DISCUSSION
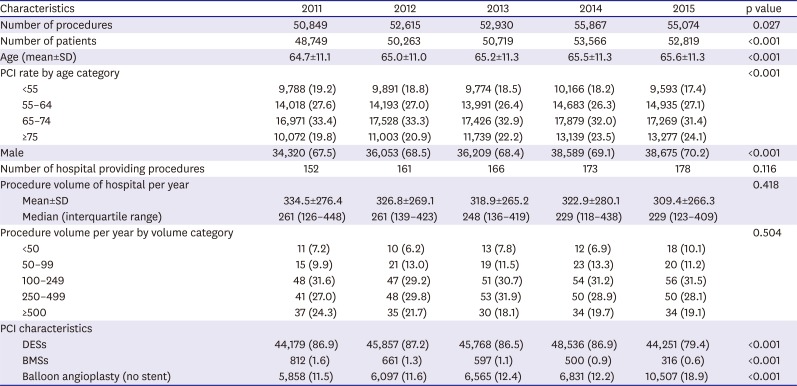
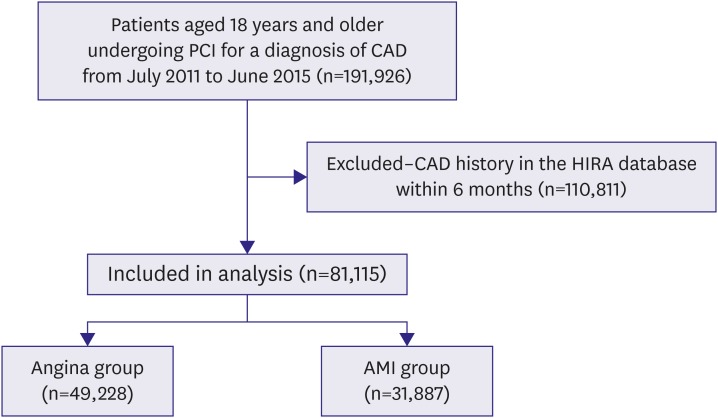
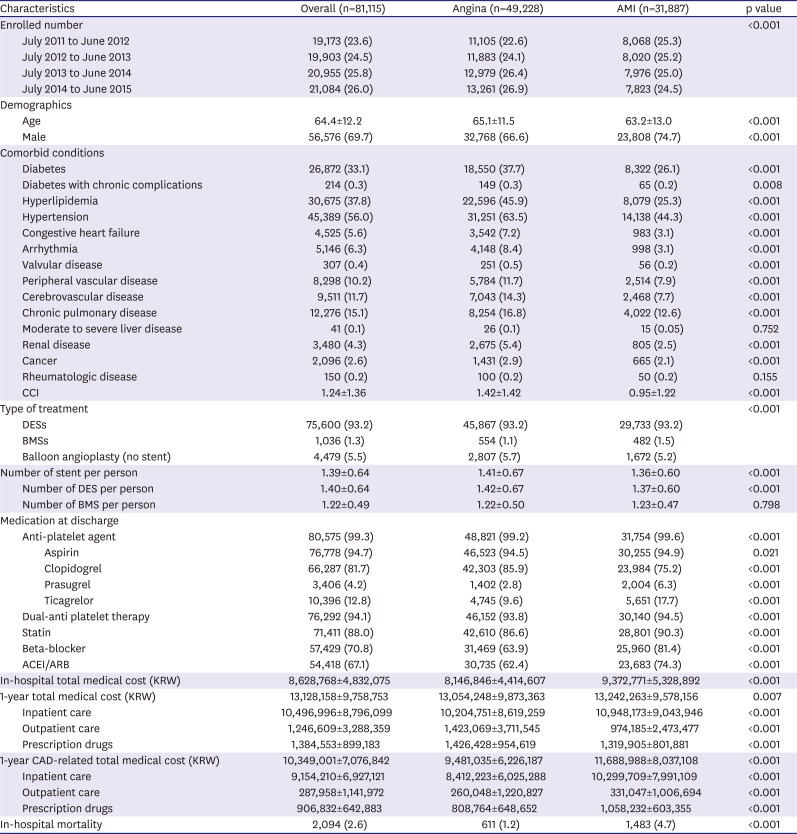
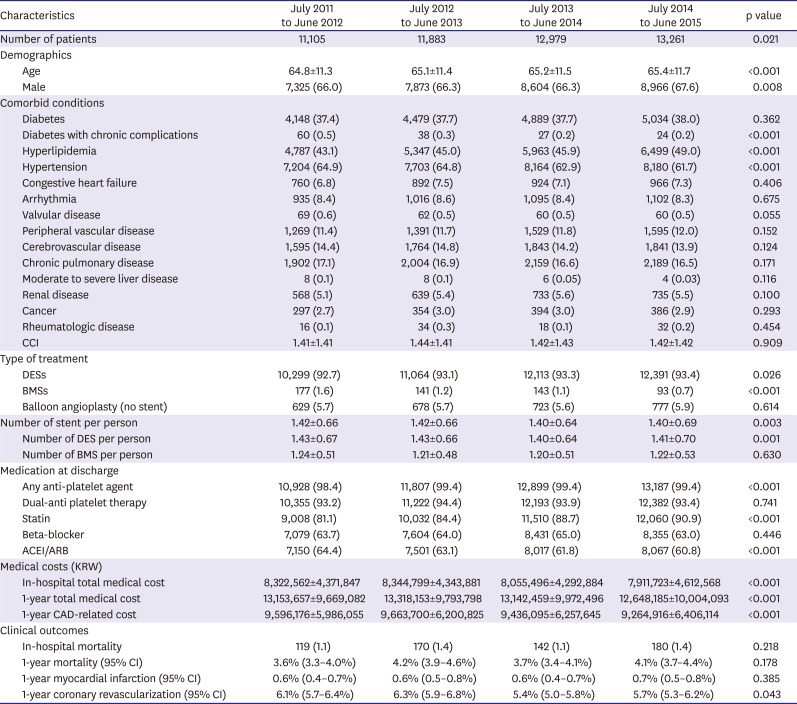
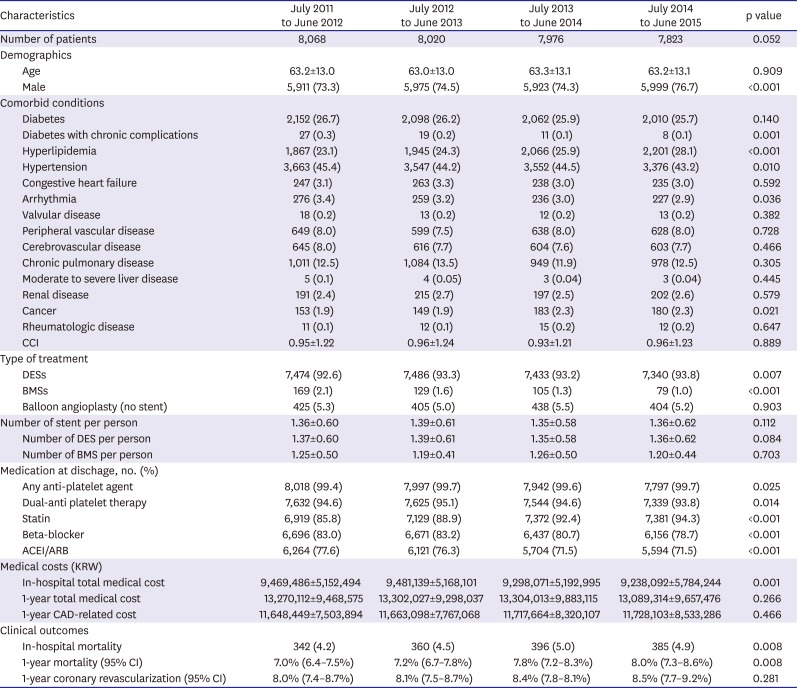
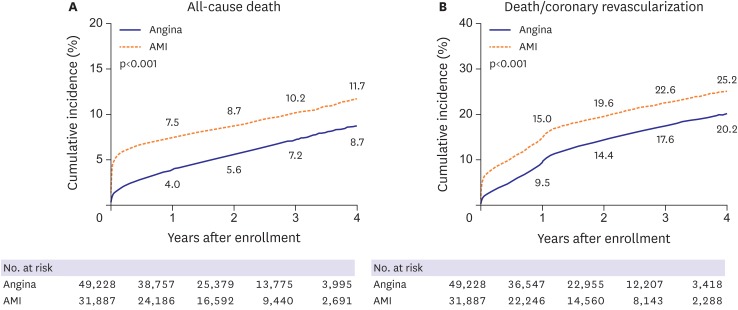
In the present analysis using NHI claims data in Korea, our main findings were as follows: 1) In patients who underwent PCI for the first episode of CAD, the number of patients for angina significantly increased, but the number of those for AMI marginally decreased; 2) Irrespective of clinical presentations, DES was the most commonly used device; 3) The use of medication at discharge was still inappropriate and clinical outcomes did not improve between 2011–2012 and 2014–2015.
