Abstract
Background and Objectives
The recently discovered myokine irisin has a proposed role in adipose tissue metabolism. The aim of this study was to evaluate the relationship between serum irisin level and the coronary artery severity in patients with stable coronary artery disease (CAD).
Subjects and Methods
Sixty-three patients who underwent coronary angiography (CA) diagnosed with stable CAD and twenty-six patients with normal coronary artery (NCA) were enrolled in the study. Stable CAD patients were divided into two groups as high synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) score (≥23) and lower SYNTAX score (<23). Serum irisin level measurement was carried out using human irisin colorimetric enzyme-linked immunosorbent assay (ELISA) commercial kit (AG-45A-0046EK-KI01, Adipogen, San Diego, CA, USA) as recommended by the manufacturer's protocol.
Results
The patients with stable CAD with a higher SYNTAX score (score ≥23) had significantly lower serum irisin levels (127.91±55.38 ng/mL), as compared the patients with a low SYNTAX score (score <23) (224.69±92.99 ng/mL) and control group (299.54±123.20 ng/mL). Irisin levels showed significant differences between all groups (p<0.001).
Myokines are a type of cytokines that have autocrine, paracrine and endocrine effects, mostly secreted by skeletal muscle.1) Irisin is a recently reported novel myokine, which is generated by exercise and acts as an insulin-sensitizing hormone.2) Fibronectin type III domain containing protein 5 (FNDC5) is a plasma membrane protein that is proteolytically cleaved to Irisin. Irisin induces the browning of subcutaneous white adipocytes and stimulates thermogenic genes including uncoupling protein 1 (UCP1) both in stromal vascular fraction (SVF) cells and in mouse models.3) Mice injected with adenoviral vectors containing full-length FNDC5 showed a threefold-fourfold increase in plasma irisin levels, which provided to lower weight gain, improvement in glucose tolerance and insulin resistance.3) Human studies have shown that serum irisin levels are associated with other hormones, such as adipokines,4) myokines,5) obesity,6) insulin resistance7) and metabolic syndrome.8) However, the results of reported studies are conflicting. One study reported a positive relationship between body mass index and serum irisin levels, whereas, another study showed a negative relationship.6)9)10) Similar paradoxal association was found in patients with diabetes mellitus.10)11) A cohort study conducted in nondiabetic patients showed that serum irisin levels were positively associated with body weight, body fat mass, fasting, two hours post-load insulin levels and carotid intima-media thickness; depite the negative correlation between serum irisin levels and insulin-stimulated glucose disposal.12) Furthermore, high irisin levels were related with major adverse cardiovascular events in the post-infarct period.
The synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) score is an angiographic score that defines the grade and complexity of coronary artery disease (CAD).13) Numerous studies confirmed that patients with a relatively high SYNTAX score have poor outcomes, and that the score is an independent predictor of major advanced cardiovascular outcomes (MACE) for percutaneous coronary intervention (PCI).14)
In this study, we aimed to investigate the relationship between irisin levels and the severity of coronary artery disease with the SYNTAX score in patients with stable coronary artery disease.
Sixty-three patients who underwent coronary angiography (CA) diagnosed with stable CAD and twenty-six patients with normal coronary artery (NCA) were enrolled in the study from May 2015 to December 2015. Patients with previous coronary artery bypass grafting (CABG) and acute coronary syndrome were excluded from the study. Patients with diabetes mellitus, body mass index >30 kg/m2 (obese patients), active infection, or chronic inflammatory diseases, severe hepatic or renal dysfunction, and malignancy were also excluded. The study was approved by the local ethical committee and all patients provided informed consent.
Coronary angiography was performed using the Judkins technique (Siemens Axiom Artis Zee 2011; Siemens Healthcare, Erlangen, Germany) through the femoral artery or the radial artery. Each coronary artery was displayed in at least two different plane images. According to the baseline CA, the SYNTAX score was calculated in all patients by 2 experienced interventional cardiologists unaware of the clinic and laboratory results of the patients. The SYNTAX score was determined for all coronary lesions with >50% diameter stenosis in a vessel >1.5 mm, based on the SYNTAX score calculator 2.1 (www.syntaxscore.com). Stable CAD patients were divided into two groups as high SYNTAX score (≥23) (30 patients) and lower SYNTAX score (< 23) (33 patients).
To define intra-observer variability, fifteen subjects were selected randomly from the patients. Measurements were repeated under the same basal conditions. Reproducibility of SYNTAX score by CA was assessed by coefficient of variation between measurements. Intra-observer variability was 3.5% for SYNTAX score.
