Abstract
Purpose
The aim of study was to determine the level of the radiation exposure of surgical staff during surgical probe applications in breast cancer.
Methods
Three operations of a sentinel lymph node biopsy were randomly selected. Spaced circles (50 cm apart) were drawn surrounding the operation bed on the floor. Tc-99m nanocolloid was injected peritumorally and intradermally into a patient. The radiation dose was measured with a GeigerMueller counter placed according to the drawn circles at distances of 50-200 cm from the side of patient's head and bilateral chest while the patient lay on the operation bed. All of the surgical procedures were recorded with a video camera and were monitored.
Sentinel lymph node (SLN) is the first lymph node of the tumor's lymphatic drainage. SLN biopsy gives information about the tumoral infiltration of SLN. The exclusion of metastasis in SLN makes the regional lymph node dissection unnecessary.(1-4) Only the 30% and 10% of the axillary lymph node dissections are positive for palpable breast carcinomas and non-palpable breast carcinomas, respectively. This means 70-90% of axillary lymph node dissections are unnecessary.(5,6) The complications of axillary lymph node dissection are ipsilateral arm edema, hematoma, neuropathy and infections. Therefore, SLN biopsies can prevent unnecessary surgery and related complications.
The radionuclide Tc-99m is used in many medical radioactive diagnostic tests because of short half-life (T1/2=6.01 hr), the energy of the gamma ray it emits (140 keV), and the ability of technetium to be chemically bound to many biologically active molecules.(7) The short-lived gamma-emitting radionuclide technetium-99m is used as a label for the colloid for sentinel lymph node detection. However, the use of radioactive materials in the surgery room generates concern among the staff about the radiation exposure. The aim of this study is to develop a method to estimate and to calculate the radiation exposure of the surgical staff in surgical probe applications during sentinel lymph node biopsy for breast cancer.
This study was approved by the institutional review board of the Dokuz Eylül University radiation security committee. Three operations of sentinel lymph node biopsy for breast cancer were randomly selected. Lymphoscintigraphy was performed for sentinel lymph node detection for these three patients in the morning of the operation day. Tc-99m nanocolloid (Nycomed Amersham SorinS.r.I., with colloidal diameter ≤80 nm, GE Healthcare, Milan, Italy) was injected peritumorally (four quadrants around the tumor, 150 µCi/0.5 cc each) and intradermally (skin location of tumor, 200 µCi/0.1 cc) in the first two operations. Tc-99m nanocolloid was injected peritumorally (four quadrants around the tumor, 250 µCi/0.5 cc each) and intradermally (skin location of tumor, 200 µCi/0.1 cc) in the third operation. The lymphoscintigraphy was then performed at the anterior and prone lateral static image up to two hours. The patients entered the operation room 3 hr after radiocolloid injection. Spaced circles (50 cm apart) were drawn surrounding the operation bed on the floor of the operation room with a pen prior to the operations (Figure 1). In the operation room, the radiation dose was measured with a calibrated hand-held Geiger Mueller counter (Morgan, Series 1000, Mini Instrument Ltd., Wiltshire, England) (µSv/hr) at the circles drawn at distances of 50 cm, 100 cm, 150 cm, and 200 cm from the side of the patient's head, right and left chest while the patient lay on the operation bed prior to the operation. Sentinel lymph node was detected in all patients by gamma probe (Navigator GPS, probe head diameter 14 mm, energy spectrum 27-364 keV, maximum count rate 25,000 cps, detector material CdTe) during the operation. Breast protecting surgery and SLN biopsies were performed for all of the patients. All operations were recorded throughout with a video camera in the operation room. Three nuclear medicine physicians monitored all of the camera recordings. The working times of all of the surgical staff (anesthetist, senior surgeon, first assistant surgeon, second assistant surgeon and nurse) in the circles at the certain distances during the operation were recorded and whole body doses of the surgical staff were calculated by multiplying the time spent at each distance by the dose rate at that distance formulated using the following formula ([R=Σrd×hd] d: distance in cm, r: measured dose rate in µSv/hr, R: calculated total dose in µSv). The calculated doses were compared with the annual dose limits recommended by the International Commission on Radiological Protection (ICRP). Figure 2 shows the setting of the operation room.
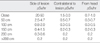
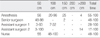
The dose rates at each distance are shown in Table 1. The mean duration of operation was 100 min. The working times of the surgical staff in the circles are shown in Table 2. The least and highest exposure of the surgical staff were calculated as 0.18-0.65 µSv for the anesthetist, 2.00-4.70 µSv for the senior surgeon, 0.65-4.30 µSv for the first assistant surgeon, 0.08-0.83 µSv for second assistant surgeon, and 0.40-0.50 µSv for the nurse (Table 3). As there were three measurements, the dose rates and working times are given in a minimum to maximum ranges.
The annual dose limit to the whole body for a radiation worker is 20 mSv (20,000 µSv/yr), and for a member of the public the annual dose limit is 1 mSv (1,000 µSv/yr) as recommended by the ICRP.(8) The minimum to maximum whole body dose to the senior surgeon resulting from surgery performed on a sentinel node patient was 2.00-4.70 µSv. According to these measured doses, a senior surgeon can perform 212-500 procedures per year in order to reach the annual dose limit for a member of the public and can perform 4,255-10,000 procedures per year in order to reach the dose limit of a radiation worker.
