Abstract
We report a rare case of a giant ovarian tumor presenting as an incarcerated umbilical hernia. A 61-yr-old woman was admitted to the hospital with severe abdominal pain, an umbilical mass, nausea and vomiting. On examination, a large, irreducible umbilical hernia was found. The woman underwent an urgent operation for a possible strangulated hernia. A large, multilocular tumor was found. The tumor was excised, and a total abdominal hysterectomy and bilateral salphingo-oophorectomy were performed. The woman was discharged 6 days after her admission. This is the first report of incarcerated umbilical hernia containing a giant ovarian tumor within the sac.
Because of serious complications such as rupture and strangulation of the hernia content, incarceration of the umbilical hernia is a significant surgical condition (1). The small bowel, the omentum and the large bowel are frequently seen in the hernia sac. However, incarceration of intra-abdominal tumors is rare. In this case report, we present a patient with an incarcerated umbilical hernia caused by a giant ovarian tumor.
A 61-yr-old woman was admitted to the emergency department with symptoms of sudden abdominal pain, nausea, vomiting and painful swelling in a previously diagnosed umbilical hernia. She had had severe abdominal pain and the sensation of a mass for the previous 2 hr. Because of her low socioeconomic status, she had no history of routine healthcare, and she had a history of uncontrolled hypertension.
On examination, she had a 15×10 cm, irreducible, purple-colored umbilical hernia, and there was extreme tenderness and hyperemia on hernia. Because of the incarcerated umbilical hernia and possible strangulation of the hernia content, the patient underwent an urgent operation without any diagnostic evaluation.
During the operation, a partial omental infarct and an intraabdominal tumor were found in the hernia sac (Fig. 1). A partial omentectomy was performed, and abdominal incision was extended from pubis to the epigastrium. A large, multilocular, left ovarian cyst, which extended from the transverse colon to rectovesical space, was observed (Fig. 2). After dissecting the tumor from the adjacent tissues, tumor excision, total abdominal hysterectomy and bilateral salphingo-oophorectomy were performed with no complications. During the operation, a frozen section was unavailable. The abdominal wall was closed with primary continuous sutures.
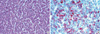
The resected tumor measured as 25×23×16 cm and weighed 3,680 g. On microscopic examination, the tumor was uniform and composed of pale oval cells with prominent grooves (coffee bean appearance). The diagnosis of a granulosa cell tumor was supported by the immunohistochemical expression of inhibin in the neoplastic cells (Fig. 3).
Because she had high blood pressure, the patient was followed-up in the intensive care unit. The hypertension was controlled, and the patient recovered uneventfully. She was discharged 6 days after her admission. About 2 weeks after discharge, she underwent second operation (ie, a staging operation) that used the same incision. An omentectomy, a paraaortic and pelvic lymphadenectomy, peritoneal washing, cytology analysis, and peritoneal biopsies were done at that time, and no metastases were found. After the second operation, combination chemotherapy with bleomycin (10 mg/m2), cisplatin (100 mg/m2) and etoposide (100 mg/m2) was begun.
A granulosa cell tumor of the ovary is an uncommon neoplasm derived from granulosa cells. It occurs in 2% to 5% of all ovarian cancers (2). Although it can be seen at any age, it occurs most commonly during the perimenopausal and early postmenopausal years. The incidence of granulosa cell tumors has been reported to be 0.4 to 1.7 per 100,000 women (2). Survival of patients with granulosa cell tumors is good. Surgery is the main therapy for tissue diagnosis and staging. Postoperative chemotherapy is given for patients with granulosa cell tumors that are of stages II, III, and IV. However, some patients with large stage-I tumors (ie, those >10-15 cm), a high mitotic index, tumor rupture or all or any combination of these can be considered for adjuvant chemotherapy (2). This is why we gave adjuvant chemotherapy to our patient: because of the high risk of recurrence. However the benefit of adjuvant chemotherapy for high-risk stage-I patients has not been supported by prospective randomized studies (2).
The umbilicus is a site at which intra-abdominal cancer metastases that are inoperable can be seen, beacuse the tumors appear as a characteristic Sister Mary Joseph's nodule. However, primary tumors that protrude into the umblical hernia sac are uncommon. The small bowel, the omentum, and the large bowel are frequently seen within the hernia sac (3). Other intra-abdominal organs are rarely seen in the sac. Rare cases including gallstones after a laparoscopic cholecystectomy, perforated acute appendicitis, strangulated Meckel's diverticulum, myomatous uterus, and incarcerated pregnant uterus in the umbilicus have been reported (3).
Millar and associates reported a patient similar to ours: theirs was the first report of a reducible umbilical hernia with an ovarian tumor (4). But ours is the first report of an incarcerated umbilical hernia with a giant ovarian tumor. Uludağ and associates reported incarceration of an umbilical hernia during pregnancy because of a sessile fibroid (1), and Wong (5) reported a uterine fibroid presenting as an incarcerated umbilical hernia during pregnancy.
In conclusion, intra-abdominal tumors presenting as incarcerated or strangulated hernias are extremely rare but do occasionally occur. If it is not suspected before surgery, a careful exploration is needed to identify the content. In such cases, diagnostic biopsies, mass resections, or both, with primary hernia repairs are sufficient procedures for a first step. Definitive surgery for the primary disease should be planned after doing a detailed evaluation of the patient and consulting with the related surgical branches in elective surgery services.
Figures and Tables
References
1. Uludag M, Yetkin G, Demirel M, Citgez B, Isgor A. Incarceration of umbilical hernia during pregnancy due to a sessile fibroid. Hernia. 2006. 10:357–359.
2. Schumer ST, Cannistra SA. Granulosa cell tumor of the ovary. J Clin Oncol. 2003. 21:1180–1189.
3. Daoud FS. Incarcerated endometriotic ovarian cyst within paraumbilical hernia. J Obstet Gynaecol. 2005. 25:828–829.
4. Millar RC, Geelhoed GW, Ketcham AS. Ovarian cancer presenting as umbilical hernia. J Surg Oncol. 1975. 7:493–496.
5. Wong C. A uterine fibroid presenting as an incarcerated umbilical hernia during pregnancy. Hernia. 2005. 9:298–299.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download