There are limited data available to provide a contemporary snapshot of PCI in Korea. A recent large-scale multicenter registry described the current status of PCI in Korea.
3)4) However, these efforts may be limited somewhat either by short-term clinical outcomes or institutional selection. Therefore, considering the nationwide situation in clinical practices, this present study was designed. Well-controlled and reliable data from the HIRA database in Korea (i.e., a quasigovernmental organization) enabled to provide an overview of the national trends for PCI. In addition, compared with the 2014 Korean Percutaneous Coronary Intervention (K-PCI) registry,
3)4) the similar age ranges for patients and similar proportion of male, diabetes, hypertension, hyperlipidemia, and intervention for AMI or angina were noted. The frequency of DES usage (93.2% vs. 91.3%) and in-hospital mortality (2.6% vs. 2.3%) did not differ between our study and the 2014 K-PCI registry. Therefore, we believe that this study reflects the contemporary status of PCI in Korea.
In Korean patients undergoing PCI for the first episode of CAD, the total number of PCI procedures increased between 2011 and 2015, with a progressive increase of patients with angina and a gradual decline of those with AMI. With cognition of importance and impact of cardiovascular disease, in many western countries, health programs have been developed for the prevention and management of major cardiovascular risk factors such as diabetes, hypertension, and hyperlipidemia.
11)12) Consequently, control of these cardiovascular risk factors has improved cardiovascular outcomes in these countries.
13)14) In Korea, CAD has become one of the leading causes of death because of prolonged life expectancy and rapid westernization.
15)16) In the present study, no significant changes in comorbid conditions reflected by the CCI were detected in angina group between 2011–2012 and 2014–2015. However, the absolute number of patients with major risk diseases such as diabetes, hyperlipidemia, and hypertension increased in the same period. In AMI group, although the proportion of diabetes or hypertension was stabilized, the proportion of hyperlipidemia also increased during 4 years. Therefore, to reduce the burden of CAD in Korea, tailored management for cardiovascular risk factors with a risk prediction model, considering differences of risk factors attributable to development of CAD in a Korean population, is necessary.
In the early-generation DES, clinical data were challenged by less favorable long-term safety issues such as stent thrombosis and late failure.
17)18) Accordingly, these findings led to a marked improvement in stent design, and the development of new drugs and drug-carrier systems. Based on these enhanced properties, newer-generation DES demonstrated better clinical efficacy and safety than those of BMS and first-generation DES.
19)20) A registry data also indicated that routine use of DES was associated with a decline in the incidence of restenosis and stent thrombosis.
21) Furthermore, even in patients with ST-segment-elevation myocardial infarction, newer-generation DES showed advantages in efficacy and safety over BMS.
22) Reflecting these findings, BMS use continued to decline between 2011 and 2015, while DES implantation was on the rise. DES has become the main strategy for PCI in Korea regardless of clinical presentations.
In the present study, clinical outcomes between 2011 and 2015 did not improve. To enhance clinical outcomes of patients with CAD, appropriate medical treatment is important.
23) Optimal medical therapy (OMT), defined as the combination of at least 1 anti-platelet agent, statin, beta-blocker, and ACEI/ARB, is the suggested initial treatment strategy and recommended for all patients with CAD.
24)25) In the SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) trial, a post hoc analysis demonstrated that the lack of OMT was associated with adverse clinical outcomes of patients with complex CAD requiring coronary revascularization.
24) However, in the current study, the number of patients taking OMT in the angina and AMI groups were 20,731 (42.1%) and 19,249 (60.4%), respectively. Overall, only 39,980 (49.3%) patients were taking OMT. Accordingly, the use of OMT remains suboptimal. In the literature, OMT provided clinical benefits in patients with CAD.
24)25) Therefore, to improve clinical outcomes, OMT should be considered for all patients undergoing PCI unless contraindicated.
Our study had several limitations. First, the present study was based on administrative data from the HIRA in South Korea. Similar to previous studies using administrative databases, our study lacked patient clinical data and test findings. Thus, our findings might be limited by uncertainties in unmeasured confounding variables that may affect the management of patients.
8)26) Second, although we used a database from a quasi-governmental organization, a possibility that these data did not fully reflect patient outcomes still exists. Additionally, we did not specify the cause of death.
This study provides a contemporary overview of PCI procedures performed in Korea. In addition, it provides an important perspective on many healthcare aspects, including trends, characteristics, clinical outcomes, and medical costs. Together with the further researches with nationwide database, we hope that this study encourages the further development of clinical guidelines and implementation of these guidelines into clinical practice to improve cardiovascular outcomes in Korea.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download