Abstract
Purpose
This study aimed to investigate the prevalence of nocturia according to the International Continence Society (ICS) definition in Turkish women and to determine the associated risk factors and the correlation of other voiding symptoms with nocturia.
Materials and Methods
A prospective epidemiological study was carried out by use of self-reported questionnaires in 4,250 reproductive-aged women from January 2013 to May 2013. The International Consultation on Incontinence Questionnaire-Short Form and a questionnaire developed by the researchers according to the ICS were administered to define nocturia and other lower urinary tract symptoms. Other physical, reproductive, and health characteristics were also recorded concurrently.
Results
Overall, 1,636 women were included in the final analyses. The women had an average age of 34.4±5.26 years. The overall prevalence of nocturia was 34.7% (567 of 1,636 women). Women with nocturia were older (p<0.001), had a higher body mass index (p=0.026), and had more children (p<0.001). Nocturia occurred more frequently in women with a history of nocturnal enuresis (p<0.001). Three or more pregnancies, 3 or more deliveries, and age >40 years were significant risk factors for nocturia. We also found that other lower urinary tract symptoms correlated significantly (p<0.001) with nocturia.
Conclusions
Although the prevalence of nocturia is higher with increasing age, younger adults are also affected. Nocturia may cause sleep disorders, mood disturbances, reduced quality of life, and distractibility. Thus, even if one void nightly causes a patient to experience bother, nocturia should be queried about and should be treated if necessary according to the cause of the disease.
Whereas nocturia was previously viewed as only a part of lower urinary tract symptoms (LUTS), recently, nocturia has been evaluated as a specific symptom and has been studied by researchers on the basis of its etiology and consequences. Furthermore, nocturia has become a common urologic problem rather than just a clinical symptom that affects quality of life. Although some definitions have been described before, the International Continence Society (ICS) offered the first standardization of nocturia terminology in 2002. According to the ICS, nocturia is defined as the complaint of needing to wake at night one or more times to void [1,2].
Prevalence estimates vary owing to methodological differences, the age range considered, and the definition of nocturia used. Additionally, overall rates of nocturia prevalence may have been misleading in some previous studies because the age distribution of the sample was not equal. The estimated prevalence of nocturia varies from approximately 20% to 44% due to one or more voids in younger women [2].
The first aim of this article was to investigate the prevalence of nocturia according to the ICS definition in reproductive-aged Turkish women in order to emphasize the prevalence of nocturia in younger women. Limited information is available on this age group in the literature. The second aim was to determine the risk factors associated with nocturia. The researchers also analyzed the correlation of other voiding symptoms with nocturia.
With Institutional Review Board approval, a cross-sectional, epidemiological study was carried out in reproductive-aged women from January 2013 to May 2013 in Ankara, the capital and second largest city of Turkey. A questionnaire developed by researchers and the International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF) were distributed to the mothers of 4,250 primary school children. The participants completed the forms at their homes. Three days later, the questionnaires were collected from the schools. Data were collected by self-administered questionnaire. The study consisted of 10 randomly selected primary schools in Ankara.
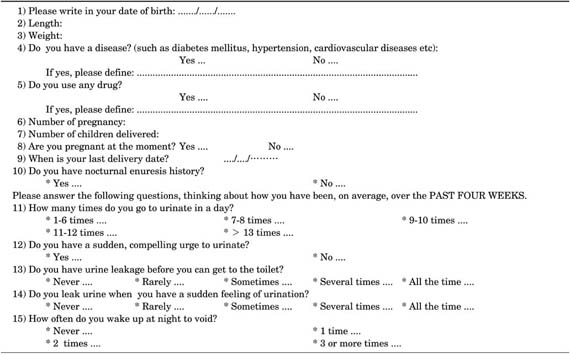
The questionnaire consisted of essentially two parts. In the first part, the researchers collected information from the Turkish validated form of the ICIQ-SF questionnaire [3]. The second part of the study was prepared to analyze the physical, reproductive, and health characteristics; history of nocturnal enuresis (NE); and urinary characteristics of the women (Appendix). The questions regarding the urinary features of the participants were quoted from the Bristol Female Lower Urinary Tract Symptom Index, which was validated by Gokkaya et al. [4]. Furthermore, the researchers performed a pilot study with a developed questionnaire in a relevant group. Frequency was defined as more than seven voids per day, urgency was defined as the complaint of a sudden desire to pass urine, and nocturia was defined on the basis of the ICS definition as mentioned above [1]. Urge urinary incontinence was determined as a result of the ICIQ-SF questionnaire [5]. Probable overactive bladder was presumed on the basis of the subjects' answers to the questionnaire.
