoric acid gel (Gel Etch, 3M Unitek, Monrovia, CA, USA) and washed with water spray for 20 seconds and air-dried with an oil-free air force. Primer was rubbed with pressure onto the enamel surface of each tooth for 5 seconds and dried with air. The brackets were coated with Transbond XT adhesive paste and positioned at the center of the lingual surface. Excess adhesive was removed from the margins of the bracket base with a scaler before polymerization. All brackets were light-cured for a total of 40 seconds (10 seconds each from the mesial, distal, gingival and occlusal margins) with a halogen curing unit (Hilux Ultra Plus, 600 mW/cm2, Benlioğlu Dental, Ankara, Turkey). The light intensity of the halogen curing unit was checked before each testing procedure with a curing radiometer (Demetron Kerr, Danbury, CT, USA). There was no measurable reduction in intensity for any light during the experiment.
In Group 2, the same bonding procedure was performed as in Group 1. After the bonding of the brackets, a fluoride-releasing resin, Orthocoat (Orthocoat, Pulpdent, Watertown, MA, USA) was applied around the bracket-enamel margin and light cured for a total of 40 seconds (10 seconds each from the mesial, distal, gingival and occlusal margins) in accordance with the manufacturer's guidelines.
In Group 3, Cervitec Plus (Ivoclar Vivadent, Schaan, Liechtenstein) which is a varnish that contains a combination of chlorhexidine and thymol, was applied to the bracket-enamel margin after bonding the brackets as in the first group.
The brackets were bonded by following the manufacturer's instructions with Aegis Ortho (Bosworth, Skokie, Ill, USA), a light-cure orthodontic adhesive containing amorphous calcium phosphate (ACP) in Group 4. First, the enamel was etched for 30 seconds with 35% phosphoric acid, washed with water for 20 seconds and air-dried with an oil-free air stream. The primer was rubbed with pressure onto the enamel surface of each tooth for 5 seconds and dried with air. The adhesive paste was applied to the bracket base and the brackets were positioned at the center of the lingual surface. After the removal of excess adhesive, the teeth were light-cured for a total of 40 seconds, 10 seconds each from the mesial, distal, gingival and occlusal margins.
In Group 5, an anti-bacterial self-etching primer, Clearfil Protect Bond (Kuraray Medical, Osaka, Japan) was applied as suggested by the manufacturer. Clearfil Protect Bond was manufactured to provide adequate bond strength for bonding to dentine and prepared enamel surfaces. As brackets were bonded to uncut enamel surfaces, the enamel surface was etched for 10 seconds with 37% phosphoric acid gel prior to bonding. Second, the teeth were washed with water for 20 seconds and air-dried. Third, the Clearfil Protect Bond primer was applied with a brush on the etched enamel surfaces in a thin uniform layer, left for 20 seconds and sprayed with an air stream to evaporate the solvent. Later, the bonding agent was applied and light cured for 10 seconds. Brackets were bonded with Transbond XT adhesive paste, placed on the center of the lingual surfaces and after removal of excess adhesive, they were light cured for 40 seconds.
All specimens were stored in distilled water at room temperature for 24 hours. Tensile debonding test was performed with a Universal testing machine (Instron, Canton, MA, USA). The specimens were stressed in a vertical direction to the bracket base with a crosshead speed of 1 mm/min. The maximum tensile force necessary to debond each bracket was recorded in Newton and then converted into Megapascal (MPa).
The debonded enamel surfaces were examined under a stereomicroscope (Nikon, Osaka, Japan) at 20 × magnification to assess the residual adhesive remaining on the tooth surface by a blinded examiner (CU). A modified adhesive remnant index (ARI) was used to quantify the amount of remaining adhesive on the tooth surface. The following scale was used: 1, all adhesive remaining on the tooth; 2, more than 90% of the adhesive remaining on the tooth; 3, between 10 - 90% of adhesive remaining on the tooth; 4, less than 10% of the adhesive remaining on the tooth; 5, no adhesive remaining on the tooth.
