Abstract
Background and Objectives
The etiopathogenesis of coronary artery ectasia (CAE) is not known completely. In most of the cases, CAE is associated with atherosclerosis; however, isolated CAE has a nonatherosclerotic mechanism. The association between atherosclerotic coronary artery disease and apelin has been examined in previous studies. However, the role of plasma apelin in isolated coronary artery ectasia has not been studied. In this study, we investigated the relationship between plasma apelin levels and isolated coronary artery ectasia.
Subjects and Methods
The study population included a total of 54 patients. Twenty-six patients had isolated CAE (53.6±8.1 years); 28 patients with normal coronary arteries (51.6±8.8 years) and with similar risk factors and demographic characteristics served as the control group. Apelin levels were measured using an enzyme-linked immunoassay kit.
Results
Apelin level in the CAE group was significantly lower (apelin=0.181±0.159 ng/mL) than that in the control group (apelin=0.646±0.578 ng/mL) (p=0.033). Glucose, creatinine, total cholesterol, triglyceride, low density lipoprotein cholesterol, and high density lipoprotein cholesterol levels were not significantly different between the two groups.
Apelin is an adipocytokine and a endogenous ligand for the angiotensin-like 1 receptor (APJ). The function of apelin in the cardiovascular system is not clear. Increased apelin expression has been found in coronary vessels, cardiomyocytes, large conduit vessels,1) vascular smooth muscle cells, and endothelial cells.2) Apelin plays an opposite role to the renin-angiotensin-aldosterone system. Apelin has been found to be reduced in patients with heart failure.3) Some functions of apelin such as positive inotropism,4) endothelium-dependent vasodilation,5) cardiac contractility,6) and reduction of vascular wall inflammation7) have been described.
Coronary artery ectasia (CAE) has been defined as abnormal dilatation of a segment of the coronary artery that is 1.5 times larger than the diameter of an adjacent normal segment of artery.8) The incidence of CAE has been reported to be 0.3% to 4.9% in patients who have undergone coronary angiography.9) It has been demonstrated that CAE could predispose to adverse coronary events such as vasospasm, thrombosis, dissection, and even myocardial infarction.10) Although the exact mechanism leading to CAE is not clear to date, atherothrombosis, endothelial dysfunction, and vasculitis have been suggested as possible responsible factors.11) The relation between CAE and chronic vascular inflammation is known. We believe that apelin protects vessels from ectasia by decreasing vessel wall inflammation. According to the data, we suggested a possible relationship between apelin and isolated CAE. In this study, we aimed to examine the relation between serum apelin level and isolated CAE.
Study population included a total of 54 patients who were admitted to the Cardiology Department. Twenty-six patients with isolated CAE (53.6±8.1 years) were categorized into the CAE group, and 28 patients with normal coronary arteries proven by angiography (51.6±8.8 years) and with similar risk factors and demographic characteristics as the CAE group served as the control group. Patients with malignancy, heart failure, acute coronary syndrome, renal disease, collagen tissue diseases, vasculitis, and coronary artery disease were excluded from the study. All patients underwent a detailed physical examination. Body mass index was calculated as weight divided by height in meters squared. Clinical laboratory analyses were performed in a biochemical laboratory. Biochemical tests were performed by an Abbott Architect C16000 auto-analyzer (Architect C16000 auto-analyzer Abbott Laboratory, Abbott Park, IL, USA) with original kits and hematological counts were measured by an automated hematology analyzer (Abbott Cell-Dyn 3700; Abbott Laboratory, Abbott Park, IL, USA) in peripheral venous blood samples. Standard methods were used to measure total and high density lipoprotein cholesterol (HDL-C), triglycerides, and fasting glucose. Serum obtained by centrifugation was stored at -80℃ until analysis for apelin measurement. Apelin levels were measured using an enzyme-linked immunoassay kit (Phoenix Pharmaceuticals, Inc., CA, USA) according to the manufacturer's instructions, and expressed as ng/ml. Minimal detectable limit of apelin was 0.07 ng/mL.
Coronary angiography was routinely performed using the Allura Xper FD10 (Philips, Amsterdam, Netherlands) through the femoral artery by the Judkin's technique without the use of nitroglycerin. The contrast agent used was Iopamiro 370 (Bracco, Milan, Italy) in all patients. Each angiogram was evaluated concurrently by two interventional cardiologists who were blinded to the study and to each other. Angiographically, CAE was diagnosed when the diameter of a dilated segment of the coronary artery was 1.5 times larger than that of an adjacent normal segment.8) The study was approved by the Local Ethics Committee and informed consent was obtained from each patient.
