INTRODUCTION
Cervical cancer (CC) is currently the fourth most common malignant disease of women worldwide; according to GLOBOCAN series of the International Agency for Research on Cancer, an estimated 560,505 new cases of CC were diagnosed in 2012, and approximately 285,000 deaths due to this type of tumor were recorded during the same period [
1].
Surgical treatment, including radical hysterectomy (RH) with or without bilateral salpingo-oophorectomy and pelvic lymphadenectomy +/− para-aortic lymphadenectomy, is the gold standard for women with early stage CC. Furthermore, although radio-chemotherapy represents the standard of care for patients affected by locally advanced cervical cancer (LACC), neoadjuvant chemotherapy (NACT) followed by radical surgery represents a safe alternative [
2].
Ideally, surgical treatment of CC should guarantee maximal oncological disease control while minimizing early and late morbidity. Since the first description of the RH by Wertheim in 1898, several technical modifications have been developed with the aim of decreasing the rate of intra-operative complications and postoperative pelvic dysfunctions. In this scenario, the concept of preservation of autonomic nerves during RH has become the standard in many gynecological oncologic centers [
3]. Nerve-sparing radical hysterectomy (NSRH) was firstly introduced and subsequently sharpened by the Japanese school [
45]. Available studies have shown the benefits of NSRH in terms of functional outcomes (bladder, bowel, and sexual function) [
678], while weaker evidence is available on the oncologic outcomes of this surgical procedure. In fact, a recent systematic review underlines that most of the trials lacked a control group, had small sample size, and had short follow-up intervals [
9].
Therefore, the current retrospective study compared the effectiveness and safety of NSRH with conventional RH in a relatively large number of the patients of CC patients undergoing either primary surgery or NACT followed by surgery.
MATERIALS AND METHODS
A large institutional prospectively collected database, including CC patients between 1980 and 1995, and between 2001 and 2015 was retrospectively reviewed, searching records of women who underwent either primary radical surgery or NACT followed by radical surgery. The patients submitted to surgery between 1996 and 2000 were not considered in this study because in this period, according to protocol, we did not perform type III RH. All patients gave consent for the use of personal information for health research. The Institutional Review Board (IRB) of National Cancer Institute – Milan approved this study (approval number: INT-006812).
Inclusion criteria were histologically diagnosed CC, type C (both C
1 and C
2) RH according to Querleu-Morrow classification [
10], and age more than 18 years.
Exclusion criteria were: other metachronous or synchronous neoplasia; history of preoperative urinary, intestinal, or sexual dysfunctions; presence of other severe comorbidities; previous pelvic surgery (all but cesarean section); presence of psychiatric disease or any condition precluding the acquisition of written informed consent.
For the purposes of the study, patients were distinguished in 2 groups: women undergoing type C1 NSRH and those undergoing conventional type C2 RH.
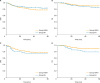
The primary outcome of this study was to evaluate the 5-year oncologic outcomes, disease-free survival (DFS) and overall survival (OS) between the study groups. Secondary outcome was to compare the rate and the type of recurrences rate. Tertiary outcome was to assess the rate of early and late complications/dysfunctions between the study groups.
Patients were preoperatively assessed with complete physical and gynecologic examination, routine blood and urine analysis, chest radiograph, and magnetic resonance imaging. Cystoscopy, rectoscopy, or computed tomography was performed only when clinically indicated. The stage of the disease was determined by the International Federation of Gynecology and Obstetrics (FIGO) staging system [
11].
NACT consisted in 3 to 4 cycles of platinum-based chemotherapy. Since 2001, all patients with FIGO stage IB2, IIA2 and IIB underwent NACT. All patients included in the study underwent radical surgery including RH with or without bilateral salpingo-oophorectomy and pelvic lymphadenectomy +/− para-aortic lymphadenectomy. Type C
1 RH was performed as previously described [
121314]. Two experienced surgeons (more than 500 radical hysterectomies performed) in gynecologic oncology (F.R. and A.D.) performed all surgical procedures.
Pelvic lymphadenectomy consisted of total removal of all lymph fatty tissue around pelvic vessels and obturator fossae. Para-aortic lymphadenectomy was performed only when pelvic lymph node was positive for the presence of metastases in the iliac area on frozen section.
Pathologic evaluation included histological type, depth of cervical stromal infiltration, infiltration of parametrium and resection margins, vaginal involvement, lymph vascular space invasion (LVSI), tumor diameter, number of pelvic lymph nodes, and number of lymph node metastases.
In group RH, in case of positive lymph nodes, parametrial or/and vaginal involvement, or positive surgical resection margins (<5 mm), presence of at least 2 cervical risk factors after RH according to Sedlis criteria [
15], patients underwent adjuvant radiotherapy, whereas, the presence of LVSI alone was not considered sufficient to receive adjuvant therapy. In group NSRH, in case of positive lymph nodes, parametrial or/and vaginal involvement, or positive surgical resection margins (<5 mm) patients underwent adjuvant radiotherapy. In the RH group, according to that period's protocol, all patients were submitted to adjuvant brachytherapy.
Recurrences were diagnosed during regular follow-up visits and confirmed by computed tomographic and/or magnetic resonance imaging scans. Whenever possible, histologic or cytologic confirmation was obtained. Local recurrences were defined as vaginal recurrences, pelvic recurrences, or pelvic lymph node metastases.