Tc-99m labeled colloids for lymphoscintigraphy and radioguided surgery do not cause any relevant radiation burden to patients.(9-13) Very low doses of Tc-99m are injected into patients and 2-3 hr elapse between the Tc-99m nanocolloid injection and the surgical procedure. However, the need for radiation protection during sentinel lymph node biopsy sometimes concerns the surgical staff involved in the procedure including the anesthetist, surgeon, nurse and sometimes the pathologist. Unfortunately, there has been limited information available regarding the radiation safety of sentinel lymph node biopsy.
Stratmann et al.(9) studied 20 breast cancer patients, who underwent a sentinel lymph node biopsy. Radiation exposure was measured with a hand-held Geiger counter. The dose rates from the breast injection site before skin incision, lumpectomy specimens and sentinel nodes were measured at distances of 3, 30, and 300 cm. The exposure to the surgeon's torso was determined as 13.3 µSv/hr.(9) Waddington et al.(10) showed that the mean whole-body dose to the surgical staff resulting from surgery performed on a sentinel node biopsy patient was 0.34 µSv, a the maximum recorded dose below 2 µSv. Brenner et al.(14) reported the whole-body doses of 0.45 mSv, 0.11 mSv, 0.05 mSv, and 0.21 mSv for the surgeon, the operating room nurse, the anesthetist, and the pathologist, respectively. De Kanter et al.(15) published data regarding the radiation dose to the operating room personnel from patients who underwent a sentinel node biopsy for breast cancer. The dose to the thoracic wall, to the abdominal wall and both the dose to the hands of the surgeon and the assistant were measured with small thermoluminoscent-dosemeters. The exposure to the thoracic wall of the surgeon was 3.7 µSv and the dose to the abdominal wall was 8.2 µSv.(15)
In our study we found the total radiation exposure of the senior surgeon during all of the operations as 2.00-4.70 µSv. Though the time spent at each distance may vary for the other staff members, the senior surgeon spent most of his/her time at 0.5 m circle.
The exposure rate may also be influenced by the amount of radiocolloid injected and the time of surgery after injection. Operating the next day after the injection of the radiocolloid minimizes the exposure rate.(10,16) The exposure of the staff will increase if the patient is operated a few hours after surgery but still this radiation exposure level is very small and the level represents a very small fraction of the dose limit to a member of the public. The annual dose limit to the whole body for a member of the public recommended as 1,000 µSv per year as recommended by the ICRP and the senior surgeon can perform 212-500 procedures per year in order to reach the annual dose limit for a the member of the public.(8) If a surgeon performs more than 212 procedures per year, although he/she is not classified as an occupational radiation worker, he/she should use a radiation dosimeter during the operation in order to measure the actual dose. In our opinion, the use of a lead shields is not necessary because operation rooms cannot reach the high levels that are classified as a radiation controlled area by the ICRP.(8)
The effective radiation dose for a chest X-ray is 20 µSv per procedure and a London-New York commercial flight results in an exposure of 60 µSv per flight; the dose from a single sentinel node biopsy is very low as compared to these exposures.(10) Using the method in this study, any staff member can calculate his/her own radiation exposure in a surgical procedure by measuring the dose rate at a distance and the time spent at that distance using the provided formula. The number of patients in this study is very limited but the aim was to describe a practical calculation method to estimate the dose to the surgical staff. Our dose calculation depends on the time spent at average distances and this method was not compared to any other method or measurement. Increasing the patient numbers may result in a change of the mean and standard deviation of the doses estimated for the staff, but this will not influence the method itself. The results can be compared to actual measurements to check for the validity of the estimation method.
Our method depends on the time spent at each distance in the operation. Therefore, we use Geiger Mueller counter in order to measured of radiation dose at the circles drawn at distances of 50 cm, 100 cm, 150 cm, and 200 cm from the side of the patient's head, right and left chest while the patient lay on the operation bed prior to the operation. Intrinsic inaccuracy of Geiger Mueller counter may result in a change of the mean of the doses estimated for the staff. Geiger Mueller counter was calibrated as systematic by Committee of Turkish Atomic Energy calibration accuracy: ±2% for two calibration point of Co-60 source.
We conclude that, the radiation exposure of the surgical staff from sentinel node detection procedure using radiocolloids is negligible and can be safely performed by the surgeons. The radiation risk to the surgical staff is low, and the classification of the personnel in the operating room as occupational radiation workers is not necessary.
Figures and Tables
References
1. Ivens D, Hoe AL, Podd TJ, Hamilton CR, Taylor I, Royle GT. Assessment of morbidity from complete axillary dissection. Br J Cancer. 1992. 66:136–138.