Data were analyzed with Statistical Package for the Social Sciences (SPSS) software version 18.0 for Windows (SPSS Inc., Chicago, IL, USA). The Kolmogorov-Smirnov test was used to verify that continuous variables were normally distributed. Continuous variables are expressed as mean±standard deviation, and categorical variables are expressed as percentages. The independent sample t-test or Mann-Whitney U test was used for continuous variables and the chi-square test was used for categorical variables. Statistical significance was defined as p<0.05.
The study included a total of 54 patients. The CAE group included 26 patients with isolated coronary artery ectasia (mean age 53.6±8.1 years), with 73.1% (n=19) of these patients being males. The control group included 28 patients with normal coronary arteries (mean age 51.6±8.8 years), with 64.3% (n=18) of these patients being males. There was no difference between the two groups in terms of basal demographic data (p>0.05). Demographic characteristics of the groups are presented in Table 1. We found that the apelin level in the CAE group was significantly lower (apelin=0.181±0.159 ng/mL) than that in the control group (apelin=0.646±0.578 ng/mL) (p=0.033) (Fig. 1). Glucose, creatinine, total cholesterol, triglyceride, low density lipoprotein cholesterol (LDL-C), and HDL-C levels were not significantly different between the two groups (p>0.05).
The main finding of the present study is that patients with isolated CAE had significantly lower plasma apelin levels compared with patients with angiographically normal coronary arteries. To the best of our knowledge, this is the first study in the literature that has investigated the relation between apelin and isolated CAE. CAE has been defined as an abnormal dilatation of a coronary artery that is 1.5 times larger than the diameter of adjacent normal segments.8) The etiology of CAE is not completely understood. In approximately half of the cases, CAE occurs due to atherosclerosis. In a minority of cases, CAE is observed in the absence of a significant atherosclerotic lesion. The intima is intact, but extensive media degeneration and hyalinization, possibly as a result of chronic vascular inflammation, are commonly seen in all cases of CAE.11) Another mechanism of CAE is proteolysis of the extracellular matrix proteins by metalloproteinases.12) Overexpression of matrix metalloproteinases (MMPs), especially MMP-3 leads to enhanced vessel wall degradation of various matrix proteins, such as proteoglycans, laminin, fibronectin, and collagen types III, IV, V, and IX; thus MMPs may lead to excessive vessel wall dilatation.13) In addition, another mechanism of CAE is the inflammatory vascular hypothesis. According to this hypothesis, the presence of CAE is related to elevated plasma levels of high sensitivity C-reactive protein (hsCRP),14) interleukin-6 (Il-6),15) intercellular adhesion molecule, vascular cell adhesion molecule, and E-selectin. This hypothesis suggests the presence of extensive chronic inflammation in patients with CAE.16)
The cardiovascular system is the main target of apelin and its receptor APJ. Apelin has an important role in cardiovascular homeostasis. Positive inotropism, vasodilation, decreased blood pressure,17) and reduction of vascular wall inflammation,7) are some of the effects of apelin on the cardiovascular system. It is difficult to suggest a standard normal level of apelin. Various apelin levels have been demonstrated in different studies. Ellinor et al.18) reported a mean apelin level of 304 pg/mL in the normal population. Li et al.19) reported an apelin level of 1.98 ng/mL in the healthy group. Kadoglou et al.20) reported that the apelin level in the healthy control group was 2.99±1.52 ng/mL. We found that the mean apelin level in the control group was 0.646±0.578 ng/mL. The relationship between CAE and apelin is not clear. Recent studies17)21)22) have shown some cardioprotective effects of apelin on the cardiovascular system. The possible role of apelin in the pathophysiology of CAE is summarized in Fig. 2. Japp et al.17) demonstrated that apelin is a direct coronary vasodilator that increases myocardial contractility in humans via nitric oxide-dependent mechanisms and causes a reduction in left ventricular end-diastolic pressures. In another study,3) it has been suggested that the apelin/APJ pathway is a regulator of cardiovascular function. Apelin has been shown to have a positive effect on contractility, and experiments using myocardial injury rat models have suggested that apelin also has a positive inotropic effect on failing myocardium.21) Simpkin et al.22) reported that apelin has a cardioprotective effect against reperfusion injury. In an in vivo and in vitro rodent model of myocardial ischemia/reperfusion, apelin was administered at reperfusion. Reduction in the infarct size was demonstrated in both experiments.