The patients' blood pressure, smoking status, body mass index and medications were recorded. Venous blood samples were obtained from the antecubital vein on admission. All patients underwent laboratory tests using standard methods following an overnight fasting to determine serum creatinine, fasting blood glucose, thyroid stimulating hormone levels (TSH), high sensitivity C-reactive protein (hs CRP) and lipid levels. Baseline, white blood cell count, platelet count and hemoglobin levels were also measured. Insulin resistance Index was calculated using the formula: IRI=(glucose [nmol/L]× insulin [µU/mL]/22.5), using fasting values.15)
Blood samples for irisin measurements were centrifuged immediately and serum samples were stored at -80℃ until the day of analysis. At study enrollment, 10 mL of whole blood was taken using serum separation tube (SST) and ethylenediaminetetraacetic acid (EDTA) tube. Interassay and intraassay coefficients of variation were <8% and <6% for irisin, respectively. Serum irisin measurement was carried out using human irisin colorimetric enzyme-linked immunosorbent assay (ELISA) commercial kit (AG-45A-0046EK-KI01, Adipogen, San Diego, CA, USA) as recommended by the manufacturer's protocol.
The SPSS 18.0 Statistical Package Program for Windows (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Continuous variables were expressed as mean±standard deviation or median with interquartile range, and categorical variables were expressed as percentages and numbers. A χ2 test or Fisher's exact test was used to compare the categorical variables. The normality of distributions of the parameters was assessed by using the Shapiro-Wilk test. Comparison between continuous variables was made by use of independent samples t test for normally distributed variables, and Mann-Whitney U test when the distribution was skewed. Univariate logistic regression analysis was used to evaluate the relationship between variables and SYNTAX score. Variables that were statistically significant in the univariate analysis were further used in a multivariate logistic regression analysis with forward stepwise method, in order to determine the independent predictors of high SYNTAX score and severe CAD. The results of the regression analyses were presented as odd ratios (OR) and 95% confidence intervals (CI). A p value <0.05 was considered statistically significant.
Clinical, demographic and laboratory variables of the groups were shown in Table 1. The patients in the higher SYNTAX group (score ≥23) was older than the lower SYNTAX group (score <23) and control group (62.40±8.05, 60.93±9.58 and 58.42±10.46, respectively; p=0.001). Body mass index, blood pressure (systolic and diastolic), smoking, fasting glucose, hemoglobin, TSH, serum creatinine and serum lipid levels were not statistically significant between groups. Compared with lower SYNTAX group (score <23) patients, higher SYNTAX group (score ≥23) patients had significantly higher serum hs-CRP levels (p<0.001), higher insulin resistance index (p=0.001) and lower left ventricular ejection fraction (p=0.002).
The patients with stable CAD with a higher SYNTAX score (score ≥23) had significantly lower serum irisin levels (127.91±55.38 ng/mL), as compared to patients with a low SYNTAX score (score <23) (224.69±92.99 ng/mL) and control group (299.54±123.20 ng/mL). Irisin levels showed significant differences between all groups (p<0.001). Irisin level showed a significant inverse correlation with SYNTAX score (p<0.001, r=-0.428) (Fig. 1).
The results of the univariate and multivariate logistic regression analyses were listed in Table 2. In the multivariate regression analysis, hs-CRP (p=0.004, OR: 0.229, 95% CI: 0.265-1.348), and lower serum irisin levels (p<0.001, OR: -0.566, 95% CI: -0.072~-0.042) were independent predictors of SYNTAX score in the study subjects after adjusting other confounders.
In the present study, irisin levels were lower in the patients with higher SYNTAX score. Lower irisin levels are an independent predictor of coronary artery disease severity. Our findings highlight the role of irisin not only in metabolic disorders, but also in cardiovascular diseases.
Myokines are novel biomarkers identified in patients with cardiovascular diseases, which are proposed to modulate energy metabolism. Among myokines, myostatin, irisin, leukemia inhibitory factor (LIF) are most well-known. FNDC5 is enzymatically cleaved and secreted as the hormone peptide irisin, as first reported by Bostrom et al.3) As demonsrated in Fig. 2, it enhances metabolic uncoupling and hence caloric expenditure in the situation of exercise or temperature by converting the WAT to brown to brown adipose tissue (BAT).3)16) Heart and skeletal muscle, adipose tissue, liver, kidneys, peripheral nerve sheath, dermis and hypodermis of the skin secrete irisin.17) Reduction in energy level cause decrease the irisin concentration in circulation, and further ischemia in the cardiac tissues.16)
Our study demonstrated that the patient with lower irisin levels had higher insulin resistance index. Irisin is considered a cellular ‘energy sensor’ blocking white adipose tissue to brown adipose tissue, resulting in decreased metabolic thermogenesis. The first studies showed that irisin was associated with increased risk of the metabolic syndrome, cardiometabolic variables, and cardiovascular disease in subjects with a history of myocardial infarction or stroke.8) Positive association was reported between irisin levels and adverse metabolic phenotypes, such as obesity and the metabolic syndrome (MS).9)18) On the other hand, few studies demonstrated an inverse association between circulating irisin levels and obesity or diabetes.18)19)20)
The role of irisin in human physiology remains largely unknown despite recently published studies. High irisin concentration causes a loss of ATP because of its uncoupling properties and decreased irisin level protects energy loss of myocardial cells.3) Cardiac muscle cells produce more irisin than skeletal muscle.3)21) Recently, a link between myocardial infarction and circulated irisin concentration was suggested.16) Aronis et al.22) demonstrated that circulating irisin levels do not predict the development of ACS in healthy individuals, however increased irisin levels prospectively predict the development of MACE in patients with established CAD after PCI. Theirs was the first study to evaluate the relationship between circulating irisin levels and ACS in human subjects, as well as clinical outcomes in patients with established CAD.22) In a study with animal models, Kuloglu et al.16) showed that serum irisin level was gradually decreased in the isoproterenol-induced myocardial infarction.
