Abstract
Purpose
To compare pain scores of patients during intravitreal 27-gauge bevacizumab and 30-gauge ranibizumab injection procedures.
Methods
Seventy eyes of 70 patients who had not previously undergone intravitreal anti-vascular endothelial growth factor therapy were included in this study. Thirty-five patients received ranibizumab and 35 patients received bevacizumab. The diagnoses of the patients were: 27 age related macular degeneration, 15 diabetic macular edema, 9 diabetic vitreous hemorrhage, 6 central retinal vein occlusion, 11 branch retinal vein occlusion and 2 central serous chorioretinopathy. Bevacizumab (1.25 mg/0.05 mL) was injected into the vitreous cavity using a 27-gauge needle, and ranibizumab (0.5 mg/0.05 mL) was injected with 30-gauge needle. Patients were asked just after the injection to rate their perceived pain during the injection using the visual analogue scale (VAS) of 0 (no pain) to 10 (unbearable/worst pain). The average of these scores was used as the primary outcome.
Results
The VAS pain scores in the ranibizumab and bevacizumab groups were 1.06 ± 0.91 (range, 0 to 3) and 1.94 ± 1.55 (range, 0 to 7), respectively, a significant difference (p = 0.005). Patients <65 and ≥65 years of age in both the ranibizumab and bevacizumab groups were then compared. For patients <65, there was a significant difference in the average VAS pain scores between groups (p = 0.003). However, for patients ≥65 years, there was not a significant difference in the average VAS pain scores between groups (p = 0.238). Female and male patients in both ranibizumab and bevacizumab groups were also compared. For female patients, there was a significant difference in the average VAS pain scores between groups (p = 0.016), although not for male patients (p = 0.078).
Recent clinical trials regarding intravitreal injection of anti-vascular endothelial growth factor (VEGF) agents have shown excellent results in the treatment of intraocular neovascular disorders, macular edema, neovascular glaucoma and various corneal neovascular diseases [1,2,3,4]. Over the past decade, intravitreal injection of anti-VEGF agents have gained tremendous acceptance among retinal specialists and become one of the most common intraocular procedures [5]. Minimizing patient pain is critical during intravitreal injection. Patient discomfort at the time of injection can lead to sudden movements of the eye, which can be associated with intraocular complications. In addition, patients with diseases such as cystoid macular edema and age-related macular degeneration that require multiple intravitreal injections may be less likely to continue intravitreal injection after a bad experience [6].
Bevacizumab and ranibizumab are currently the most commonly used anti-VEGF agents. Ranibizumab (Lucentis; Genentech, San Francisco, CA, USA), a fragment of a humanized monoclonal antibody against all VEGF isoforms, is prepared as a single-use glass vial designed to provide 0.05 mL for intravitreal injection with a 30-gauge needle [3]. Bevacizumab is a humanized monoclonal antibody that binds all isoforms of VEGF and interferes with receptor binding to inhibit its signal [2]. Currently, intravitreal injection of bevacizumab is off label and does not have any commercially available form. For clinical use, it has been dispensed into single-use syringes with 26- to 30-gauge needles [7,8].
Despite the common use of intravitreal injections, there have been only a few studies that have investigated injection-related pain [8,9]. Thus, the aim of this study was to compare pain scores of patients during intravitreal 27-gauge bevacizumab and 30-gauge ranibizumab (Lucentis) injection procedures.
This prospective, interventional, non-randomized, comparative study was carried out at Department of Ophthalmology, Adıyaman University. All procedures followed the Declaration of Helsinki, and written informed consent was obtained from all patients. They were all informed of the off-label use of the bevacizumab and its potential risks and benefits.
Seventy eyes of 70 patients who had not previously undergone intravitreal anti-VEGF therapy were included in this study. Exclusion criteria were history of previous eye surgery other than for cataract, herpetic eye disease, glaucoma, uveitis, active conjunctivitis, keratitis and bullous keratopathy. Patients with poor cooperation in using the visual analogue scale (VAS) and/or using systemic analgesics or sedative medications were also excluded.