Loss of musculoelastic components of the vessel media plays an important role in the pathogenesis of CAE. Attenuation of the vessel wall has been shown in nonatherosclerotic forms of CAE by Rath et al.11) The cause of attenuation was degeneration of media of the vessel wall and hyalinized collagen that replaced the smooth muscle.11) Li et al.23) reported that apelin may have a regulatory effect on proliferation of vascular smooth muscle cells and nitric oxide production. Recent studies7)24)25) suggest a role of apelin in inflammation. Apelin expression in adipose tissue of mice has been shown to be up-regulated by tumor necrosis factor-α (TNF-α).24) In another study,25) apelin was negatively correlated with inflammatory markers (hsCRP and IL-6) in patients with CAE. It has been suggested that the apelin pathway may provide a mechanism for systemic inflammatory monitoring and adaptive regulation of cardiovascular function.25) Leeper et al.7) reported that apelin infusion was associated with significantly reduced aortic IL-6 and TNF-α messenger-RNA levels. They suggested that apelin prevents aortic aneurysm formation by inhibiting macrophage proinflammatory cytokines.7) C-reactive protein (CRP) levels have been reported to be associated with coronary events.26) Also, the relationship between inflammation and CAE has been reported in some studies. Turhan et al.16) reported that CRP levels were significantly higher in patients with isolated CAE compared to patients with coronary artery disease and subjects with angiographically normal coronary arteries. Another marker of inflammation is the neutrophil to lymphocyte ratio. Ayhan et al.27) reported that the neutrophil to lymphocyte ratio was higher in patients with CAE compared to subjects with normal coronary arteries. Additionally, Sincer et al.28) reported that serum levels of hsCRP in the CAE group were higher than those in controls. Apelin and other adipocytokines are associated with inflammation and its clinical consequences.29) Apelin is a member of the adipocytokine family like adiponectin. Dagli et al.30) reported that there was a negative correlation between ectatic coronary artery diameter and plasma adiponectin level. In this study, we reported that the plasma apelin level in patients with isolated CAE was significantly lower than that in controls. Therefore, we believe that apelin might be associated with CAE. Based on the recent data, we suggest that apelin has cardioprotective effects and it may protect the vessels from ectasia by decreasing vessel wall inflammation.
One of the limitations of the study is that intravascular ultrasound (IVUS) was not performed in patients for establishing the diagnosis. IVUS may be useful for identifying the atherosclerotic plaques that cannot be seen by coronary angiography. Another limitation of the study was that a small patient population was included. Larger studies are required to verify the relationship between apelin and CAE.
Figures and Tables
Fig. 1
Comparison of apelin levels between the CAE and control groups. In the CAE group, the mean apelin level is significantly lower (p=0.033). CAE: coronary artery ectasia.

Fig. 2
The pathophysiological role of apelin in coronary artery ectasia. Apelin is associated with reduced interleukin-6 (IL-6) and Tumor necrosis factor-α (TNF-α) levels. It has been suggested that apelin inhibits macrophage proinflammatory cytokines.

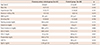
Table 1
Baseline clinical characteristics of the study population
Acknowledgements
We are grateful to Dicle University DUBAP for their sponsorship about English editing of this manuscript.
References
1. Kleinz MJ, Davenport AP. Emerging roles of apelin in biology and medicine. Pharmacol Ther. 2005; 107:198–211.
2. Ronkainen VP, Ronkainen JJ, Hänninen SL, et al. Hypoxia inducible factor regulates the cardiac expression and secretion of apelin. FASEB J. 2007; 21:1821–1830.
3. Chandrasekaran B, Dar O, McDonagh T. The role of apelin in cardiovascular function and heart failure. Eur J Heart Fail. 2008; 10:725–732.
4. Hashimoto T, Kihara M, Ishida J, et al. Apelin stimulates myosin light chain phosphorylation in vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 2006; 26:1267–1272.
5. Tatemoto K, Takayama K, Zou MX, et al. The novel peptide apelin lowers blood pressure via a nitric oxide-dependent mechanism. Regul Pept. 2001; 99:87–92.
6. Farkasfalvi K, Stagg MA, Coppen SR, et al. Direct effects of apelin on cardiomyocyte contractility and electrophysiology. Biochem Biophys Res Commun. 2007; 357:889–895.
7. Leeper NJ, Tedesco MM, Kojima Y, et al. Apelin prevents aortic aneurysm formation by inhibiting macrophage inflammation. Am J Physiol Heart Circ Physiol. 2009; 296:H1329–H1335.
8. Hartnell GG, Parnell BM, Pridie RB. Coronary artery ectasia. Its prevalence and clinical significance in 4993 patients. Br Heart J. 1985; 54:392–395.
9. Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990; 21:28–40.
10. Valente S, Lazzeri C, Giglioli C, et al. Clinical expression of coronary artery ectasia. J Cardiovasc Med (Hagerstown). 2007; 8:815–820.