Parallel to the our study, Park et al.21) showed that irisin is independently associated with the general Framingham risk score profile, demonstrating that patients with lower circulating irisin levels have an increased event-free survival rate 12 months after PCI.8) Emanuele et al.23) demonstrated that healthy centenarians are characterized by increased serum irisin levels, whereas levels of this molecule were significantly lower in young patients with myocardial infarction. On the other hand, their data indicated that circulating irisin levels may be significantly associated with successful aging and could also serve as a potential vascular risk marker.23) As noted above, irisin level was associated with coronary disease severity but the exact mechanism between irisin and coronary artery disease or atherosclerosis is unknown. Although increased irisin level may be the cause or consequence of coronary artery disease, a mouse study by Lu et al.24) showed that irisin might have a preventive role in atherosclerosis; they reported systemic administration of irisin protected against endothelial injury and ameliorated atherosclerosis by inhibition of oxidative stress.24) In the same study, they reported that irisin decreased the plaque area and the infiltrating macrophages and T lymphocytes in the plaques, and down-regulated the mRNA expression of inflammatory cytokines in the aortas.24) According to our results, the mean age was lower in control group. Löffler et al.25) also showed a negative association between age and serum irisin levels. Our results indicated that age was associated with high SYNTAX score in the study group. However, in the regression analyses, only hs-CRP and irisin levels were independent predictors of high SYNTAX score.
Our study had some limitations. First, our study has relatively small sample size of selected patients. Secondly, it is a cross-sectional study. Irisin concentration was only measured at admission and without correction for potential variability in levels. Further large, multicenter follow up studies are needed to confirm this relation.
In conclusion, this is the first study to show that decreased irisin levels predict the severity of stable coronary artery disease and higher SYNTAX score. Future studies are needed to assess whether irisin is associated with cardiometabolic disease, reactively expressed as a protective mechanism, or uninvolved in the pathophysiology of patients with coronary artery disease. Elucidating the correct mechanism would lead to a better understanding of the clinical role of irisin.
Figures and Tables
Fig. 1
Correlation between Irisin level and SYNTAX score. SYNTAX: synergy between percutaneous coronary intervention with taxus and cardiac surgery.
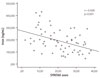
Fig. 2
Irisin synthesis and the principle biochemical effects of irisin. FNDC5: fibronectin type III domain-containing protein 5, UCP-1: uncoupling protein 1.

Table 1
Basic characteristics of the study participants
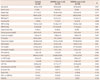
Values are presented as mean±standard deviation or n (%). SYNTAX: synergy between percutaneous coronary intervention with taxus and cardiac surgery, BMI: body mass index, SBP: systolic blood pressure, DBP: diastolic blood pressure, TC: total cholesterol, HDL: high density lipoprotein-cholesterol, LDL: low density lipoprotein-cholesterol, TSH: thyroid stimulating hormone, hs-CRP: high sensitive C-reactive protein, LVEF: left ventricle ejection fraction, ACE-I: angiotensin converting enzyme, ARB: angiotensin 2 receptor blocker, CCB: calcium channel blocker
Table 2
Multivariate linear regression analysis showing independent predictors of the SYNTAX score

References
1. Pedersen BK, Febbraio MA. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat Rev Endocrinol. 2012; 8:457–465.
2. Pedersen BK, Akerstrom TC, Nielsen AR, Fischer CP. Role of myokines in exercise and metabolism. J Appl Physiol (1985). 2007; 103:1093–1098.
3. Bostrom P, Wu J, Jedrychowski MP, et al. A PGC1-alpha-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature. 2012; 481:463–468.
4. Huh JY, Panagiotou G, Mougios V, et al. FNDC5 and irisin in humans: I. Predictors of circulating concentrations in serum and plasma and II. mRNA expression and circulating concentrations in response to weight loss and exercise. Metabolism. 2012; 61:1725–1738.