Thirty-five patients received ranibizumab and 35 patients received bevacizumab. Patients were first given topical anesthetic proparacaine 0.5% (Alcaine, Alcon-Couvreur, Puurs, Belgium) and povidone-iodine 5% drops. After 5% povidone-iodine was applied to the operating field, an eyelid speculum was positioned in order to stabilize the eyelids. Injections were performed one minute after instillation of the proparacaine drop. Bevacizumab (1.25 mg/0.05 mL) was previously dispensed into single-use 27-gauge needle syringes using an aseptic technique and was injected into the vitreous cavity through the pars plana at the inferotemporal quadrant, 3.5 to 4.0 mm posterior to the limbus. Ranibizumab (0.5 mg/0.05 mL) was injected with a 30-gauge needle using the same method. All injections were performed in the operating room.
Patients were asked just after the injection to rate their perceived pain during the injection on a VAS of 0 (no pain) to 10 (unbearable/worst pain). The average of these scores was used as the primary outcome.
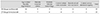
The diagnoses of the patients in the study are summarized in Table 1. The mean age was 60.43 ± 12.13 (range, 42 to 83) in the ranibizumab group and 64.86 ± 10.04 (range, 41 to 81) in the bevacizumab group. The mean age of the groups was similar (p = 0.151). In the ranibizumab group, 16 patients were male and 19 were female. In the bevacizumab group, 18 patients were male and 17 were female. The sex distribution between groups was also similar (p = 0.811). The VAS pain scores in the ranibizumab and bevacizumab groups were 1.06 ± 0.91 (range, 0 to 3) and 1.94 ± 1.55 (range, 0 to 7), respectively (Fig. 1), a significant difference (p = 0.005).
Patients were divided into two groups according to age: <65 and ≥65 years [9]. In the ranibizumab group, 16 patients were <65 and 19 patients were ≥65. There was not a significant difference in the average VAS pain scores between groups ( p = 0.145). The VAS pain scores in the younger and older groups were 0.81 ± 0.91 and 1.27 ± 0.87, respectively. In the bevacizumab group, 14 patients were <65 and 21 patients were ≥65. There was not a significant difference in the average VAS pain scores between groups (p = 0.339). VAS pain scores in younger and older groups were 2.29 ± 1.49 and 1.76 ± 1.61, respectively.
Patients <65 years of age in both the ranibizumab (16 patients) and bevacizumab (14 patients) groups were compared. There was a significant difference in the average VAS pain scores between groups (p = 0.003). The VAS pain scores in the ranibizumab and bevacizumab groups were 0.81 ± 0.91 and 2.29 ± 1.49, respectively.
Patients ≥65 years of age in both the ranibizumab (19 patients) and bevacizumab (21 patients) group were compared. There was not a significant difference in the average VAS pain scores between groups (p = 0.238). The VAS pain scores in the ranibizumab and bevacizumab groups were 1.27 ± 0.87 and 1.76 ± 1.61, respectively.
Patients were divided into two groups according to sex. In the ranibizumab group, there was not a significant difference in the average VAS pain scores between sexes (p = 0.481). The VAS pain scores in the male and female groups were 0.93 ± 0.77 and 1.16 ± 1.01, respectively. Nor was there a significant difference between sexes in average VAS pain score in the bevacizumab group (p = 0.163). The VAS pain scores in the male and female groups were 1.61 ± 1.29 and 2.35 ± 1.77, respectively.
Female patients in both the ranibizumab (19 patients) and bevacizumab (17 patients) groups were compared. There was a significant difference in the average VAS pain scores between groups (p = 0.016). The female VAS pain scores in the ranibizumab and bevacizumab groups were 1.16 ± 1.01 and 2.35 ± 1.77, respectively.
Male patients in both the ranibizumab (16 patients) and bevacizumab (18 patients) groups were compared. There was not a significant difference in the average VAS pain scores between groups (p = 0.078). The male VAS pain scores in the ranibizumab and bevacizumab groups were 0.93 ± 0.77 and 1.61 ± 1.29, respectively.
VAS is frequently used as an assessment instrument to evaluate the analgesic effects of various therapies and to detect minute pain changes during analgesic administration. VAS is a simple tool to use on anyone cognitively capable of understanding the parameters and responding to clinician instructions. Indeed, its popularity is frequently attributed to the ease and convenience in a fast-paced clinical setting [10]. VAS has been widely used in ophthalmologic research [11,12,13,14]. We evaluated the pain experiences of the patients with VAS because of its easy and quick use.