11. Rath S, Har-Zahav Y, Battler A, et al. Fate of nonobstructive aneurysmatic coronary artery disease: angiographic and clinical follow-up report. Am Heart J. 1985; 109:785–791.
12. Lamblin N, Bauters C, Hermant X, Lablanche JM, Helbecque N, Amouyel P. Polymorphisms in the promoter regions of MMP-2, MMP-3, MMP-9 and MMP-12 genes as determinants of aneurysmal coronary artery disease. J Am Coll Cardiol. 2002; 40:43–48.
13. Finkelstein A, Michowitz Y, Abashidze A, Miller H, Keren G, George J. Temporal association between circulating proteolytic, inflammatory and neurohormonal markers in patients with coronary ectasia. Atherosclerosis. 2005; 179:353–359.
14. Turhan H, Erbay AR, Yasar AS, Balci M, Bicer A, Yetkin E. Comparison of C-reactive protein levels in patients with coronary artery ectasia versus patients with obstructive coronary artery disease. Am J Cardiol. 2004; 94:1303–1306.
15. Tokgozoglu L, Ergene O, Kinay O, Nazli C, Hascelik G, Hoscan Y. Plasma interleukin-6 levels are increased in coronary artery ectasia. Acta Cardiol. 2004; 59:515–519.
16. Turhan H, Erbay AR, Yasar AS, et al. Plasma soluble adhesion molecules; intercellular adhesion molecule-1, vascular cell adhesion molecule-1 and E-selectin levels in patients with isolated coronary artery ectasia. Coron Artery Dis. 2005; 16:45–50.
17. Japp AG, Cruden NL, Amer DA, et al. Vascular effects of apelin in vivo in man. J Am Coll Cardiol. 2008; 52:908–913.
18. Ellinor PT, Low AF, Macrae CA. Reduced apelin levels in lone atrial fibrillation. Eur Heart J. 2006; 27:222–226.
19. Li Z, Bai Y, Hu J. Reduced apelin levels in stable angina. Intern Med. 2008; 47:1951–1955.
20. Kadoglou NP, Lampropoulos S, Kapelouzou A, et al. Serum levels of apelin and ghrelin in patients with acute coronary syndromes and established coronary artery disease--KOZANI STUDY. Transl Res. 2010; 155:238–246.
21. Ashley EA, Powers J, Chen M, et al. The endogenous peptide apelin potently improves cardiac contractility and reduces cardiac loading in vivo. Cardiovasc Res. 2005; 65:73–82.
22. Simpkin JC, Yellon DM, Davidson SM, Lim SY, Wynne AM, Smith CC. Apelin-13 and apelin-36 exhibit direct cardioprotective activity against ischemia-reperfusion injury. Basic Res Cardiol. 2007; 102:518–528.
23. Li L, Li L, Xie F, et al. Jagged-1/Notch3 signaling transduction pathway is involved in apelin-13-induced vascular smooth muscle cells proliferation. Acta Biochim Biophys Sin (Shanghai). 2013; 45:875–881.
24. Daviaud D, Boucher J, Gesta S, et al. TNFalpha up-regulates apelin expression in human and mouse adipose tissue. FASEB J. 2006; 20:1528–1530.
25. El-Shehaby AM, El-Khatib MM, Battah AA, Roshdy AR. Apelin: a potential link between inflammation and cardiovascular disease in end stage renal disease patients. Scand J Clin Lab Invest. 2010; 70:421–427.
26. Arroyo-Espliguero R, Avanzas P, Cosín-Sales J, Aldama G, Pizzi C, Kaski JC. C-reactive protein elevation and disease activity in patients with coronary artery disease. Eur Heart J. 2004; 25:401–408.
27. Ayhan SS, Oztürk S, Erdem A, et al. Relation of neutrophil/lymphocyte ratio with the presence and severity of coronary artery ectasia. Turk Kardiyol Dern Ars. 2013; 41:185–190.
28. Sincer I, Aktürk E, Açikgöz N, Ermiş N, Koşar MF. Evaluation of the relationship between serum high sensitive C-reactive protein and the elasticity properties of the aorta in patients with coronary artery ectasia. Anadolu Kardiyol Derg. 2011; 11:414–420.
29. Malyszko J, Malyszko JS, Pawlak K, Wolczynski S, Mysliwiec M. Apelin, a novel adipocytokine, in relation to endothelial function and inflammation in kidney allograft recipients. Transplant Proc. 2008; 40:3466–3469.
30. Dagli N, Ozturk U, Karaca I, et al. Adiponectin levels in coronary artery ectasia. Heart Vessels. 2009; 24:84–89.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download