The following medical, perioperative and pathologic information were obtained from the database review: age, body mass index (BMI), parity, operative time, estimated blood loss, intraoperative complications, number of perioperative blood transfusions, hospital stay, early and late postoperative complications, pain evaluation using a visual analogue scale, resumption of bladder function (day of urinary catheter removal with urinary residual <100 cc after first spontaneous micturition), FIGO stage, histopathologic subtype, number and disease status of lymph nodes removed, follow-up time, DFS, OS, and locoregional recurrence (LRR). For OS, event times were computed as the interval between the date of surgery and the date of death for any cause, with censoring at the date of last follow-up for alive patients. For DFS, event times were computed as the interval between the date of surgery and the date of first relapse or death for any cause, with censoring at the date of last follow-up for event-free subjects. For LRR, event times were computed as the interval between the date of surgery and the date of local relapse as first event, censoring at the date of last follow-up for event-free patients, and considering as competing events vaginal relapse, distant relapse, and death, whichever occurred first. Post-operative complications were arbitrarily distinguished in early (those occurring in a period of time ≤60 days) and late (those occurring in a period of time >60 days) complications.
1. Statistical analysis
Data are summarized using basic descriptive statistics. The normal distribution of continuous variable data was evaluated with the Kolmogorov-Smirnov test. Categorical variables were analyzed using the χ2 test. Continuous variables, before and after treatment, were analyzed by using the paired t-test and the Wilcoxon rank sum test accordingly to data distribution.
Survival outcomes were evaluated with both Kaplan-Meier and Cox models. Hazard ratio (HR) and 95% confidence intervals (CIs) were calculated for each comparison. Univariate and multivariate analysis were performed when appropriate. All covariates with a p value less than 0.20, based on univariate analysis were included in the multivariate model. All p values were 2-sided. Statistical analysis was performed using GraphPad Prism version 6.0 for Mac (GraphPad Software, San Diego, CA, USA) and IBM-Microsoft SPSS version 20.0 for Mac (SPSS Science, Chicago, IL, USA). The p values <0.05 were statistically significant.
DISCUSSION
The current study investigated the effectiveness and safety of NSRH with RH in a relatively large number of the patients of CC patients undergoing either primary surgery or NACT followed by surgery. It was reported no difference in 5-year OS was significantly between RH and NSRH groups, while 5-year DFS was superior in RH group compared with NSRH group. However, this finding is not surprising due to the higher number of patients of NSRH group with LACC and treated with NACT, and to the larger use of adjuvant radiotherapy in NSRH group. In fact, when considering only patients receiving NACT no difference in both 5-year DFS and OS was reported. Interestingly, while no difference has been reported in the rate of early complications between 2 study groups, a higher number of late complications was experienced by patients of RH group, mainly due to lymphatic complications or intestinal ileus. Patients belonging to this group were operated in an older period of time compared with patients of NSRH group; therefore, the use of vascular clips and energy coagulation was superior in NSRH group and this may justify the higher number of lymphatic complications in RH group. In addition, it is well known that the autonomic nerves innervate the bowel and that the damage to these nerves in the pelvis can lead to diarrhoea or constipation [
121617], thus explaining why more patients experienced impaired bowel function in RH group.
Different trials have compared class II RH with class III NSRH showing similar results in terms of bladder function, quality of life, and oncological outcomes. However, only few studies have investigated the outcomes of type C
1 NSRH compared with conventional type C
2 RH in the treatment of CC [
1418]. Our previous research included a total of 496 patients, of whom 185 patients were treated with type C
1 NSRH and 311 patients with type C
2 RH with a median follow-up of 93 months (42 and 159 months for the NSRH and RH groups, respectively). This study demonstrated that the oncologic results and relapse rates were comparable between the 2 study groups. Bladder function and postoperative complications rate were significantly better in the NSRH than in RH group [
14]. These findings are confirmed by the current study, which was conducted in a substantially enlarged study population, supporting the role of nerve-sparing technique. More recently a randomized controlled trial (RCT) was conducted to evaluate the efficacy of type C
1 NSRH in preserving bladder function and its oncologic safety in the treatment of CC. Ninety-two patients with CC stage IA2 to IIA were randomized to surgical treatment with type C
2 RH (N=44) or type C
1 NSRH (n=48), and 86 patients finally included in the analysis. This trial demonstrated no difference in 10-year DFS between the RH group (94.9%) and NSRH group (92.4%). Furthermore, volume of residual urine and bladder compliance were significantly deteriorated at 12 months after RH, while all parameters of urodynamic study were recovered no later than 3 months after NSRH. This study is the only available RCT investigating the issue of type C
1 NSRH versus conventional type C
2 RH. However, from a merely statistical point of view, it is significantly underpowered to assess oncologic outcomes. Indeed, a recent systematic review on this issue by Basaran and colleagues [
9] has been underlined this concept. In their paper, the Authors calculated that the number of patients needed to prove non-inferiority of NSRH to RH with regard to recurrence would be between 4,300 and 1,000 depending on the expected risk of recurrence (5% and 20%, respectively) [
9]. In this view, we deem that our study provides important data due to the large number of patients included; however, we acknowledge that the main limitations of the current work are represented by the inherent biases of the retrospective, single centre study design. Another limitation of this study is that standardized questionnaires and/or urodynamic study were not used to evaluate bladder function before and after surgery, thus limiting the assessment of this specific outcome. Finally, the significant difference in length of follow-up between the two study groups prevents us to show the long-term follow-up (10 years) of the patients.
In conclusion, this study supports the efficacy and safety of NSRH for the treatment of CC patients. NSRH seems superior to RH, NSRH correlates with lower morbidity rate and similar oncologic outcomes than RH. Although the retrospective design of the study, we deem that our findings may be useful to provide a more detailed preoperative and postoperative counselling to the patients. However, well-designed, large-scale prospective non-inferiority trials are strongly required to confirm these results.








 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download