Statistical evaluation was performed, using SPSS for Windows version 11.0 (Chicago, IL, USA). Descriptive statistics including the mean, standard deviation, minimum and maximum values were calculated for each group. The distribution of the variables was evaluated by Kolmogorov-Smirnov test. Since the measurements were not normally distributed and because of the small sample size, nonparametric tests were used. Kruskal-Wallis one-way ANOVA was used to determine differences in bond strength data and ARI values. As the p-values of Kruskal-Wallis tests were less than 0.001, pairwise comparisons were performed using Mann-Whitney U-test adjusted according to Bonferoni at a significance level of p < 0.005.
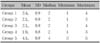
The bond strength values and the statistical comparisons are presented in Table 1. Kruskal-Wallis test revealed significant differences among groups (p < 0.005). Pairwise comparison of the groups with the Mann-Whitney U test showed no significant differences between groups 1, 2 and 3, whereas groups 4 and 5 showed statistically significant differences when compared with each other and with the other groups (p < 0.005). Group 5 had the highest bond strength, whereas group 4 had the lowest bond strength values (Table 1).
The ARI scores are displayed in Table 2. No enamel fractures were detected in any of the specimens. Statistically significant differences were found with the Kruskal-Wallis test (p < 0.001). The Mann-Whitney U test showed that group 5 displayed a significantly greater ARI score when compared to the other groups (p < 0.001).
In the current study the main aim was to determine whether different adhesive systems and enamel protective agents would affect the tensile bond strength of lingual brackets bonded to the enamel of lower incisor teeth. Different from the labial surface, the lingual side of lower anterior teeth have a convex surface topography such as a cingulum, which may exaggerate the results of commonly used shear bond strength tests. For this reason, the tensile bond strength test was preferred in order to eliminate the effect of lingual morphology.
The use of orthodontic fixed appliances creates significant oral hygiene challenges for the patient and the clinician throughout the long treatment periods. The results of studies have suggested using enamel protective methods which reduce the dependence on patient compliance in preventing the development of white spot lesions around brackets and at the gingival margins.17 Proper oral hygiene is more difficult to maintain in patients with lingual brackets, because hygiene control is harder from the lingual than from the buccal side, therefore plaque accumulations, gingivitis and demineralization cannot be detected by the patient.2 The problems in maintaining oral hygiene in lingual orthodontic patients can be handled by using special prophylactic procedures.18
The recently developed light-cured reinforced resin, Ortho Coat claims to prevent decalcification, micro leakage, and discoloration of teeth under orthodontic brackets. It coats the enamel around the brackets and prevents food and bacteria from collecting around and under the brackets. Another product used in this study, Cervitec Plus is a further development of Cervitec, a protective varnish containing chlorhexidine. The caries preventive effect of Cervitec during orthodontic therapies has been investigated in two studies.19,20 Application of these products to the enamel surface could provide protection throughout the orthodontic treatment but they could also have an adverse effect on the bond strength of brackets, depending on the application method.5 The effects of similar products on the bond strength of lingual orthodontic brackets have not been elucidated yet. The differences of the etching surface and the anatomical surfaces might have an effect on bond strength quality and quantity of mandibular incisors.
Both of the products were applied around the bracket periphery in the present study, and the results revealed that neither the fluoride-releasing light cure resin nor the chlorhexidine varnish had a significant adverse effect on the enamel bond strength. This was in accordance with previous studies.21-23 In contrast to our findings, Meng et al.24 found that the application of acidulated phosphate fluoride after acid etching enamel had an adverse effect on orthodontic bond strength of human enamel. Additionally, Karaman and Uysal22 stated that different forms of antimicrobial varnishes have some effect on bond strength of orthodontic brackets.
