To the Editor,
In the United States, ovarian carcinoma remains the most deadly gynecologic malignancy, and approximately 14,000 deaths are projected from the disease in 2017 [
1]. Ovarian carcinoma comprises various histologic subtypes based on the cell of origin, with serous carcinoma being the most common subtype. Serous ovarian carcinomas are commonly grouped into 2 types based on histologic characteristics (high-grade and low-grade) [
23]. Mounting evidence has shown that low-grade serous ovarian carcinoma (LGSOC) has distinct clinical and molecular differences from high-grade serous ovarian carcinoma (HGSOC) [
45]. Unlike HGSOC, LGSOC is considered a rare tumor and has been understudied due to its low incidence. To date, there have been no population-based reports of LGSOC statistical trends. The objective of our study was to examine the temporal changes in the proportion of LGSOC among women with epithelial ovarian cancer.
This retrospective observational study examined data from the National Cancer Institute, Surveillance, Epidemiology, and End Results (SEER) program between 1973 and 2013. The SEER database is the largest tumor registry in the United States covering approximately 28% of the US population. The SEER data are publicly available and de-identified. The University of Southern California Institutional Review Board exempted this study. SEER*Stat 8.3.2 (IMS Inc., Calverton, MD, USA) was used to extract the SEER 18 cases, generating the dataset from “Ovary” limited to malignancy and female sex. Primary invasive epithelial ovarian cancer was eligible for analysis, and the International Classification of Diseases for Oncology, Third Edition (ICD-O-3) site/histology validation and World Health Organization histological classification codes were used for identifying serous ovarian cancer cases as previously described [
6].
In our study, tumor grade was combined with histology types, and serous ovarian carcinomas that were designated as well-differentiated tumors (grade 1) were considered LGSOC whereas moderately-differentiated (grade 2) and poorly-differentiated (grade 3) tumors were considered HGSOC. This classification is based on the rationale that historical grade 1 tumors correlate with LGSOC and grade 3 tumors correlate with HGSOC in the 2-tier system [
3]. In addition, moderately-differentiated (grade 2) tumors were grouped as HGSOC in this study as the majority of this group are generally high-grade tumors.
A time-specific proportion of LGSOC across the study period was examined among all epithelial type ovarian carcinomas and all serous ovarian carcinomas (any grade). The Joinpoint Regression Program 4.2.0.2 (National Cancer Institute, Bethesda, MD, USA) was used to model temporal trends as a function of calendar year using a piecewise linear regression following log transformation, and annual percent change (APC) was estimated with 95% confidence interval (CI). All statistical analyses were 2-sided, and a p-value of less than 0.05 was considered statically significant.
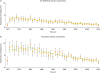
We identified 2,617 cases of LGSOC during the study period. This represented 2.05% (95% CI=1.98, 2.13) of all epithelial ovarian carcinomas (n=127,476). The year-trend of proportion of LGSOC among all epithelial ovarian carcinomas is shown in
Fig. 1A. Between 1975 and 2013, there was a significant decrease in the proportion of LGSOC among all epithelial ovarian carcinomas (APC=−3.06; 95% CI=−3.47, −2.64; p<0.001). In the years 1975 and 2013, the proportions of LGSOC among all epithelial ovarian carcinomas were 3.64% and 1.02%, respectively.
LGSOC represented 4.66% (95% CI=4.49, 4.84) of serous ovarian carcinomas (n=56,117). The year-trend of proportion of LGSOC among serous ovarian carcinomas is shown in
Fig. 1B. Between 1983 and 2013, there was a significant decrease in proportion of LGSOC among serous ovarian carcinomas (APC=−3.51; 95% CI=−4.15, −2.87; p<0.001). In the years 1983 and 2013, the proportions of LGSOC among all serous ovarian carcinomas were 9.60% and 2.23%, respectively.
Stage-specific trends of the proportion of LGSOC were examined (stage I–II cases for early-stage disease; and stage III–IV cases for advanced-stage disease). Among cases with early-stage disease, there was a significant decrease in the proportion of LGSOC among all epithelial ovarian carcinomas (APC=−3.97; 95% CI=−4.59, −3.35; p<0.001) between 1977 and 2013 as well as serous ovarian carcinomas (APC=−3.46; 95% CI=−4.28, −2.63; p<0.001) between 1983 and 2013. Similarly, among advanced-stage disease, the proportion of LGSOC has significantly decreased among all epithelial ovarian carcinomas (APC=−3.01; 95% CI=−3.72, −2.30; p<0.001) and among serous ovarian carcinomas (APC=−3.72; 95% CI=−4.41, −3.01; p<0.001) between 1983 and 2013.
