This article has been
cited by other articles in ScienceCentral.
We read with great interest the excellent paper of Ouh and colleagues [
1] on the prevalence of human papillomavirus (HPV) genotypes and precancerous cervical lesions in a screening population in the Republic of Korea.
Distribution of HPV genotypes is a keen issue in the identification of high risk genotypes. In the international scientific literature, there are several reports describing HPV genotype distributions [
2]. The findings of Ouh and colleagues [
1] are consistent with the results of other studies. However, limited information is available on the occurrence frequency or prevalence of HPV infection within the general population.
Within the Hungarian organized cervical cancer screening program, which was implemented in 2003 [
3456], a pilot program was introduced in 2013 for the involvement of health visitors. It meant that in addition to gynecologists, health visitors, having a B.Sc. degree in health sciences, were allowed to take the smears. The aim of this pilot was to increase the participation rate of women attending the screening program [
78910].
Within this Hungarian health visitor based pilot program, the smears were tested and evaluated for the presence of HPV. In the screening period, the call-in rate was 32.45% (301,830 out of 930,058 women) nationally, with the compliance of 8.26% (24,926 out of 301,830 invited women). The occurrence of any positive result was 1.85% (461 out of 24,926 tests) nationally. We found 113 HPV positive cases from 24,926 women participating in the screening program, thus the frequency of HPV was 0.45 which equals a prevalence of 37.44/100,000 persons.
The prevalence of HPV in Hungary proved to be lower than those of in the Republic of Korea (16.7%) reported by Ouh and colleagues (
Table 1) [
1]. Ouh and colleagues [
1] examined 18,170 women aged 17 to 83 years; they underwent HPV genotyping and conventional cervical cytology. Hungarian health visitors conducted a pilot program, in which 24,926 women aged 25 to 65 years were examined. The different age group of the target population might explain a part of differences in prevalence in the Korean and Hungarian study.
Bruni and colleagues [
11] reported in their meta-analysis, that “the estimated global HPV prevalence was 11.7% (95% confidence interval, 11.6%–11.7%). Sub-Saharan Africa (24.0%), Eastern Europe (21.4%), and Latin America (16.1%) showed the highest prevalence.”
In European region, there is a large variability between programs in the organization of smear taking. In Ireland, Netherland, and United Kingdom general practitioners, physician associates take sample for cervical screening. In Sweden, Spain, Poland, and Estonia midwives take sample as well. Nurses in Malta, nurses and midwives in Finland and Greece, health visitors in Hungary are involved in performing of screening [
1213].
Korean guideline recommends in asymptomatic women aged over 20 to be begun cervical cancer screening with Pap smear or liquid-based cytology every 3 years until the age of 74 when 3-consecutive cytology shows negative results within ten years. The combined test (cervical cytology and HPV DNA test) is alternatively recommended after taking into account clinical decision and individual risk or preference [
14].
However, the U.S. Preventive Services Task Force does not recommend screening for cervical cancer in women who are younger than 21 years old and screening for cervical cancer with HPV testing, alone or in combination with cytology, as well as in women who are younger than 30 years old [
15].
The European Guideline concluded that “Primary testing for oncogenic HPV can be used in an organized, population-based program for cervical cancer screening” and “Only one primary test (either cytology or testing for oncogenic HPV) should be used at any given age in cervical cancer screening” [
16].
Further consideration of HPV screening as a first line screening method for cervical cancer is an important health policy issue in many countries.
Figures and Tables
Table 1
Results of the Hungarian pilot program for cervical cancer screening by health visitors (2013–2015)
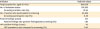
|
Indicator |
National values |
|
Target population; aged 25–65 yr |
930,058 |
|
No. of invitation letters |
301,830 |
|
Screening invitation rate (%) |
32.45 |
|
No. of women who participated in screening |
24,926 |
|
Screening participation rate (%) |
8.26 |
|
Positive findings (cases) |
461 |
|
Positive findings rate (positive findings/total screening) (%) |
1.85 |
|
HPV positive findings (cases) |
113 |
|
HPV prevalence rate compared to screening (%) |
0.45 |