Moisseiev et al. [8] evaluated the correlation between pain associated with intravitreal bevacizumab injection and the location of the injection. They did not find any statistically significant difference in terms of pain experience between anatomical quadrants. In order to achieve standardization, we performed all injections into the inferotemporal quadrant. Knecht et al. [15] compared tunneled scleral intravitreal injection with straight scleral intravitreal injection in terms of short-term intraocular pressure changes, occurrence and amount of vitreous reflux, and patient discomfor. They did not find a difference in patient discomfort or intraocular pressure increase after the injection between groups. We used a straight injection technique in all patients.
Green-Simms et al. [7] surveyed the intravitreal injection technique practice patterns of retinal specialists in the United States. They found that a majority of the survey participants used a 30-gauge needle for the intravitreal injection of ranibizumab (78%) and bevacizumab (60%).
The studies that have evaluated pain scores of patients during intravitreal injection with different needle calibers have reported contrasting results. Rodrigues et al. [16] reported that the patients injected with a 26- or 27-gauge needle experienced more pain compared to those injected with 29- or 30-gauge needles. Eaton et al. [17] reported that injections with a 33-gauge device were significantly faster, but there was no significant difference in the levels of pain between a 33-gauge device and a standard 30-gauge needle. Rifkin and Schaal [9] used 27- and 30-gauge needles for injection and determined that the caliber of the needle did not significantly affect the pain score. We found that intravitreal injection with a 30-gauge needle was less painful for the patients. According to our experience, it is easier and safer to pierce the sclera with a 30-gauge needle than a 27-gauge needle during intravitreal injection. One patient, a 43-year-old woman diagnosed with diabetic macular edema, experienced a complication during the intravitreal 27-gauge bevacizumab injection. The patient reported extreme pain during the intravitreal injection as the reason for head movement. The tip of the 27-guage needle touched the posterior capsule of the crystalline lens. Cataract development was detected at the control visit. The cataract was removed with a phacoemulsification technique, and a foldable IOL was placed into the sulcus.
A 27-gauge needle has a diameter of 413 µm, and a 30-gauge needle has a diameter of 311-µ [9]. Pulido et al. [18] reported that 27-gauge needles require almost twice the force to penetrate the sclera than 30- or 31-gauge needles. This may explain why patients experienced less pain with the 30-gauge needle in our study.
Rifkin and Schaal [9] demonstrated that the pain score was not significantly related to diagnosis. Moisseiev et al. [8] also did not find a significant difference in the pain scores between any of the indications for the injection. We did not evaluate the relationship between the diagnosis and pain scores in this study.
Rifkin and Schaal [9] determined that patients aged >65 years reported a lower average pain score than those aged <65 years. Moisseiev et al. [8] found no correlation between pain score and patient age. To minimize the age factor, we formed two groups with similarly aged patients. We conducted a subgroup analysis according to two age groups: <65 and ≥65. Patients <65 years of age in the ranibizumab group reported a lower average pain score than those in the bevacizumab group. Patients ≥65 years old in the ranibizumab and bevacizumab groups were also compared, demonstrating no significant difference in average VAS pain scores.
Rifkin and Schaal [9] showed that female sex was associated with a lower post-injection pain score. Moisseiev et al. [8] demonstrated no statistically significant difference in pain score according to sex. In our study, there were no pain score differences between the sexes in the ranibizumab and bevacizumab groups. We also conducted a subgroup analysis for each sex. Female patients in the ranibizumab group reported a lower average pain score than those in the bevacizumab group. There was not a significant difference in the average pain score in male patients between the ranibizumab and bevacizumab groups.
Our study had some limitations. Forming the groups with same drug might have been more appropriate. Sensory innervation of the eye is provided by the peripheral axons of the primary sensory neurons located in the trigeminal ganglion [19]. The sensory nerves enter the eyeball mainly through the ciliary nerves and innervate all ocular tissues with the exception of the lens and the retina [19]. Since the retina has no nociceptors, and an equal volume of the drug was injected in both groups, we assumed that the pain sensation during intravitreal injection was mainly due to the caliber of the needle and so separated the patients accordingly. Another limitation of the study was the subjective character of the VAS. However, since there is not a quantitative technique to evaluate the amount of pain, the VAS was our best option.