We observed that the proportion of LGSOC has been steadily decreasing over the past few decades in the United States. These findings were consistent in the whole cohort of epithelial ovarian carcinoma and in the cohort for serous histology. Moreover, we found that the proportion of LGSOC has decreased in both early- and advanced-stage disease.
A decreasing trend of the proportion of LGSOC demonstrated in this study is in contrast to the increasing trend of borderline ovarian tumors (BOTs) seen over this time period [
7]. Specifically, a previous population-based study found that the proportion of BOTs among all epithelial ovarian carcinomas has been increasing from 8.3% to 23.6% between the 1960s and 2000s [
8]. In addition, their study reported that the population-based incidence of BOTs has increased during the same period [
8]. Another nation-wide cohort study demonstrated similar findings in that the incidence of BOTs has increased in the past decades with a greater increase in serous BOTs as compared to mucinous types [
9].
There are multiple plausible explanations for these findings, including that there have been changes in diagnostic criteria of BOTs and LGSOC, the more recent recognition of the significance of LGSOC, and increases in the early detection of precursor ovarian neoplasms.
First, approximately 4 decades ago, when the SEER database was launched, BOTs were included as a separate entity in its classification and staging system of gynecologic malignancies by the International Federation of Gynecology and Obstetrics (FIGO) [
10]. We speculate that serous BOTs were likely diagnosed as well-differentiated serous ovarian carcinomas prior to their recognition as a separate clinical entity. Even after integration of the BOT classification into the FIGO system, changes in the practice pattern for histopathology diagnosis would not have been immediate, and certain serous BOTs would continue to be diagnosed as serous ovarian carcinomas for years following the addition of the new classification. Misclassification of serous BOTs as serous ovarian carcinoma in the early years of the study population is likely the cause of the higher proportion of LGSOC in the 1970 to 1980s.
Second, the concept of LGSOC is relatively new, and it is possible that pathologists have recently been stricter in diagnosing LGSOC. In our study, central pathology review to confirm LGSOC was not available, and we recognize that this may have affected our results. Thus, some of LGSOC cases may have also been misclassified as moderately-differentiated (grade 2) serous ovarian carcinoma.
Third, epithelial ovarian cancer, particularly HGSOC, is generally a disease of the elderly, whereas the average age of women with LGSOC is approximately 20 years younger [
45]. Furthermore, the U.S. population has significantly aged over the past few decades. Thus, a relative increase in HGSOC as compared to LGSOC may have resulted in a relative decrease in the proportion of LGSOC.
Lastly, early detection of precursor lesions of invasive ovarian cancer is suggested by the increased incidence of BOTs [
89]. This can be particularly applicable to mucinous BOTs in relation to invasive mucinous ovarian cancer, but it remains unknown if the increase in the incidence of serous BOTs results in a decrease in LGSOC. Some serous BOTs and LGSOC share genetic similarity [
11], and thus, it may be speculated that increasing the detection of serous BOTs, a precursor form of LGSOC, results in a decrease in LGSOC. Further study to test this hypothesis is warranted.
In summary, our study suggests that LGSOC may have become less common in the United States accounting for only small percent of all serous ovarian carcinomas in recent years. These statistics can be applicable to care of patients with LGSOC. That is, the histopathologic diagnosis of LGSOC may benefit from centralized review by experienced gynecologic pathologists given that this clinical entity may not be common in general practice. Both serous BOTs and moderately-differentiated (grade 2) serous ovarian carcinomas would likely benefit most from expert review. Proper diagnosis of LGSOC is of paramount importance for grade 2 lesions because treatment choice for LGSOC is largely different from HGSOC. In addition, the rarity of LGSOC may impact clinical trials for novel therapeutics, particularly in the randomized setting. The low incidence of LGSOC could limit patient accrual of this type of study, and centralizing institutions for clinical trials for LGSOC may be necessary.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download