Abstract
Purpose
To evaluate the long-term outcomes of artificial urinary sphincter (AUS) implantation and to report the complication rates, including mechanical failure, erosion, and infection.
Materials and Methods
From June 1990 to May 2011, AUS (AMS 800) implantations were performed in 56 adult males by one surgeon. Various demographic and preoperative variables, surgical variables, and postoperative outcomes, including success and complication rates with a median follow-up of 96 months, were recorded retrospectively.
Results
The mean age of the patients at the time of AUS implantation was 61.8 (±14.2) years. During the follow-up period, the total complication rate was 41.1% (23 patients). The incidence of complications was significantly lower during the follow-up period after 48 months (p<0.05). Kaplan-Meier analysis revealed that 5- and 10-year failure-free rates were 50.3% and 45.2%, respectively.
Owing to the increasing number of radical prostatectomies (RPs) as a standard treatment for localized prostate cancer, the number of men with postoperative stress urinary incontinence (SUI) has increased. The reported prevalence of urinary incontinence in all men is as high as 39% and increases with age [1], and RP is the most prevalent cause. Although the incidence of SUI decreases with the surgeon's increased experience with RP, it is still a significant problem, and reported SUI rates in these patients are between 5% and 48.0% [1].
With the proven major impact on quality of life, which affects patients' physical activity and social well-being [2,3], male SUI is an important health problem. There are several options for the surgical treatment of male SUI, including some minimally invasive technics and artificial urinary sphincter (AUS) implantation. In recent years, numerous minimally invasive treatment options (bulking agents, adjustable techniques, and several types of male slings) with different success rates have been investigated. Lack of evidence in long-term durability and efficacy is the major problem for these minimally invasive options. On the other hand, the AUS is a well-established treatment for male SUI [4,5], including that resulting from RP. Furthermore, different from the other devices, the AUS is versatile and effective for a wide range of situations, including severe incontinence, SUI after radiation, and as a salvage procedure after failure of other treatments.
In this retrospective study, we evaluated the long-term outcomes of AUS implantation in our clinic with 21 years of experience. We also report the complication rates, including mechanical failure, erosion, and infection, and the long-term durability of AUSs.
From June 1990 to May 2011, AUS (AMS 800, American Medical Systems Inc., Minnetonka, MN, USA) implantations were performed in 56 adult males by one surgeon. All of the AUS cuffs were placed at the bulbar urethra. Various demographic and preoperative variables (patient age at implantation, etiology of incontinence (post prostetctomy incontinance [PPI] or neurogenic), history of pelvic radiation, and type of prior treatment for urinary incontinence), surgical variables (the date of surgery, type of surgery [primary, secondary, or revision], and operative time), and the postoperative outcomes (social or medical continence status, complications, malfunction, months to revision if applicable, and total follow-up time in months) were collected from the patients' medical charts. Social continence was defined as continence status with the use of two or fewer pads per day. Failure was defined as that caused by any reason, such as mechanical failure, surgical revision, or removal. AUS durability was analyzed by use of Kaplan-Meier survival plots. Differences in durability according to different criteria were analyzed by using the Student t-test. p-values less than 0.05 were considered significant. SPSS ver. 17 (SPSS Inc., Chicago, IL, USA) was used for all analyses. The local institutional review board approved the study.
The mean age of the patients at the time of AUS implantation was 61.8 (±14.2) years and all of the patients were male. The median follow-up time of the patients was 96 months (range, 11 to 149 months). The clinical and concomitant comorbidities of the patients are shown in Table 1. RP was the most common indication for AUS implantation (41 patients). Neurogenic male sphincter insufficiency and transurethral resection of the prostate were the other indications with a total of 9 and 6 patients in each group, respectively. The incidence of type 2 diabetes was 28.5% and the incidence of hypertension was 48.2% in the study group.