Participants who did not fully complete the questionnaire (n=304), had entered menopause (n=11), were pregnant or had given birth during the previous 3 months (n=12), or had a self-reported comorbidity, such as cardiovascular diseases (n=3), diabetes mellitus (n=9), or hypertension or had used antihypertension drugs or diuretics (n=7), were excluded from the study.
Results were reported as the mean±standard deviation or as frequencies and percentages. Statistical analysis of the clinical data between the two groups consisted of Student t-tests for parametric data and Mann-Whitney U-test analysis for nonparametric data. In addition, Fisher exact and chi-square tests were used to compare categorical data. The significant precipitating factors for nocturia were reported with their prevalence and odd ratios. Additionally, logistic regression analysis was performed to examine the independent effect of each variable on nocturia. Statistical analysis was performed by using PASW Statistics 18.0 (SPSS Inc., Chicago, IL, USA), and the level of significance was established at the 0.05 level (2-sided).
A total of 4,250 questionnaires were distributed. Of those, 1,982 questionnaires (46.6%) were completed, and 1,636 (38.5%) reproductive-aged women were included in the final analyses.
The women in the sample had an average age of 34.4±5.26 years (range, 20-46 years). Women with nocturia were older (35.09±5.58 years vs. 34.03±5.05 years, p=0.0001), had a higher body mass index (BMI) (25.62±4.15 kg/m2 vs. 25.24±4.26 kg/m2, p=0.026), and had more children (2.33±0.87 vs. 2.11±0.74, p=0.0001) (Table 1).
The overall prevalence of nocturia was 34.7% (567 of 1,636 women). When nocturia was defined as two or more voidings per night, the prevalence of nocturia was 12.8% (210 of 1,636 women). The prevalence of nocturia increased with age, BMI, number of pregnancies, and number of children delivered. More than three pregnancies, more than three deliveries, and age>40 years were significant risk factors for nocturia. The distribution of nocturia prevalence according to age, BMI, number of pregnancies, and number of children delivered is shown in Table 2.
One hundred twenty-eight women had a history of NE enuresis, and nocturia occurred more frequently in women with a history of NE (p=0.0001). The researchers also found that other LUTS correlated significantly (p<0.001) with nocturia, and 76.2% of women with overactive bladder reported nocturia (Table 3).
Women with nocturia were older and had a greater number of pregnancies than did women without nocturia. Nocturia also occurred more frequently in women with a history of NE. However, BMI and number of children delivered were not significant risk factors for the presence of nocturia in women (Table 4).
To the best of our knowledge, this is the first population-based prevalence study using the 2002 ICS definitions that analyzed nocturia prevalence and associated risk factors among Turkish women. Although the estimated prevalence of nocturia varies markedly from study to study, nocturia is one of the most common symptoms in women. According to the current study, the prevalence rate of nocturia was 34.7% in reproductive-aged women.
The prevalence rate in the present study may seem lower than the rate in the literature because of the difference in age groups. For example, a Dutch population study, which included participants aged ≥18 years old, showed that 54% of women voided once or more at night [6]. Data from 1,247 women from Austria demonstrated that 55% of the women had nocturia [7]. Similarly, a population-based study of 1,134 women (aged 20-95 years) from Singapore showed that the prevalence rate of nocturia was 58% [8]. In the aforementioned studies, the researchers obtained prevalence rates when nocturia was defined as voiding at least once nightly. However, in contrast with the current study, all age groups were included in these studies.
The rate in the present study may seem to be higher than the rate in the literature because of differences in the definition used. Despite the definition of ICS, some other previous studies were performed that defined nocturia as two or more voids per night. In these studies, the prevalence of nocturia varied from approximately 10% to 30% [7,9,10].