5. Vamvini MT, Aronis KN, Panagiotou G, et al. Irisin mRNA and circulating levels in relation to other myokines in healthy and morbidly obese humans. Eur J Endocrinol. 2013; 169:829–834.
6. Moreno-Navarrete JM, Ortega F, Serrano M, et al. Irisin is expressed and produced by human muscle and adipose tissue in association with obesity and insulin resistance. J Clin Endocrinol Metab. 2013; 98:E769–E778.
7. Crujeiras AB, Pardo M, Arturo RR, et al. Longitudinal variation of circulating irisin after an energy restriction-induced weight loss and following weight regain in obese men and women. Am J Hum Biol. 2014; 26:198–207.
8. Park KH, Zaichenko L, Brinkoetter M, et al. Circulating irisin in relation to insulin resistance and the metabolic syndrome. J Clin Endocrinol Metab. 2013; 98:4899–4907.
9. Stengel A, Hofmann T, Goebel-Stengel M, Elbelt U, Kobelt P, Klapp BF. Circulating levels of irisin in patients with anorexia nervosa and different stages of obesity--correlation with body mass index. Peptides. 2013; 39:125–130.
10. Liu JJ, Liu S, Wong MD, et al. Relationship between circulating irisin, renal function and body composition in type 2 diabetes. J Diabetes Complications. 2014; 28:208–213.
11. Choi YK, Kim MK, Bae KH, et al. Serum irisin levels in new-onset type 2 diabetes. Diabetes Res Clin Pract. 2013; 100:96–101.
12. Sesti G, Andreozzi F, Fiorentino TV, et al. High circulating irisin levels are associated with insulin resistance and vascular atherosclerosis in a cohort of nondiabetic adult subjects. Acta Diabetol. 2014; 51:705–713.
13. Farooq V, Vergouwe Y, Raber L, et al. Combined anatomical and clinical factors for the long-term risk stratification of patients undergoing percutaneous coronary intervention: the Logistic Clinical SYNTAX score. Eur Heart J. 2012; 33:3098–3104.
14. Garg S, Sarno G, Serruys PW, et al. Prediction of 1-year clinical outcomes using the SYNTAX score in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: a substudy of the STRATEGY (Single High-Dose Bolus Tirofiban and Sirolimus-Eluting Stent Versus Abciximab and Bare-Metal Stent in Acute Myocardial Infarction) and MULTISTRATEGY (Multicenter Evaluation of Single High-Dose Bolus Tirofiban Versus Abciximab With Sirolimus-Eluting Stent or Bare-Metal Stent in Acute Myocardial Infarction Study) trials. JACC Cardiovasc Interv. 2011; 4:66–75.
15. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–419.
16. Kuloglu T, Aydin S, Eren MN, et al. Irisin: a potentially candidate marker for myocardial infarction. Peptides. 2014; 55:85–91.
17. Aydin S, Aydin S, Kuloglu T, et al. Alterations of irisin concentrations in saliva and serum of obese and normal-weight subjects, before and after 45 min of a Turkish bath or running. Peptides. 2013; 50:13–18.
18. Liu JJ, Wong MD, Toy WC, et al. Lower circulating irisin is associated with type 2 diabetes mellitus. J Diabetes Complications. 2013; 27:365–369.
19. Polyzos SA, Kountouras J, Anastasilakis AD, Margouta A, Mantzoros CS. Association between circulating irisin and homocysteine in patients with nonalcoholic fatty liver disease. Endocrine. 2015; 49:560–562.
20. Moreno M, Moreno-Navarrete JM, Serrano M, et al. Circulating irisin levels are positively associated with metabolic risk factors in sedentary subjects. PLoS One. 2015; 10:e0124100.
21. Park SE, Park CY, Sweeney G. Biomarkers of insulin sensitivity and insulin resistance: Past, present and future. Crit Rev Clin Lab Sci. 2015; 52:180–190.
22. Aronis KN, Moreno M, Polyzos SA, et al. Circulating irisin levels and coronary heart disease: association with future acute coronary syndrome and major adverse cardiovascular events. Int J Obes (Lond). 2015; 39:156–161.
23. Emanuele E, Minoretti P, Pareja-Galeano H, Sanchis-Gomar F, Garatachea N, Lucia A. Serum irisin levels, precocious myocardial infarction, and healthy exceptional longevity. Am J Med. 2014; 127:888–890.
24. Lu J, Xiang G, Liu M, Mei W, Xiang L, Dong J. Irisin protects against endothelial injury and ameliorates atherosclerosis in apolipoprotein E-Null diabetic mice. Atherosclerosis. 2015; 243:438–448.
25. Löffler D, Müller U, Scheuermann K, et al. Serum irisin levels are regulated by acute strenuous exercise. J Clin Endocrinol Metab. 2015; 100:1289–1299.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download