During the follow-up period, the total complication rate was 41.1% (23 patients). The mechanical failure rate was the most common complication with a rate of 25% (14 patients). The mechanical failures were difficulty to compress the pump, breakdown of the device, and inadequate urethral compression by the balloon. The mean mechanical failure time was 33 months (±24 months). Erosion and infection were the other complications with a rate of 8.9% (5 patients) and 7.1% (4 patients), respectively. In the early postoperative period, the AUS was removed in 4 patients owing to erosion (in 1 patient) and infection (in 3 patients). We removed the AUS in 1 patient at 8 months after the operation owing to a massive scrotal abscess. The mean erosion time was 41 months (±34 months). We compared the overall complication rates during the follow-up period at intervals of 12 months (Table 2). The comparison of the complications of the 1-12 months, 13-24 months, 25-36 months, and 37-48 months periods did not demonstrate any significant differences. However, the incidence of complications was significantly lower during the follow-up period after 48 months (p<0.05). Kaplan-Meier analysis revealed that 5- and 10-year failure-free rates were 50.3% and 45.2%, respectively (Fig. 1).
Of the study group, 58.9% (33 patients) of the patients did not demonstrate any complications. Because four patients experienced removal of the device before activation of the control pump, continence was evaluated in 52 patients. The 46% (24 patients) of patients with a functioning AUS (52 patients) did not use any pads per day, and 19.2% (10 patients) used ≤2 pads per day. The social continence rate was 65.3% (34 patients).
In the present study, we reported our AUS implantation series with a long follow-up period. Although many studies have reported AUS results, not as many studies had a long-term follow-up period. Regarding the outcomes, the long-term results of operations performed with mechanical devices are important. In three studies with more than 6 years of follow-up, mechanical failure rates ranged from 25% to 61% [6-8]. Similar to these studies, our mechanical failure rate was 25%. Haab et al. [6] reported a significant decrease in the mechanical failure rate after 1987 owing to device improvements. However, the mechanical failure rate in our study, which was performed between 1990 and 2012, was similar to that of the Haab et al. study (25% for both). Therefore, we believe that this finding of Haab et al. needs to be verified with further studies. Erosion and infection rates with AUS implantation vary considerably among the studies, with reports of 4-13% and 1.3-7%, respectively, in patients with PPI [6,9-11]. Our complication rates, regarding erosion and infection, were on the high side of this range, with rates of 8.9% and 7.1%, respectively. The high complication rates of the present study may be related to the longer follow-up period of our study compared with the others. Another reason may be our clinic's status. Because ours is a tertiary center, the patient population of our clinic consists mainly of men with comorbidities. In particular, the inclusion of patients with type 2 diabetes and neurogenic patients with previous urinary instrumentation in the study population may explain the relatively high rate of complications. Indeed, the findings of a recent study with a median of 6.8 years of follow-up were similar to the present study, with an 8% erosion rate and a 5.6% infection rate [7]. In that study, Kim et al. [7] reported the overall complication rate as 37%, and mechanical failure was the most common cause. Similar to the present study, they also concluded that most events, regarding the complications, occurred in the first 48 months.
Success rates for AUS implantation are generally excellent, often between 75% and 90% [8,11]. In a report of patients with a minimum of 10 years of follow-up, a continence rate of 75% was demonstrated despite a revision rate of 80% [8]. Our social continence rate was 65.3%, which is lower than in previous studies. We think that the higher complication and lower revision rates may clarify this relatively low social continence outcome.
Owing to the small number of patients, we did not perform any statistical analyses regarding the risk factors for failure. Findings in the literature differ about the risk factors for AUS implantation failure. Pelvic radiation has been considered a potential risk factor for AUS treatment failure and complications [12-14]. Thiel et al. [15] investigated the clinical and urodynamic parameters to determine the risk factors for failure and concluded that there were no significant factors and that only older patients tended to have decreased perceived improvement. Furthermore, in a study by Kim et al. [7] using a multivariate logistic model, no significant predictive factor for failure of AUS was found . On the other hand, another study by Arai et al. [16] reported that operation time was an independent risk factor for AUS failure. Although the number of patients in the two last-mentioned studies was similar, the median follow-up times were quite different (6.8 years vs. 24.5 months). The findings of the study by Kim et al. [7], with the longer follow-up time, may be more reliable. However, the finding of Arai et al. [16] suggesting a significant learning curve effect on the treatment outcome must also be taken into consideration.