The present study demonstrated that the prevalence of nocturia increased with age. This finding was supported by the literature [6,7,8,9,10]. Several mechanisms may contribute to the increase in nocturia with aging. Due to the age-related changes, nocturnal polyuria, which is an overproduction of urine at night without an increase in the normal 24-hour urination, may be considered to be one of the causes of nocturia [1]. Secondly, Kim et al. [11] reported that decreased nocturnal bladder capacity is another cause of female nocturia. Moreover, they indicated that nocturnal polyuria is the major cause of nocturia in aged women.
The current study confirmed the association between nocturia and BMI. Although nocturia occurred more frequently in women with higher BMI, BMI was not a significant risk factor for the presence of nocturia in women. Nocturia occurred more frequently in women with higher BMI. Hsieh et al. [12] demonstrated that the prevalence of nocturia increased significantly with BMI. Additionally, in the BACH Survey, nocturia was associated with increasing BMI [10]. Recently, results from the FINNO study, which investigated the impact of obesity on urinary storage symptoms, showed that obesity was associated with nocturia in women [13]. However, data of 1,005 women from Korea showed that BMI was not associated with an increased likelihood of nocturia in women [14].
The researchers of the current study found that the prevalence of nocturia increased with the number of pregnancies and the number of children delivered. The number of pregnancies was a significant risk factor for the presence of nocturia in women. Choo et al. [14] reported that the likelihood of at least one nighttime void was related to the number of deliveries. Tikkinen et al demonstrated that parity was associated with an increased risk of nocturia [15]. Furthermore, a study performed in Chinese women reported that parity >2 was a risk factor for nocturia as well as other storage symptoms [16].
Another result of the present study was that nocturia occurred more frequently in women with a history of NE. Until now, few studies have been performed on the association between enuresis and nocturia. Some prior studies demonstrated the link between childhood urinary symptoms and adult overactive bladder symptoms [17,18]. In particular, Fitzgerald et al. [19] indicated that childhood urinary symptoms were independently associated with adult LUTS, and frequent nocturia in childhood was strongly associated with adult nocturia. Although the study was performed on a small number of subjects, the relationship between childhood NE and adult nocturia was first demonstrated by Montaldo et al. [20]. In their study, 64% of women were affected by enuresis in childhood. The current study with a larger number of subjects confirmed this finding. In contrast, Yazici et al. [21] found that there was no relation between young adulthood nocturia and childhood NE, but they found that as the nocturia frequency increased, the rate of childhood NE also increased. As a result, the researchers proposed that childhood NE could be evaluated as a risk factor for adult nocturia. Additionally, the researchers suggested that the early treatment of NE might affect the development of nocturia. This issue should be investigated in further prospective studies. The present study also determined that 76.2% of women with overactive bladder reported nocturia, which was a natural situation as a result of the ICS definition [1].
Four major pathophysiologic mechanisms of nocturia have been defined: 24-hour polyuria, nocturnal polyuria, reduced bladder capacity, and sleep disorders [22]. It is also suggested that aging and a higher number of pregnancies or births could cause a decrease in functional bladder capacity. These factors also induce urogenital prolapse, which causes a reduction in the anatomic and functional capacity of the bladder. The increasing prevalence of overactive bladder and voiding dysfunctions with age also causes nocturia. Additionally, we suggest that bladder aging could be considered a reason for nocturia.
The current study was strengthened by the number of subjects and by the use of the ICS definitions. Although without clinical verification, comorbid conditions and medications that could impact bladder function were excluded from the study on the basis of participant reports. This exclusion benefited the study's ability to determine risk factors. Moreover, as was mentioned earlier, this was the first population-based study from Turkey. However, this study had some limitations. First, epidemiologic studies are generally based on self-reports and methodological differences and differentiation of the definition have significant impacts on the results. Second, the data were collected and evaluated according to the description of the women; thus, socioeconomic and educational differences were not evaluated in this survey. Third, the researchers did not analyze the effect of nocturia on quality of life. Additionally, only reproductive-aged women were included in the study. Finally, the subjects were all Turkish natives, and thus, racial and cultural differences might have affected the results.
Although the prevalence of nocturia was higher with increasing age, younger adults were also affected. As consequences of nocturia, sleep disorders, mood disturbances, reduced quality of life, and distractibility could be seen in young adults. Therefore, nocturia should be queried about and should be treated if necessary.
Figures and Tables
References
1. van Kerrebroeck P, Abrams P, Chaikin D, Donovan J, Fonda D, Jackson S, et al. The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:179–183.