Aegis Ortho which is a light-cured orthodontic adhesive containing Amorphous Calcium Phosphate (ACP), promotes the enhancement of the tooth's natural repair mechanism by releasing calcium and phosphate ions. A recent report has shown that the ACP-containing adhesive demonstrated a bond strength of 6.6 ± 1.5 MPa, and declared that although this adhesive demonstrated a low bond strength, it produced a consistent bond.12 Similarly we found a mean bond strength of 6.6 ± 0.6 MPa, which was significantly lower than the other groups. Consistent with previous studies, the antimicrobial self-etching system, Clearfil Protect Bond demonstrated the highest bond strength among the other groups.25,26 The mean bond strength value in this study was 15.9 ± 1.4 MPa, which was similar to the results of a previous study.25 The present bond strength values were found to be higher than Reynolds'27 minimal bond strength values that are clinically acceptable (5.9 - 7.8 MPa). However, lower incisors have thinner layers of enamel than other teeth which was claimed to limit their load dissipation potential resulting in enamel fracture. A bond strength greater than 8 - 9 MPa has been argued to exceed the clinical requirements.16 These results demonstrate that the use of Clearfil Protect Bond, especially where the enamel is likely to be thin may cause a safety issue for orthodontic purposes. On the other hand, current results depend on in-vitro evaluations, and none of the materials have been subjected to different features of an oral environment.
When the ARI scores were considered, a significant difference was observed for group 5, showing less composite remaining on the tooth after debonding when compared with the other groups (Table 2). The majority of the mean scores ranged around 2, indicating that most of the adhesive remained on the tooth surface after debonding in groups 1, 2, 3 and 4. The lowest ARI scores were found in group 4, indicating that almost all the adhesive remained on the tooth, which suggests that the bond between the bracket and the adhesive was weak. Although group 5 had the statistically highest bond strength value, ARI scores revealed that less adhesive resin remained on the enamel surface in this group. This suggests that the predominant mode of bracket failure was at the enamel-adhesive resin interface in Clearfil Protect Bond, which was in accordance with a previous report.28 There are conflicting results about the amount of residual adhesive on teeth which might have emanated from the different bonding systems, differences in the bracket sizes and designs, or the classification system of ARI.29,30 In our conception, high bond strength during orthodontic treatment and shorter chair time for residual resin removal during debonding would be beneficial in clinical performance. One of the major problems in lingual orthodontics is the clear up of composite from lingual tooth surfaces which is time consuming and uncomfortable for the patient. However, excessive bond strength and bracket failure at the enamel composite interface should be balanced in order to avoid enamel fractures.
The findings indicate that application of fluoride-releasing resin or chlorhexidine products did not significantly affect bond strength of lingual orthodontic brackets. Although acceptable bond strengths were observed in all tested groups, the excessive bond strength achieved with Clearfil Protect Bond should be taken into consideration especially where the enamel is thin.
Figures and Tables
References
1. Caniklioglu C, Oztürk Y. Patient discomfort: a comparison between lingual and labial fixed appliances. Angle Orthod. 2005. 75:86–91.
2. Hohoff A, Stamm T, Kühne N, Wiechmann D, Haufe S, Lippold C, et al. Effects of a mechanical interdental cleaning device on oral hygiene in patients with lingual brackets. Angle Orthod. 2003. 73:579–587.
3. Miyawaki S, Yasuhara M, Koh Y. Discomfort caused by bonded lingual orthodontic appliances in adult patients as examined by retrospective questionnaire. Am J Orthod Dentofacial Orthop. 1999. 115:83–88.