In conclusion a 30-gauge intravitreal injection is more comfortable than a 27-gauge injection. Injection of bevacizumab with a 30-gauge needle syringe may be more tolerable for patients.
Figures and Tables
References
1. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006; 355:1419–1431.
2. Avery RL, Pearlman J, Pieramici DJ, et al. Intravitreal bevacizumab (Avastin) in the treatment of proliferative diabetic retinopathy. Ophthalmology. 2006; 113:1695.
3. Pieramici DJ, Rabena M, Castellarin AA, et al. Ranibizumab for the treatment of macular edema associated with perfused central retinal vein occlusions. Ophthalmology. 2008; 115:e47–e54.
4. Park SC, Su D, Tello C. Anti-VEGF therapy for the treatment of glaucoma: a focus on ranibizumab and bevacizumab. Expert Opin Biol Ther. 2012; 12:1641–1647.
5. Peyman GA, Lad EM, Moshfeghi DM. Intravitreal injection of therapeutic agents. Retina. 2009; 29:875–912.
6. Tewari A, Shah GK, Dhalla MS, Blinder KJ. Surface anesthesia for office-based retinal procedures. Retina. 2007; 27:804–805.
7. Green-Simms AE, Ekdawi NS, Bakri SJ. Survey of intravitreal injection techniques among retinal specialists in the United States. Am J Ophthalmol. 2011; 151:329–332.
8. Moisseiev E, Regenbogen M, Bartfeld Y, Barak A. Evaluation of pain in intravitreal bevacizumab injections. Curr Eye Res. 2012; 37:813–817.
9. Rifkin L, Schaal S. Factors affecting patients' pain intensity during in office intravitreal injection procedure. Retina. 2012; 32:696–700.
10. Reed MD, Van Nostran W. Assessing pain intensity with the visual analog scale: a plea for uniformity. J Clin Pharmacol. 2014; 54:241–244.
11. Aslankurt M, Aslan L, Baskan AM, et al. Pain and cooperation in patients having dominant-side or nondominant-side phacoemulsification. J Cataract Refract Surg. 2014; 40:199–202.
12. Mirshahi A, Lashay A, Roozbahani M, et al. Pain score of patients undergoing single spot, short pulse laser versus conventional laser for diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol. 2013; 251:1103–1107.
13. Chen D, Lian Y, Li J, et al. Monitor corneal epithelial healing under bandage contact lens using ultrahigh-resolution optical coherence tomography after pterygium surgery. Eye Contact Lens. 2014; 40:175–180.
14. Narvaez J, Wessels I, Bacon G, et al. Prospective randomized evaluation of short-term complications when using buffered or unbuffered lidocaine 1% with epinephrine for blepharoplasty surgery. Ophthal Plast Reconstr Surg. 2010; 26:33–35.
15. Knecht PB, Michels S, Sturm V, et al. Tunnelled versus straight intravitreal injection: intraocular pressure changes, vitreous reflux, and patient discomfort. Retina. 2009; 29:1175–1181.
16. Rodrigues EB, Grumann A Jr, Penha FM, et al. Effect of needle type and injection technique on pain level and vitreal reflux in intravitreal injection. J Ocul Pharmacol Ther. 2011; 27:197–203.
17. Eaton AM, Gordon GM, Wafapoor H, et al. Assessment of novel guarded needle to increase patient comfort and decrease injection time during intravitreal injection. Ophthalmic Surg Lasers Imaging Retina. 2013; 44:561–568.
18. Pulido JS, Zobitz ME, An KN. Scleral penetration force requirements for commonly used intravitreal needles. Eye (Lond). 2007; 21:1210–1211.
19. Levin LA, Nilsson SF, Hoeve JV, Wu S. Adler's physiology of the eye. In : Levin LA, Nilsson SF, Hoeve JV, Wu S, editors. Sensory innervation of the eye. 11th ed. London: Elsevier;2011. p. 363–384.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download