2. Maffioli L, Sturm E, Roselli M, Fontanelli R, Pauwels E, Bombardieri E. State of the art of sentinel node biopsy in oncology. Tumori. 2000. 86:263–272.

3. Sandrucci S, Casalegno PS, Percivale P, Mistrangelo M, Bombardieri E, Bertoglio S. Sentinel lymph node mapping and biopsy for breast cancer: a review of the literature relative to 4791 procedures. Tumori. 1999. 85:425–434.

6. Bombardieri E, Crippa F, Maffioli L, Draisma A, Chiti A, Agresti R, et al. Nuclear medicine approaches for detection of axillary lymph node metastases. Q J Nucl Med. 1998. 42:54–65.
7. Wilson MA. Textbook of nuclear medicine. 1998. Philadelphia: Lippincott-Raven;396.
8. International Commission on Radiological Protection. 1990 recommendations of the Internataional Commission on Radiological Protection. 1990. Oxford: Pergamon Press.
9. Stratmann SL, McCarty TM, Kuhn JA. Radiation safety with breast sentinel node biopsy. Am J Surg. 1999. 178:454–457.

10. Waddington WA, Keshtgar MR, Taylor I, Lakhani SR, Short MD, Ell PJ. Radiation safety of the sentinel lymph node technique in breast cancer. Eur J Nucl Med. 2000. 27:377–391.

11. Cremonesi M, Ferrari M, Sacco E, Rossi A, De Cicco C, Leonardi L, et al. Radiation protection in radioguided surgery of breast cancer. Nucl Med Commun. 1999. 20:919–924.

12. Eshima D, Fauconnier T, Eshima L, Thornback JR. Radiopharmaceuticals for lymphoscintigraphy: including dosimetry and radiation considerations. Semin Nucl Med. 2000. 30:25–32.

13. Miner TJ, Shriver CD, Flicek PR, Miner FC, Jaques DP, Maniscalco-Theberge ME, et al. Guidelines for the safe use of radioactive materials during localization and resection of the sentinel lymph node. Ann Surg Oncol. 1999. 6:75–82.

14. Brenner W, Ostertag H, Peppert E, Czech N, Kampen WU, Muhle C, et al. Radiation exposure to the personnel in the operating room and in the pathology due to SLN detection with Tc-99m-nanocolloid in breast cancer patients. Nuklearmedizin. 2000. 39:142–145.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download