4. Sinclair PM, Cannito MF, Goates LJ, Solomos LF, Alexander CM. Patient responses to lingual appliances. J Clin Orthod. 1986. 20:396–404.
5. Bishara SE, Vonwald L, Zamtua J, Damon PL. Effects of various methods of chlorhexidine application on shear bond strength. Am J Orthod Dentofacial Orthop. 1998. 114:150–153.

6. Mattingly JA, Sauer GJ, Yancey JM, Arnold RR. Enhancement of Streptococcus mutans colonization by direct bonded orthodontic appliances. J Dent Res. 1983. 62:1209–1211.

7. Scheie AA, Arneberg P, Krogstad O. Effect of orthodontic treatment on prevalence of Streptococcus mutans in plaque and saliva. Scand J Dent Res. 1984. 92:211–217.

8. Corbett JA, Brown LR, Keene HJ, Horton IM. Comparison of Streptococcus mutans concentrations in non-banded and banded orthodontic patients. J Dent Res. 1981. 60:1936–1942.

9. Lundström F, Krasse B. Streptococcus mutans and lactobacilli frequency in orthodontic patients; the effect of chlorhexidine treatments. Eur J Orthod. 1987. 9:109–116.

10. El Bokle D, Munir H. An in vitro study of the effect of Pro Seal varnish on the shear bond strength of orthodontic brackets. World J Orthod. 2008. 9:141–146.
11. Sköld-Larsson K, Borgström MK, Twetman S. Effect of an antibacterial varnish on lactic acid production in plaque adjacent to fixed orthodontic appliances. Clin Oral Investig. 2001. 5:118–121.

12. Foster JA, Berzins DW, Bradley TG. Bond strength of an amorphous calcium phosphate-containing orthodontic adhesive. Angle Orthod. 2008. 78:339–344.

13. Imazato S, Kinomoto Y, Tarumi H, Torii M, Russell RR, McCabe JF. Incorporation of antibacterial monomer MDPB into dentin primer. J Dent Res. 1997. 76:768–772.

14. Imazato S, Kuramoto A, Takahashi Y, Ebisu S, Peters MC. In vitro antibacterial effects of the dentin primer of Clearfil Protect Bond. Dent Mater. 2006. 22:527–532.

15. Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982. 81:93–98.

16. Hobson RS, McCabe JF, Hogg SD. Bond strength to surface enamel for different tooth types. Dent Mater. 2001. 17:184–189.

17. Geiger AM, Gorelick L, Gwinnett AJ, Benson BJ. Reducing white spot lesions in orthodontic populations with fluoride rinsing. Am J Orthod Dentofacial Orthop. 1992. 101:403–407.

18. Hohoff A, Fillion D, Stamm T, Goder G, Sauerland C, Ehmer U. Oral comfort, function and hygiene in patients with lingual brackets. A prospective longitudinal study. J Orofac Orthop. 2003. 64:359–371.
19. Ogaard B, Larsson E, Glans R, Henriksson T, Birkhed D. Antimicrobial effect of a chlorhexidine-thymol varnish (Cervitec) in orthodontic patients. A prospective, randomized clinical trial. J Orofac Orthop. 1997. 58:206–213.
20. Øgaard B, Larsson E, Henriksson T, Birkhed D, Bishara SE. Effects of combined application of antimicrobial and fluoride varnishes in orthodontic patients. Am J Orthod Dentofacial Orthop. 2001. 120:28–35.

21. Bishara SE, Damon PL, Olsen ME, Jakobsen JR. Effect of applying chlorhexidine antibacterial agent on the shear bond strength of orthodontic brackets. Angle Orthod. 1996. 66:313–316.
22. Karaman AI, Uysal T. Effectiveness of a hydrophilic primer when different antimicrobial agents are mixed. Angle Orthod. 2004. 74:414–419.
23. Wang WN, Sheen DH. The effect of pretreatment with fluoride on the tensile strength of orthodontic bonding. Angle Orthod. 1991. 61:31–34.
24. Meng CL, Li CH, Wang WN. Bond strength with APF applied after acid etching. Am J Orthod Dentofacial Orthop. 1998. 114:510–513.

25. Arhun N, Arman A, Sesen C, Karabulut E, Korkmaz Y, Gokalp S. Shear bond strength of orthodontic brackets with 3 self-etch adhesives. Am J Orthod Dentofacial Orthop. 2006. 129:547–550.

26. Bishara SE, Soliman M, Laffoon J, Warren JJ. Effect of antimicrobial monomer-containing adhesive on shear bond strength of orthodontic brackets. Angle Orthod. 2005. 75:397–399.
28. Korbmacher HM, Huck L, Kahl-Nieke B. Fluoride-releasing adhesive and antimicrobial self-etching primer effects on shear bond strength of orthodontic brackets. Angle Orthod. 2006. 76:845–850.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download