This study had several limitations. Because this was a retrospective study, there are limitations to this study's conclusions and generalizations. Limited sample size is another limitation. However, because of the long follow-up time, we think that the findings of the present study should be taken into consideration. Because AUS implantations are performed to achieve higher quality of life, assessment of outcomes of this surgery should be performed with validated questionnaires. The use of a well-validated questionnaire would provide more clinically relevant information. The lack of such a questionnaire is also a limitation of our study. Because this was a single-institution retrospective study, multi-institutional studies may provide more reliable results.
Figures and Tables
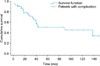 | FIG. 1Treatment failure-free survival in 64 patients with artificial urinary sphincter implantation. Five- and 10-year failure-free rates were 50.3% and 45.2%, respectively. |
References
1. Schroder A, Abrams P, Andersson KE, Artibani W, Chapple CR, Drake MJ, et al. Guidelines on urinary incontinence. In : Aus G, editor. EAU guidelines. Arnheim: European Association of Urology;2009. p. 11–28.
2. Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008; 358:1250–1261.
3. Benoit RM, Naslund MJ, Cohen JK. Complications after radical retropubic prostatectomy in the medicare population. Urology. 2000; 56:116–120.
4. Fishman IJ, Shabsigh R, Scott FB. Experience with the artificial urinary sphincter model AS800 in 148 patients. J Urol. 1989; 141:307–310.
5. Lee R, Te AE, Kaplan SA, Sandhu JS. Temporal trends in adoption of and indications for the artificial urinary sphincter. J Urol. 2009; 181:2622–2627.
6. Haab F, Trockman BA, Zimmern PE, Leach GE. Quality of life and continence assessment of the artificial urinary sphincter in men with minimum 3.5 years of followup. J Urol. 1997; 158:435–439.
7. Kim SP, Sarmast Z, Daignault S, Faerber GJ, McGuire EJ, Latini JM. Long-term durability and functional outcomes among patients with artificial urinary sphincters: a 10-year retrospective review from the University of Michigan. J Urol. 2008; 179:1912–1916.
8. Fulford SC, Sutton C, Bales G, Hickling M, Stephenson TP. The fate of the 'modern' artificial urinary sphincter with a follow-up of more than 10 years. Br J Urol. 1997; 79:713–716.
9. Gousse AE, Madjar S, Lambert MM, Fishman IJ. Artificial urinary sphincter for post-radical prostatectomy urinary incontinence: long-term subjective results. J Urol. 2001; 166:1755–1758.
10. Montague DK, Angermeier KW, Paolone DR. Long-term continence and patient satisfaction after artificial sphincter implantation for urinary incontinence after prostatectomy. J Urol. 2001; 166:547–549.
11. Elliott DS, Barrett DM. Mayo Clinic long-term analysis of the functional durability of the AMS 800 artificial urinary sphincter: a review of 323 cases. J Urol. 1998; 159:1206–1208.
12. Lai HH, Hsu EI, Teh BS, Butler EB, Boone TB. 13 years of experience with artificial urinary sphincter implantation at Baylor College of Medicine. J Urol. 2007; 177:1021–1025.
13. Trigo Rocha F, Gomes CM, Mitre AI, Arap S, Srougi M. A prospective study evaluating the efficacy of the artificial sphincter AMS 800 for the treatment of postradical prostatectomy urinary incontinence and the correlation between preoperative urodynamic and surgical outcomes. Urology. 2008; 71:85–89.
14. Walsh IK, Williams SG, Mahendra V, Nambirajan T, Stone AR. Artificial urinary sphincter implantation in the irradiated patient: safety, efficacy and satisfaction. BJU Int. 2002; 89:364–368.
15. Thiel DD, Young PR, Broderick GA, Heckman MG, Wehle MJ, Igel TC, et al. Do clinical or urodynamic parameters predict artificial urinary sphincter outcome in post-radical prostatectomy incontinence? Urology. 2007; 69:315–319.
16. Arai Y, Kaiho Y, Takei M, Nonomura K, Baba S, Habuchi T, et al. Burden of male stress urinary incontinence: a survey among urologists in Japan. Int J Urol. 2009; 16:915–917.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download