2. Bosch JL, Weiss JP. The prevalence and causes of nocturia. J Urol. 2013; 189:1 Suppl. S86–S92.
3. Cetinel B, Ozkan B, Can G. The validation study of ICIQ-SF Turkish version. Turk J Urol. 2004; 30:332–338.
4. Gokkaya CS, Oztekin CV, Doluoglu OG, Guzel O, Ersahin V, Ozden C, et al. Validation of Turkish version of bristol female lower urinary tract symptom Index. J Clin Anal Med. 2012; 3:415–418.
5. Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004; 23:322–330.
6. van Dijk L, Kooij DG, Schellevis FG. Nocturia in the Dutch adult population. BJU Int. 2002; 90:644–648.
7. Schatzl G, Temml C, Schmidbauer J, Dolezal B, Haidinger G, Madersbacher S. Cross-sectional study of nocturia in both sexes: analysis of a voluntary health screening project. Urology. 2000; 56:71–75.
8. Liew LC, Tiong HY, Wong ML, Png DC, Tan JK. A population study of nocturia in Singapore. BJU Int. 2006; 97:109–112.
9. Yoshimura K, Terada N, Matsui Y, Terai A, Kinukawa N, Arai Y. Prevalence of and risk factors for nocturia: Analysis of a health screening program. Int J Urol. 2004; 11:282–287.
10. Fitzgerald MP, Litman HJ, Link CL, McKinlay JB. BACH Survey Investigators. The association of nocturia with cardiac disease, diabetes, body mass index, age and diuretic use: results from the BACH survey. J Urol. 2007; 177:1385–1389.
11. Kim SO, Kim JS, Kim HS, Hwang EC, Oh KJ, Kwon D, et al. Age related change of nocturia in women. Int Neurourol J. 2010; 14:245–249.
12. Hsieh CH, Chen HY, Hsu CS, Chang ST, Chiang CD. Risk factors for nocturia in Taiwanese women aged 20-59 years. Taiwan J Obstet Gynecol. 2007; 46:166–170.
13. Vaughan CP, Auvinen A, Cartwright R, Johnson TM 2nd, Tahtinen RM, Ala-Lipasti MA, et al. Impact of obesity on urinary storage symptoms: results from the FINNO study. J Urol. 2013; 189:1377–1382.
14. Choo MS, Ku JH, Park CH, Lee YS, Lee KS, Lee JG, et al. Prevalence of nocturia in a Korean population aged 40 to 89 years. Neurourol Urodyn. 2008; 27:60–64.
15. Tikkinen KA, Auvinen A, Tiitinen A, Valpas A, Johnson TM 2nd, Tammela TL. Reproductive factors associated with nocturia and urinary urgency in women: a population-based study in Finland. Am J Obstet Gynecol. 2008; 199:153.
16. Zhang W, Song Y, He X, Xu B, Huang H, He C, et al. Prevalence and risk factors of lower urinary tract symptoms in Fuzhou Chinese women. Eur Urol. 2005; 48:309–313.
17. Foldspang A, Mommsen S. Adult female urinary incontinence and childhood bedwetting. J Urol. 1994; 152:85–88.
18. Kuh D, Cardozo L, Hardy R. Urinary incontinence in middle aged women: childhood enuresis and other lifetime risk factors in a British prospective cohort. J Epidemiol Community Health. 1999; 53:453–458.
19. Fitzgerald MP, Thom DH, Wassel-Fyr C, Subak L, Brubaker L, Van Den Eeden SK, et al. Childhood urinary symptoms predict adult overactive bladder symptoms. J Urol. 2006; 175(3 Pt 1):989–993.
20. Montaldo P, Tafuro L, Narciso V, Apicella A, Iervolino LR, Del Gado R. Correlations between enuresis in children and nocturia in mothers. Scand J Urol Nephrol. 2010; 44:101–105.
21. Yazici CM, Abali R, Tasdemir N, Dogan C, Yildiz T. Is nocturia of young adulthood a remnant of childhood nocturnal enuresis. Int Urogynecol J. 2014; 25:273–278.
22. Cornu JN, Abrams P, Chapple CR, Dmochowski RR, Lemack GE, Michel MC, et al. A contemporary assessment of nocturia: definition, epidemiology, pathophysiology, and management: a systematic review and meta-analysis. Eur Urol. 2012; 62:877–890.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download